Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.3 Madrid mar. 2014
SPECIAL ARTICLE
Sedation for gastrointestinal endoscopy. Clinical practice guidelines of the Sociedad Española de Endoscopia Digestiva
Sedación en endoscopia digestiva. Guía de práctica clínica de la Sociedad Española de Endoscopia Digestiva
Francisco Igea, Juan Antonio Casellas, Ferrán González-Huix, Cristina Gómez-Oliva, Juan Salvador Baudet, Guillermo Cacho, Miguel Ángel Simón, Emilio de-la-Morena, Alfredo Lucendo, Francesc Vida and Leopoldo López-Rosés
Sociedad Española de Endoscopia Digestiva
Introduction
Sedation for gastrointestinal endoscopic procedures has become indispensable, hence sedation is now a mandatory requirement to be offered to all patients before an endoscopic exam following the discussion of its benefits, risks, drawbacks, and alternative options. Patient sedation pursues a dual purpose -on the one hand the achievement of a good perceived quality by suppressing pain; on the other hand an avoidance of untimely movements that may compromise efficacy and safety. In the past twenty years a huge amount of papers were published showing that properly trained non-anesthetist doctors and nurses may effectively, safely, and efficiently take responsibility for the administration of sedatives and painkillers, as well as patient monitoring during endoscopy. Also, major scientific societies involved in gastrointestinal endoscopy have published guidelines with recommendations in this respect. The Sociedad Española de Endoscopia Digestiva (SEED) is no exception and published in 2006 their sedation guidelines, which included all major indications, contraindications, drug classes, and other related topics (1). Presently, the SEED Board of Directors has decided to update these guidelines by publishing a new version with revised major aspects and the addition of recent findings.
Guidelines development approach
Cooperation was requested from a number of endoscopists experienced and interested in sedation at various hospitals throughout Spain. Following the development of a table of contents, each one of them drafted a chapter based on an updated literature revision, including evidence-based recommendations in accordance with the SIGN classification at the end (2). Each initial draft was reviewed by all authors, and corrections deemed relevant were incorporated in order to provide a definitive edition. The notion behind the development of these guidelines was to obtain a concise, clear text with scientific rigor and readily applicable to clinical practice.
Sedation goals. Sedation levels
The goals of sedation and analgesia include decreasing anxiety, relieving discomfort and pain, and reducing the memory of endoscopic procedures (3,4). Sedation levels should be adjusted to each individual's needs and each procedure to ensure safety, comfort, and technical success.
Sedation levels entail a continuum of states ranging from minimal sedation or anxiolysis to general anesthesia (Table I):
- Minimal sedation or anxiolysis: A drug-induced state during which patients respond normally to verbal commands. While cognition and coordination may have functional alterations, ventilation and cardiovascular functioning are usually preserved.
- Moderate or superficial sedation: A drug-induced depression of conscience during which patients respond correctly to verbal commands and mild tactile stimulation. No intervention is necessary to maintain airway permeability, and spontaneous ventilation is adequate. Cardiovascular functioning is usually preserved.
- Deep sedation: A drug-induced depression of conscience during which patients cannot be easily awakened but respond to repeated or painful stimuli. The ability to maintain ventilation independently may be impaired. Patients may need help to keep their airway permeable, and spontaneous ventilation may be inadequate. Cardiovascular function is usually preserved.
- General anesthesia: This involves a drug-induced loss of conscience in which patients do not respond to stimuli. The ability to maintain ventilation independently is often impaired. Patients usually require help to keep their airway permeable, and positive-pressure ventilation may be needed when spontaneous breathing or neuromuscular function is depressed. Cardiovascular function may become impaired (4).
- Dosis titration and pharmacological variability: A well-known, key principle in sedative administration is that drugs must be administered in escalated doses -effects being assessed at each step- until the desired action is achieved. While certain patient characteristics may help predict the required dose for adequate sedation (e.g., age, comorbidity, body mass, race, response to prior sedation or concurrent use of oral narcotics or benzodiazepines), the precise dose that will be needed for any given patient is impossible to foretell with accuracy. This is due to the fact that response to sedatives in individual patients is variable. For instance, blood drug levels may show up to five-fold differences in age-matched patients receiving identical doses. Also, even if blood drug levels are similar, the perceived experiences of patients may differ a lot (3).
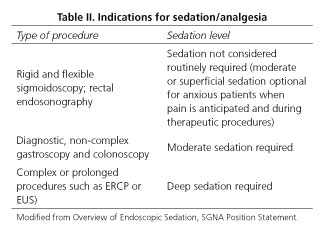
For a given exploration type required sedation levels may vary from one patient to the next. In addition, one patient may require different sedation levels within a given procedure. For instance, a patient undergoing colonoscopy may experience more pain and require more sedation at certain points during an examination. In prolonged or complex procedures, or under other circumstances, deep sedation or even anesthesia may be required. However, basic, routine endoscopic gastrointestinal procedures may be performed with moderate sedation (5) (Table II).
Different studies have shown that in basic endoscopic procedures superficial sedation is adequate, whereas deep sedation achieves better outcomes for longer, more complex exams (6-10). Finally, the staff responsible for sedation must always be ready and able to rescue patients progressing to sedation levels deeper than intended.
