My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.2 Madrid Feb. 2014
https://dx.doi.org/10.4321/S1130-01082014000200016
Ulcerative colitis and isotretinoin: Is there a causal relationship?
Colitis ulcerosa e isotretinoína, ¿existe una relación causal?
Key words: Isotretinoin. Inflammatory bowel disease. Ulcerative colitis.
Palabras clave: Isotretinoína. Enfermedad inflamatoria intestinal. Colitis ulcerosa.
Dear Editor,
We are reporting the case of a 39-year-old woman without toxic habits and with a history of mild mitral valve prolapsed that, after treatment of acne with dermatologist prescribed isotretinoin, consulted because of an increase in the number of bowel movements and bright red blood rectal bleeding after defecating without accompanying anal symptoms.
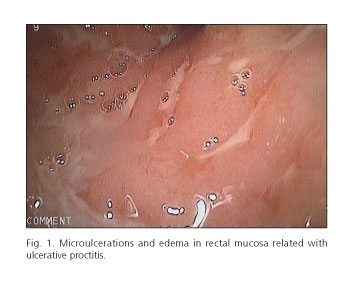
The analytical study was normal and a colonoscopy was performed. Signs of inflammation were found in the distal 10cm of rectal mucosal and had an erythematous and granular appearance with effacement of the submucosal vascular pattern and non-confluent micro-ulcers. All of this is suggestive of ulcerative proctitis (Fig. 1). The histological study showed an alteration in the glandular architecture with a reduction of goblet cells without observing crypt abscesses and with dense inflammatory infiltrate of plasma cells in the lamina propria.
The patient was treated with topical mesalazine via suppository, initially at a dosage of 1g/12h and dosage was subsequently continued at 1g/24h. There was a clinical response; cessation of rectal bleeding and intestinal rhythm normalisation was observed.
In the three years that the patient has continued follow up at our office, she has shown isolated outbreaks that have been controlled with topical mesalazine treatment, as needed.
Discussion
Some medications have been suggested as the cause or trigger of outbreaks in patients with inflammatory bowel disease (IBD) (1-3). Isotretinoin is a vitamin A analogue indicated in serious acne and whose use has been seen as being involved in the development of IBD (4-7), although information to this regard is not yet clear. In 1986, the first report of a case of a 26-year old woman who had proctitis during isotretinoin treatment and improved upon withdrawal from this medication was published. Other cases and clinical series (5-7) have been reported since this time. However, the most recent case-control studies do not seem to confirm isotretinoin as having a relevant role in the evolution of IBD. Etminan et al. carried out a case-control study with 45,339women undergoing oral contraceptive without finding an association between the use of isotretinoin with ulcerative colitis (RR: 0.9, IC 95%, 0.52-1.90) or with Crohn's disease (RR: 0.91, IC 95%, 0.37-2.25), concluding that this medication does not increase the risk of IBD (8). Alhusayen et al. did not find an association with IBD evolution either when carrying out a retrospective population-based cohort including 46,922patients treated with isotretinoin (RR 1,14; IC 95 %, 0.92-1.41) (9).
In conclusion, to date, causal relationship between isotretinoin and IBD cannot be definitively established. However, this fact should be taken into account when considering treatment with isotretinoin in patients that have IBD diagnosis and those patients with risk factors for developing this illness.
Rogger Álvaro Bendezú-García, Álvaro Hernández-Martínez,
Gustavo Óliver Patrón-Román, Francisco Bravo-Castillo
and José Luis Vega-Sáenz
Department of Gastroenterology. Hospital Torrecárdenas.
Almería, Spain
References
1. Card T, Logan RF, Rodrigues LC, Wheeler JG. Antibiotic use and the development of Crohn's disease. Gut 2004;53:246-50. [ Links ]
2. Evans JM, McMahon AD, Murray FE, McDevitt DG, MacDonald TM. Nonsteroidal anti-inflammatory drugs are associated with emergency admission to hospital for colitis due to inflammatory bowel disease. Gut 1997;40:619-22. [ Links ]
3. Godet PG, May GR, Sutherland LR. Meta-analysis of the role of oral contraceptive agents in inflammatory bowel disease. Gut 1995;37:668-73. [ Links ]
4. Brodin MB. Inflammatory bowel disease and isotretinoin. J Am Acad Dermatol 1986;14:843. [ Links ]
5. Reniers DE, Howard JM. Isotretinoin-induced inflammatory bowel disease in an adolescent. Ann Pharmacother 2001;35:1214-6. [ Links ]
6. Rolanda C, Macedo G. Isotretinoin and inflammatory bowel disease. Am J Gastroenterol 2007;102:1330. [ Links ]
7. Spada C, Riccioni ME, Marchese M, Familiari P, Costamagna G. Isotretinoin-associated pan-enteritis. J Clin Gastroenterol 2008;42:923-5. [ Links ]
8. Etminan M, Bird ST, Delaney JA, Bressler B, Brophy JM. Isotretinoin and risk for inflammatory bowel disease: a nested case-control study and meta-analysis of published and unpublished data. JAMA Dermatol 2013;149:216-20. [ Links ]
9. Alhusayen RO, Juurlink DN, Mamdani MM, Morrow RL, Shear NH, Dormuth CR. Isotretinoin use and the risk of inflammatory bowel disease: A population-based cohort study. J Invest Dermatol 2013;133:907-12. [ Links ]











 text in
text in