My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.2 Madrid Feb. 2014
https://dx.doi.org/10.4321/S1130-01082014000200017
Conservative management of isolated dissection of the superior mesenteric artery
Manejo conservador en la disección aislada de arteria mesentérica superior
Key words: Isolated disection. Superior mesenteric artery. Treatment.
Palabras clave: Disección aislada. Arteria mesentérica superior. Tratamiento.
Dear Editor,
Isolated dissection of the superior mesenteric artery (IDSMA) is an uncommon disease. Its incidence has increased due to the increased use of multislice imaging tests. It is a potentially treatable cause of mesenteric ischemia and the optimal treatment is still a controversial issue.
Case report
A 46-year-old man with a previous history of smoking (20 cig./day) was referred because of recurrent episodes of sudden high periumbilical abdominal pain. Upon examination, pain in the periumbilical region was found without peritoneal irritation sings. Blood pressure raised to 180/71mm Hg. Hemogram, biochemistry, and venous blood gas analysis were strictly normal.
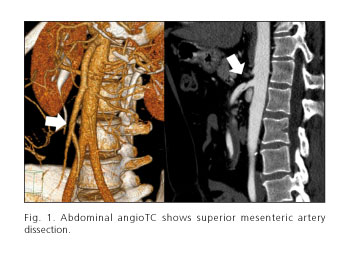
On abdominal angio-TC (Fig. 1), a low signal lineal image is detected inside superior mesenteric artery lumen, compatible with dissection, with good distal flow and good distal perfusion. Allother vascular structures were normal.
The patient was transferred to intensive care unit (ICU) and anticoagulant (bemiparine 7.500U each 24hours), antihypertensive, and analgesic treatment was initiated. Pain events eased up progressively and oral tolerance was initiated uneventfully.
As clinical stability, absence of bowel ischemia and good flow distal to SMA dissection were established, we decided to continue with conservative management and not accomplish therapeutic interventionist measures.
The patient was released from hospital after 12days. Anticoagulant treatment was maintained for a month, continuing with acetylsalicylic acid 100mg each 24hours. Blood pressure was suitably controlled with enalapril 10mg each 24hours. After a 2years follow-up the patient is clinically stable and asymptomatic, with control imaging tests without changes.
Discussion
IDSMA is an uncommon disease. According to the angiographic finds it can be classified in:
-Type I: Patent true and false lumen revealing entry and re-entry sites.
-Type II: Patent true and false lumen without re-entry.
-Type IIb: Patent true lumen but thrombosed false lumen.
-Type III: Superior mesenteric artery (SMA) occlusion.
The majority of cases evolve satisfactorily with conservative management and a minority of them present uncontrollable abdominal pain and bowel ischemia that may require surgical or revascularization treatment.
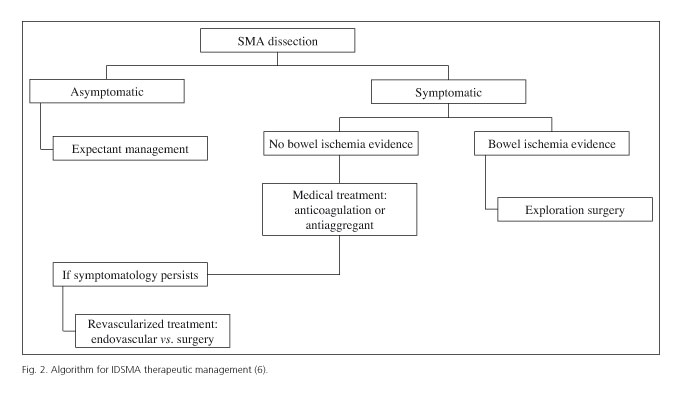
Recent trials have proposed a therapeutic algorithm for IDSMA based on published cases (2-6). To summarize (Fig. 2):
1. In asymptomatic patients, with incidental finding of IDSMA, conservative management is recommended.
2. In symptomatic patients without evidence of bowel ischemia, medical treatment is the first therapeutic option, either with anticoagulation or antiaggregants and blood pressure and pain control. Anticoagulant treatment is preferred by some authors in order to avoid the thrombosis of distal vessels with deficient perfusion. Nevertheless, no evidence of significant difference between anticoagulation or antiaggregant treatment has been shown.
3. Symptomatic patients without evidence of bowel ischemia with medical treatment, in whom intense abdominal pain or diet intolerance persists, surgery or endovascular treatment may be a good alternative.
4. In symptomatic patients, with radiologic signs or clinical suspicion of bowel ischemia, surgical exploration of abdominal cavity and intestinal revascularization are mandatory.
Francisco Javier Moreno-Machuca, Guillermo Núñez-de-Arenas-Baeza,
Francisco Diéguez-Rascón, José Enrique López-Lafuente,
Jorge Haurie-Girelli and José Vicente González-Herráez
Hospital Universitario Nuestra Señora de Valme. Sevilla, Spain
References
1. Chu SY, Hsu MY, Chen CM, Yeow KM, Hung CF, Su IH, et al. Endovascular repair of spontaneous isolated dissection of the superior mesenteric artery. Clinical Radiology 2012;67:32-7. [ Links ]
2. Park YJ, Park KB, Kim DI, Do YS, Kim DK, Kim YW. Natural history of spontaneous isolated superior mesenteric artery dissection derived from follow-up after conservative treatment. J Vasc Surg 2011;54:1727-33. [ Links ]
3. Min SI, Yoon KC, Min SK, Ahn SH, Jae HJ, Chung JW, et al. Current strategy for the treatment of symptomatic spontaneous isolated dissection of superior mesenteric artery. J Vasc Surg 2011;54:461-6. [ Links ]
4. Yun WS, Kim YW, Park KB, Cho SK, Do YS, Lee KB, et al. Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissection. Eur J Vasc Endovasc Surg 2009;37:572-7. [ Links ]
5. Cho BS, Lee MS, Lee MK, Choi YJ, Kim CN, Kang YJa, et al. Treatment guidelines for isolated dissection of the superior mesenteric artery based on follow-up CT findings. Eur J Vasc Endovasc Surg 2011;41:780-5. [ Links ]
6. Carter R, O'Keeffe S, Minion DJ, Sorial EE, Endean ED, Xenos ES. Spontaneous superior mesenteric artery dissection: Report of 2 patients and review of management recommendations. Vasc Endovascular Surg 2011;45:295-8. [ Links ]











 text in
text in