Recommendations:
1. Sedation level and drug type depend on procedure characteristics, individual patient-related factors, patient preferences, and need for patient cooperation (evidence level 4, recommendation grade D).
2. For non-complex diagnostic or therapeutic gastroscopy and colonoscopy superficial sedation suffices (evidence level 1+, recommendation grade A).
3. For complex or prolonged procedures (ERCP, EUS, etc.) deep sedation is to be preferred (evidence level 1+, recommendation grade A).
Skills required to perform sedation during gastrointestinal endoscopy. General rules for sedation. Sedation training for endoscopists
All scientific societies agree that specific training is required for practitioners involved in sedation, as well as official certification for basic life support. Endoscopy units where sedation is applied must have at least one person certified in advanced cardiopulmonary resuscitation techniques. Theoretical and practical sedation skills for endoscopy should be included in the specialty curriculum.
Multiple clinical practice guidelines are available that include sedation recommendations for digestive endoscopy, but it was not until the last decade that several European and US societies eventually established specific rules regarding sedation training (11,12).
The Sociedad Española de Endoscopia Digestiva has been offering training courses on deep sedation for endoscopists for four years now. These courses allowed a widespread use of sedation, mainly using propofol, in endoscopy units.
General rules for sedation to be met by all endoscopy unit staff members:
1. Understanding the minimal sedation equipment that needs to be available in an endoscopy unit.
2. Having a unit-specific sedation protocol according to recommendations in clinical practice guidelines.
3. Understanding the characteristics of drugs to be used for sedation.
4. Recognizing the various sedation levels and possessing skills to rescue patients anytime from a deeper-than-intended level.
5. Having the necessary skills for airway management and certification on basic life support, to be renewed every three years.
Sedation training for endoscopists must include both theoretical and practical education (13,14).
Theoretical contents must include the following:
1. Required documentation: Sedation-specific informed consent; medical record; sedation record; databases.
2. Materials and means necessary in an endoscopy unit: Examination room, preparation and recovery room. Skills regarding monitorization instrument operation, data interpretation, and limitations.
3. Prior assessment of patient risks: Sedation-specific history taking. ASA anesthesia risk classification. Mallampati scale. Recognizing situations where the presence of an anesthesiologist is advisable during sedation.
4. Knowledge of drugs used for sedation: Pharmacological and pharmacodynamic characteristics, administration regimens, dosage, synergies, interactions, and side effects. Drug preparation and administration mode (boluses, infusion pumps).
5. Understanding of sedation levels and related assessment scales.
6. Recognition and management of complications. Airway management.
7. Sedation during pregnancy and lactation.
8. Patient transfer to the recovery area. Post-sedation monitoring. Unit discharge criteria. Subsequent recommendations.
9. Knowledge of clinical practice guidelines and recommendations by scientific societies.
10. Legal aspects of sedation.
Practical training
Practical skills should be acquired in certified units and must include the following:
1. Pre-sedation history taking and risk assessment.
2. Indication and administration of all drugs necessary for each procedure at the appropriate dosage to achieve the desired sedation level.
3. Patient and vital sign monitoring during sedation.
4. Implementing appropriate corrective maneuvers for desaturation or any other events that may arise.
5. Patient monitoring in the recovery room and discharge time scheduling using the various assessment scales available.
In Spain both basic and advanced life support certificates should be officially recognized by one of the scientific societies and health care institutions included in the Consejo Español de Reanimación Cardio-Pulmonar (CERCP) -Intensive Medicine (SEMYCIUC), Cardiology (SEC), Anesthesia (SEDAR) and Emergency Medicine (SEMES).
Recommendations:
1. All endoscopy team members involved in sedation must be certified in both theoretical and practical sedation techniques (evidence level 4, recommendation grade D).
Traditional sedation (benzodiazepines and opiates). Drugs. Dosage. Antagonists
This the commonest form of sedation for gastrointestinal endoscopy when performed by non-anesthetist doctors. Drugs may be administered alone or in combination, and as intravenous boluses (see boxes). Usually, the goal of traditional sedation is the achievement of superficial sedation. Its use is particularly suited for basic diagnostic techniques, primarily gastroscopy and colonoscopy (15). In elderly patients or individuals with renal, liver or respiratory failure caution and reduced doses are advised (16).
- Benzodiazepines: Both midazolam and diazepam may be considered. Midazolam has a rapid onset and a short duration of action, and provides useful though variable amnestic effects. Because of this it is now the benzodiazepine of choice (16,17). It has minimal cardiovascular effects.

- Opiates: Meperidine and fentanyl are most commonly used. Caution is advisable when given to patients receiving other central nervous system depressants, and administration should be avoided in individuals on monoamine oxidase inhibitors.
- Meperidine: Meperidine has a wide margin of safety; however, nausea is more common when compared to fentanyl, and metabolites accumulate particularly in patients with renal disease. Both sedative and analgesic effects are less predictable than with other opiates.

- Fentanyl: Analgesic potency is much higher than meperidine's, and its pharmacodynamic profile is better because of a shorter half-life. It may induce respiratory depression, which persists longer than analgesia. It fits the duration of endoscopic procedures as 20-25 min after dosing most patients show stabilized vital signs and may be discharged. In addition to respiratory depression high doses may result in bradycardia and hipotension, which should be borne in mind. While meperidine was the most commonly used opiate among endoscopists in the past, it is now being gradually replaced by fentanyl (18,19).

- Antagonists: They counteract the effects of benzodiazepines and opiates in patients with oversedation not reversed following appropriate ventilation and stimulation. Its routine use to speed up recovery after endoscopy is not recommended (16). Their half-life is shorter than that of antagonized compounds, hence resedation is possible.
- Flumazenil: A benzodiazepine antagonist. It should not be administered to patients with seizures on benzodiazepines or high intracranial pressure.

- Naloxone: Opioid antagonist. When used together with benzodiazepines and opiates, and the patient develops respiratory depression, naloxone should be administered first because of its greater effect on respiratory depression.

Recommendations:
1. When benzodiazepines are used midazolam is recommended (evidence level 2++, recommendation grade B).
2. Moderate sedation using currently available drugs for routine endoscopic procedures (colonoscopies and gastroscopies) is highly satisfactory for patients and physicians alike given their low risk for adverse events (evidence level: 1-, recommendation grade: A).
3. If a patient has respiratory depression during sedation with benzodiazepines and/or opiates and does not respond to stimulation or oxygen ventilation, the administration of antagonists for said drugs is recommended (evidence level 2-, recommendation grade D).
4. Time to recovery following routine endoscopy is shorter when fentanyl rather than meperidine is used (evidence level 1, recommendation grade B).
Sedation with propofol. Dosage and mode of administration
Propofol (2-6-diisopropylphenol) is a drug structurally unrelated to other sedatives and with pharmacokinetic characteristics that, in many respects, make it an ideal drug for gastrointestinal endoscopy. Its main features include a rapid onset of action (30-40 seconds) and short half-life (4-5 minutes). This fast action is based on its formulation's high liposolubility. Also, its antiemetic properties and absence of many undesirable effects that are common with other drugs allow a really fast, pleasing awakening and provide patients with outstanding perceived comfort. Its safety profile when used by endoscopists or trained nurses has been consistently demonstrated in clinical trials, showing a rate of complications equal to or lower than traditional sedation (20,21). In contrast, its main drawback is a very narrow therapeutic window that renders precise dose titration mandatory. Furthermore, its pharmacokinetics is influenced by multiple factors -drugs, tobacco, alcohol, age, obesity, and other circumstances may influence patient response to propofol. From the above, individualized dosing is key, with titration according to observed clinical response. In addition, as this drug may bring about significant hemodynamic changes, its use is advised under close supervision by trained healthcare personnel and using adequate surveillance with at least arterial O2 saturation, heart rate, respiratory rate, and blood pressure monitoring (15).
Administration modes depend on the examination's duration and complexity, and on the unit's staff. Overall, it is recommended that sedation be induced with repeated boluses every 20-30 seconds for short, non-complex explorations (mainly diagnostic gastroscopy). The initial bolus depends on patient characteristics, weight, and age -in a young, healthy ASA I patient sedation may be induced with a 40-60 mg bolus, whereas lower initial doses (10-20 mg) are recommended for elderly, weak subjects; successive doses of 10-20 mg will then be administered until the patients spontaneously closes his or her eyes with absent response to verbal stimuli. With this induction additional doses are usually not needed for a short diagnostic exam. For longer explorations (colonoscopy, therapeutic gastroscopy) a staff member should be present to administer booster doses or perhaps propofol using an infusion pump. Infusion rate varies from 2 to 8 mg/kg/h depending on individual response and examination-related discomfort. A formula to estimate infusion rate based on response to initial induction has been recently reported (22). Using a syringe pump deep sedation is induced at a constant rate of 200 mL/hour (150-100 mL/hour for weak or elderly patients) for 1 % propofol (10 mg/mL). Once deep sedation is reached the pump is stopped and a calculation is made where the infused volume in mL is multiplied by four. The resulting amount will be used as infusion rate in mL/hour.
Combined use with midazolam
Under some circumstances so-called balanced sedation becomes useful. A prior administration of midazolam (1-2 mg two minutes in advance) reduces propofol requirements and propofol-related adverse hemodynamic effects (23,24). This is particularly useful for weakened patients, most particularly with heart disease and impaired ejection fraction. It may also be appropriate for younger patients or drug addicts with foreseeable higher propofol requirements.
Contraindications
Propofol is contraindicated in patients allergic to propofol and in patients with a low ejection fraction or at risk for bronchoaspiration. The presence of soy and egg components in the emulsion initially advised against its use in patients with allergy to these foods. However, there is now evidence that propofol may be safely used in subjects with egg allergy provided they never developed anaphylaxis (25). It is nevertheless prudent to assess such cases on an individual basis and consider the use of alternative medications. Special care should be used with ASA IV patients, where the presence of an anesthetist or other options should be considered.
Recommendations:
1. Propofol is an ideal drug to provide sedation for endoscopic examinations (evidence level 1+, recommendation grade A).
2. The use of propofol by endoscopists or trained nurses is as safe as traditional sedatives when monitoring is adequate (evidence level 1++, recommendation grade A).
3. The use of propofol by endoscopy staff in ASA III patients is feasible and safe in experienced endoscopy units (evidence level 3, recommendation grade D).
4. Propofol dosing must be tailored according to patient response and baseline status (evidence level 1++, recommendation grade A).
5. Midazolam administration before propofol allows to reduce dosage and adverse effects, particularly hypotension in cardiac patients or in hypovolemia, but recovery is delayed (evidence level 1+, recommendation grade B).
Human and material resources necessary for effective, safe sedation. Monitoring. When is an anesthesiologist essential?
Human resources
Sedation guidelines and propofol label indicate that deep sedation should be administered by qualified personnel other than those carrying out the examination (18,26). However, no scientific evidence has shown any benefits versus sedation with propofol administered by the same staff aiding in the procedure (27,28). Exploration characteristics and patient risks must be considered when making such a decision (Fig. 1). Non-invasive, non-complex diagnostic exams in ASA I-III patients with no risk factors may be effectively and safely performed in the absence of dedicated sedation staff, with no increase in the number of people inside the room. In complex therapeutic procedures and/or examinations in advanced ASA (> III) individuals or subjects at risk regarding sedation (short neck, sleep apnea, severe decompensated chronic conditions, etc.) (Table III) sedation-related adverse events are more common, hence the presence of an additional qualified practitioner responsible for sedation is highly advisable. Help from an anesthetist, intensivist or qualified nurse is recommended in such cases (29).
Required qualifications
The staff performing sedation and the members of the endoscopy unit where propofol is used must have knowledge, experience and training regarding this drug, as previously discussed. The whole staff must be qualified for basic life support, and at least one member should be certified in advanced life support; otherwise, an anesthesiologist or intensivist should be available within five minutes.
Roles of staff responsible for sedation
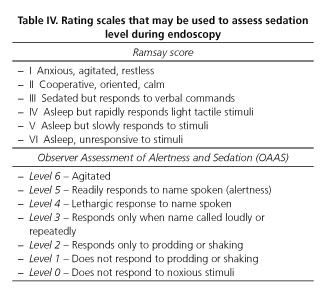
These include the design and management of the whole sedative administration process. Depending on the type of exploration to be performed and on patient characteristics, the following should be assessed: a) Sedation level necessary; b) induction and maintenance doses; c) administration mode; d) maintenance and patient monitoring using the relevant scales (Table IV) (17,30); and e) control of activity or breathing movements (with the aid of capnography, bispectral index or narcotrend when available) (31).
Preparing propofol for IV administration requires special care as this is a lipophilic drug with a high risk for bacterial or fungal contamination (32). Strict handling includes: opening a vial for each patient immediately before administration, disposing of vial remnants and infusion pumps, and changing adapters, conduits and syringes for each case.
Material resources
The Unit should have all sorts of sedation-related materials available, including: a) Sedatives and their antagonists; b) IV systems and infusion pumps; c) oximetry, ECG, and blood pressure monitors. A capnograph and bispectral index/narcotrend are desirable, particularly for higher-risk examinations (31); d) resuscitation equipment; e) defibrillator; f) Basic and advanced respiratory care systems; and g) drugs for cardiopulmonary resuscitation.
Good venous access, patient preoxygenation for 5 minutes before sedative dosing, a readily available independent aspirator, and a well-checked crash cart are all key components.
Appropriate gurneys and transportation means are also essential that provide space for resuscitation maneuvers, protection against falls, and ergonomy for both patients and staff.
The widespread use of sedation in endoscopy units makes mandatory an architectural design adapted to the use of deep sedation techniques.
The increasing use of propofol, which provides deep sedation with a rapid recovery, requires resuscitation systems available until the patient fully regains consciousness and the health status present before the procedure. To achieve maximal efficiency in the Unit a recovery ward with 1.5-2.0 boxes per operating endoscopy room is considered a must (33). The recovery ward should be staffed with nurses and fitted with cardiopulmonary support systems, monitors, gurneys, accessory rails, oxygen outlets, and aspiration inlets.
Recommendations:
1. Deep sedation with propofol for basic endoscopic procedures and patients with ASA I-II risk may be carried out effectively and safely in the absence of dedicated sedation staff and with no increase in the number of people inside the room (evidence level 2+, recommendation grade C).
2. For complex therapeutic procedures having an additional, qualified person responsible for sedation is advisable (evidence level 4, recommendation grade D).
3. For procedures performed in patients with advanced ASA scores (> III) or with risk factors for sedation (short neck, sleep apnea, chronic decompensated serious diseases, etc.) the presence of an anesthesiologist or intensivist is to be recommended (evidence level 4, recommendation grade D).
4. In endoscopy units where deep sedation is used an anesthesiologist or intensivist should be available within 5 minutes (evidence level 2+, recommendation grade C).
5. Given propofol's high risk of contamination the aseptic technique must be maximized during handling, particularly avoiding multidose containers and reusable infusion materials (evidence level 1++, recommendation grade A).
6. Endoscopy units should be fitted with all items necessary for safe, effective sedative dosing, as well as monitoring and cardiopulmonary resuscitation equipment (evidence level 2++ , recommendation grade B).
7. A recovery room with nurses, gurneys, oxygen, aspiration, monitors, and cardiopulmonary support devices is advisable (evidence level 4, recommendation grade D).
Sedation-related complications. Prevention, diagnosis, and management
The overall rate of complications of digestive endoscopy is low (0.02 %-0.54 %), with mortality at 0.0014 %. Of these, 0.27 % are cardiopulmonary, sedation-related complications. These are most common in patients with associated diseases and develop equally in procedures surveilled by both anesthetists and non-anesthetist clinicians. Most common complications include hypoxemia, hypotension, arrhythmia, vasovagal events, and bronchopulmonary aspiration (26,34).
Cardio-respiratory complications
The most common and serious of all complications, their rate was 0.9 % in a retrospective nation-wide study of over 300,000 procedures carried out in the USA (35).
Hypoxemia
Oxygen desaturation defined by satO2 < 90 % is the most common complication, possibly more common than usually thought as it is not recorded on many occasions. Incidence is highly variable (4-50 %). The risk is greater during oral endoscopy since a deeper level of sedation is needed, the airway is compressed, and laryngospasm occasionally develops. The combined administration of benzodiazepines and opiates increases the risk for respiratory depression (36). In recent studies with oxygenated, monitored patients the incidence of desaturation events during endoscopies performed under propofol was lower than 10 % (37), and the need for endotracheal intubation remained marginal.
Does oxygen administration prevent hypoxemia? All guidelines issued by national scientific societies advise that supplementary oxygen be used during endoscopic procedures. However, oxygen administration may delay apnea recognition and increase hypercapnia, hence a pulse oximeter is also recommended to provide visual monitoring for breathing movements, as well as capnography when feasible (35).
If desaturation develops sedatives must be discontinued and the patient must be stimulated using increased oxygen flow, jaw thrust to secure the airway, secretion aspirations, and a Guedel tube when required. If benzodiazepines and/or opiates were used their action may be reverted with flumazenil and/or naloxone. When desaturation is severe and persistent ventilation should be provided using an oxygen mask (Ambu), but this is only necessary in 0.1 % of cases. Should these measures fail, respiratory resuscitation maneuvers must be initiated using a laryngeal mask or orotracheal intubation; need for the latter is exceptional (38).
Hypotension
Defined by a maximal blood pressure < 90 mm Hg, it develops more commonly in cases where sedatives and pain killers are associated or when propofol is used; it usually has no clinical implications. Management usually includes electrolyte IV infusion.
Arrhythmia
Arrhythmia develops in 4-72 % of sedations; most are sinus tachycardia events possibly related to procedure-associated stimuli, but other clinically relevant arrhythmias may occur (extrasystoles, bradycardia, ectopic rhythms, etc.). Their development depends on patient age, presence of concurrent, particularly heart diseases, endoscopy type, and anxiety. Electrocardiographic changes appear in 4-42 % of cases, most commonly ST segment alterations that remain unchanged by oxygen administration and are believed to be unrelated to ischemia. Should bradycardia occur (< 50 bpm) atropine must be provided (0.5 mg IV, to a maximum of 2-3 mg).
Aspiration
This occurs in few cases (0.10 %) and usually defies recognition. However, the risk for bronchopulmonary aspiration is much higher in patients with active upper gastrointestinal bleeding or gastric retention; in such cases orotracheal intubation is recommended before the endoscopic procedure.
Phlebitis
The frequency of phlebitis is low but higher when diazepam is used in small-caliber veins. Some propofol preparations irritate venous walls, and extravasation results in pain and swelling; lidocaine may be added to the infusion to prevent this; cold application is advisable should extravasation develop.
A marginal yet possible, potentially severe complication is the transmission of bacterial, fungal or viral infections (including hepatitis C virus) because of multidose containers and propofol contamination.
Can we identify patients with higher cardiopulmonary risk? Multiple risk factors have been associated with a greater frequency of cardiopulmonary complications. Some are patient-related, including a history of ischemic heart disease or arrhythmia, lung disease, hospitalization, baseline O2 saturation < 95 %, age older than 70 years, and ASA III and IV (35,36,39-41). Other factors are associated to procedure type and are more common in emergency procedures or oral endoscopy (38,42); finally, they may also be related to drug dosage, and oxygen administration status (35).
A thorough assessment prior to sedation may identify these factors and allow actions to prevent complications. The best way to prevent them is by adequate training and having expert staff -both doctors and nurses- to manage sedation (38).
Recommendations:
1. Supplementary oxygen administration during endoscopic procedures reduces the incidence of hypoxemia but may delay apnea recognition and increase hypercapnia; hence, besides using a pulse oximeter, visual monitoring of breathing movements is advisable, and a capnograph is recommended (3) (evidence level 1+, recommendation grade B).
2. In situations with an increased risk for bronchoaspiration, as is the case with active upper GI bleeding or gastric retention, orotracheal intubation is required before the endoscopic procedure (evidence level 2+, recommendation grade B).
Pre-, intra-, and poest-sedation monitoring. Records
Having a sedation form available is advisable to record clinical data and vital signs before, during and after sedation. Similarly, all incidents occurring during sedation, as well as actions taken to solve them, should be recorded. This record form should be attached to the patient's medical record. The following sequence is advisable:
1. Pre-sedation monitoring:
- Anamnesis: The patient's individual risks should be assessed. The aim is identifying all factors that may increase sedation-associated risks. Except for specific cases neither referral for a pre-anesthetic check-up nor additional studies such as chest X-rays or electrocardiography are necessary. Good history taking immediately before a procedure is currently considered a proper replacement for conventional pre-sedation visits, which to date have not been proven essential (43).
- Medical history: Confirm the patient has been fasting for 6-8 hour for solids and 2-4 hours for liquids, and is accompanied by a responsible adult. Record the medical history likely to complicate sedation: severe cardiopulmonary or neurological disease; sleep apnea; prior adverse events with sedation/anesthesia or a history of difficult intubation; alcohol or other drug abuse; allergies to medications and, specifically, to egg and soy; potential risk for bronchoaspiration (intestinal occlusion, active gastrointestinal bleeding, gastric stasis, etc.).
- Physical exploration: Vital signs (blood pressure, heart rate, oxygen saturation) and prior level of consciousness; assess the presence of obesity and of anatomic changes in the neck and oropharynx that might ultimately hinder intubation (Mallampati classification) (44).
According to medical record and examination findings the patient's risk regarding sedation is evaluated using the ASA classification (14).
- Peripheral vein cannulation and supplementary oxygen administration: Supplementary oxygen administration is recommended prior to the procedure (nasal cannula or mouth opener with oxygen tubing) as it reduces the incidence of arterial desaturation.
2. Monitoring during sedation:
The patient must remain monitored throughout the procedure. Using a pulse oximeter is mandatory in all instances. For deep sedation as well as for patients with severe heart disease surveillance with blood pressure (every 3-5 minutes), electrocardiogram, and ventilatory function recorders is compulsory (38,45-50). Ventilation may be assessed by observing breathing movements or, if available, with a capnograph. However, the use of a capnograph has not proven indispensable. Monitorization data must be included in the medical record form.
- Level of consciousness: An assessment will be made of the response to verbal or tactile stimuli. Several scales or instruments are available to help us establish the level of consciousness, including the bispectral index/narcotrend (17,30). This assessment must be performed every 3-5 minutes by the person responsible for sedation in order to maintain the desired sedation level and rescue the patient from a deeper level if needed.
3. Monitoring after procedure completion:
- Post-sedation surveillance: All patients having undergone sedation must be adequately monitored until they recover their baseline status, out of danger, and ready to be discharged from the endoscopy unit. Once the endoscopic procedure is completed, and the defensive reflexes recovered, patients may be transferred to a recovery room with the above-mentioned staff and equipment.
As already discussed, the use of scores is recommended to assess discharge time. In practice, Aldrete's scale is the most commonly used score -9 or 10- to decide this (51) (Table V). The fact that this scale assesses physical parameters rather than psychomotor activity should be taken into account. It is for this reason that discharged patients should be in the company of a responsible adult. It is recommended that sedation be avoided for outpatients with no companions.
It is also relevant to bear in mind that, as the half-life of sedatives is longer than that of their agonists, when the latter are administered patients will need to stay longer in the recovery room to prevent potential resedation events. Providing precise written instructions for the 24 hours following sedation is highly advisable, including a phone number to contact the endoscopy unit should any adverse events or concerns arise after discharge.
Recommendations:
1. Sedation requires monitoring before, during and after the endoscopic procedure until the patient is no longer at risk (evidence level 4, recommendation grade D).
2. All actions and incidents occurring during sedation must be recorded and attached to the patient's medical records (evidence level 4, recommendation grade D).
3. With exceptions, a pre-anesthetic visit and check-up including chest X-rays and ECG is not necessary for gastrointestinal endoscopic procedures (evidence level 4, recommendation grade D).
4. To undergo sedation patients must fast 6-8 hour for solids and 2-4 hours for liquids (evidence level 4, recommendation grade D).
5. It is recommended that Aldrete's or other similar scales be used to establish discharge time for patients, who should leave the endoscopy unit accompanied by a responsible adult (evidence level 4, recommendation grade D).
6. Stay time in the recovery room will be longer for patients having received sedative antagonists (evidence level 4, recommendation grade D).
Sedation in special situations: pregnancy, lactation, pediatric age
Sedation during pregnancy
The safety of endoscopic procedures under sedation during pregnancy has not been thoroughly studied. The fetus is particularly responsive to hypoxia and hypotension in the mother (52); it is because of this that elective non-obstetric procedures, including GI endoscopy, are recommended only for a clear indication, and should be delayed to the second trimester when possible (52,53) in order to reduce the potential risks associated with perioperative stress, the procedure itself, and the effects of all drugs administered. However, numerous studies have confirmed the relative harmlessness of a single clinical exposure to anesthesia and surgery during the first trimester (54-57).
Today's sedative and anesthetic agents have no proven teratogenicity (Table VI). Meperidine and propofol (class B) or fentanyl and midazolam (class C) may be used safely during pregnancy. Pregnancy-related physiological changes increase responsiveness to thiopental and volatile anesthetics, whose induction doses should be reduced. In contrast, no reduction is required for propofol induction dosing (58).
Sedation and lactation
The responsiveness of breastfeeding women to sedatives is similar to that of other adults (53). Usual sedatives may be safely administered to women during lactation with no particular risk to the infant provided a number of recommendations are followed (59) -among opiates fentanyl is preferable to meperidine; fentanyl levels in breastmilk are low enough to lack pharmacologic effects (60,61) whereas meperidine does concentrate in breastmilk and may thus reduce infant alertness and interfere with feeding (59,62). As regards midazolam, breastfeeding should be delayed at least 4 hours following its dosing; breastmilk should be expressed and disposed of before feeding the child. Propofol concentration in breastmilk is only 0.015 % of plasma levels, hence lactation needs not be withheld after this drug (60).
Sedation in children
In contrast to adults, children require sedation for most invasive procedures as anxiety must be usually controlled, movements restrained, and pain and discomfort avoided. Sedation requirements outside operating rooms, by multiple specialists, and for a variety of diagnostic procedures are increasing in the pediatric setting (63). Limited anesthetic resources, increased efficiency in patient management, and both patient and physician convenience drive a steady increase in pediatric sedation by non-anesthetist clinicians (64,65), with no differences being reported in the frequency of adverse events among the various specialists in charge of sedation (66).
In gastrointestinal endoscopy, for selected cases, sedation is an option as effective as general anesthesia (67,68). Oral premedication with midazolam (0.5 mg/kg) (69,70) or ketamine (5 mg/kg) (71) may ease parental separation and venous cannulation, and reduce sedative dose requirements as well.
Single or combined sedatives have been used for endoscopy-related sedation in children. A combination of sedatives does not increase the potential for adverse events as compared to sedation with only one drug, but does increase the intricacy of the sedation process (69-71). As in adults, propofol doses are reduced when combined with midazolam and/or fentanyl (69,70). The combination of midazolam and ketamine provides better sedation for endoscopy versus midazolam or midazolam/fentanyl, as well as a faster recovery (71). The use of midazolam alone has been reported as likely ineffective (67).
Propofol has been shown to shorten induction time and recovery from sedation versus midazolam (72) or midazolam/meperidine (73).
A recent systematic review suggests that propofol-based sedation is the most effective regimen for digestive endoscopy in the pediatric setting (67) -propofol ensured an excellent level of successful procedures, better time management, and maximum patient comfort, particularly when midazolam was previously administered. In most studies propofol was administered by non-anesthetist clinicians (including endoscopists) with no increase in adverse events; the authors conclude that propofol may be safely administered by trained physicians. Repeated deep sedation with propofol in infants/toddlers has proven to be safe (74,75), although human research on this subject is scarce and potential risks should be weighed (76). Beyond infancy, in the absence of organ-specific dysfunction or disease sedative effects and clearance is proportional to adults.
Recommendations:
1. Indications should be unequivocal during pregnancy, and procedures should be postponed when possible until the second trimester (evidence level 4, recommendation grade D).
2. Benzodiazepines, opiates, and propofol may be used during pregnancy. Propofol induction doses need not be reduced (evidence level 1-, recommendation grade B).
3. If midazolam is used during breastfeeding breastmilk must be expressed and discarded, and feeding must be delayed to at least 4 hours after sedation; among opioids fentanyl is to be preferred to meperidine. Breastfeeding needs not be delayed after sedation with propofol (evidence level 3, recommendation grade D).
4. In the pediatric setting sedation may be an option as effective as general anesthesia. Oral premedication with midazolam may result in easier separation from parents, easier venous access cannulation, and lower sedative dose requirements (evidence level 1+, recommendation grade A).
5. In children sedation with propofol is effective and safe, and works better when midazolam is used for premedication (evidence level 1+, recommendation grade A).
Efficiency. Sedation costs
The use of sedation during gastrointestinal endoscopy reduces the discomfort and anxiety usually experienced by patients through the procedure, increases cooperation, and facilitates the examination. This translates into higher tolerance and satisfaction levels with the care received (perceived quality), and greater readiness to undergo repeated procedures when needed. The use of sedation has been shown to even improve the scientific-technical quality of explorations both for gastroscopy, where a better view of the esophago-gastro-duodenal tract is achieved (77), and colonoscopy, where sedation improves major quality indices, including the percentage of complete exams and adenoma resection rates (78).
However, these undeniable benefits of sedation may be burdened with increased exploration costs and reduced efficiency in the endoscopy unit. Sedation increases cost by rising pharmacy (drugs and IV fluids) and both fungible (venous access catheters, drip systems, oxygen administration devices, etc.) and non-fungible (monitoring equipment) material expenses. However, even more relevant than cost increases is the impact sedation may have on procedure length. Endoscopic procedures under sedation require additional time for previous venous access cannulation and sedation induction. On the other hand, patients must be monitored during recovery until their discharge from the endoscopy unit. This longer time is the factor that most significantly may impact efficiency. Furthermore, the use of sedation requires appropriately trained personnel to monitor patients during sedation and recovery, including an anesthesiologist for some cases, which further boosts costs.
Therefore, before an endoscopy sedation program is implemented the characteristics of the involved unit and its patient population should be properly analyzed in order to decide which of the above sedation strategies fits better our needs and means.
Assessing the cost-effectiveness of endoscopy sedation is challenging. On the one hand, the main goal of sedation during endoscopy, the achievement of higher tolerance and satisfaction levels, is a perceived quality parameter that cannot be easily quantified in economic terms. On the other hand, sedation cost-effectiveness is influenced by multiple factors that vary within and among countries. Thus, a hard-pressed unit will need fast patient turnover to keep up pace. In such a case a sedation strategy allowing shorter induction times and most particularly shorter recovery times would be of choice. In contrast, when care burdens are low such times are not so much a determinant of efficiency. Similarly, another core issue in determining the impact of sedation on efficiency is the amount of recovery beds per examination room. When few recovery beds are available sedation should allow faster recovery times to keep patient turnover high. Otherwise, when two or more recovery beds are available per endoscopy room delayed patient recovery will have no major impact on the unit's efficiency. Also important is an assessment of the endoscopy unit's patient population characteristics. If most are younger individuals or persons with minor conditions any of the above sedation strategies may be used without influencing efficiency. In contrast, if the patient population includes mostly elderly or multidisease individuals (ASA > III), the use of anesthetics such as propofol will often require the help of an anesthetist in the unit, which will increase overall costs and decrease efficiency.
If a benzodiazepine is to be used, midazolam is the drug of choice for endoscopy-related sedation because of its short onset of effect and shorter half-life as compared to other drugs in this class (79); midazolam provides rapid sedation induction and earlier patient recovery after the procedure. Regarding opiates, fentanyl significantly shortens induction and patient recovery versus meperidine (80,81). This shortening of times results in increased efficiency at the endoscopy unit. Induction and recovery times for both basic and advanced endoscopy are shorter with propofol than with benzodiazepines and opioids (82,83). Sedation with propofol administered by a non-anesthetist clinician may improve efficiency when compared to sedation with opiates and benzodiazepines (82,83). Also, the administration of propofol by an anesthetist during a routine endocopic procedure for a healthy, low-risk patient (ASA < III) is not cost-effective (38).
As discussed above, different sedation strategies exist. Some are based on the use of benzodiazepines either alone or associated with opioids, and others on the use of propofol either alone or in combination with opiates and/or benzodiazepines. Selecting one must be based primarily based on staff experience and training, and available technical resources. However, we must also assess the impact the selected approach may have on our endoscopy unit's efficiency. We should reach an appropriate balance between the benefits obtained with sedation and increased costs as well as potential efficiency reductions.
Recommendations:
1. When benzodiazepines are used, midazolam is the drug of choice for endoscopy-related sedation as it provides fast sedation induction and earlier patient discharge after the procedure (evidence level 2++, recommendation grade B).
2. The use of fentanyl rather than meperidine significantly reduces patient induction and recovery times. This reduction results in increased efficiency at the endoscopy unit (evidence level 2++, recommendation grade B).
3. Sedation induction time is shorter with propofol than with benzodiazepines and opiates (evidence level 1+, recommendation grade A).
4. Recovery time after sedation is shorter when propofol is used alone (evidence level 1+, recommendation grade A).
5. Sedation with propofol administered by non-anesthetist clinicians may improve endoscopy unit efficiency as compared to sedation with opiates and benzodiazepines (evidence level 1+, recommendation grade A 1+).
6. Routine propofol administration by an anesthesiologist to healthy, low-risk patients (ASA < III) in the endoscopy setting is not cost-effective (evidence level 1+, recommendation grade A).
Informed consent
To provide sedation in the digestive endoscopy setting patients must provide their informed consent (IC) in accordance with the Basic Law of Patient Autonomy (84) and the Medical Code of Deontology (85). For patients younger than 16 or if factual incapacity to receive information and/or give consent for the procedure is present the IC must be obtained from the patient's legal representatives. In life-threatening emergencies in the absence of legal representatives the circumstances leading to the waiving of informed consent must be accurately detailed in the medical record. The information given and the IC obtained by the physician prescribing the endoscopy do not exempt the endoscopist/sedator from his or her obligation to inform and obtain an IC. This obligation cannot be delegated to nurses or auxiliary staff. The verbal and written information provided on sedation must be accurate and understandable by the patient. It must include a discussion on the benefits and risks of sedation (including those related to vehicle driving and other dangerous activities after the procedure), potential complications, both typical and more severe, and available alternatives (including an optional endoscopy with no sedation). The fact that sedation will be administered by qualified personnel under the responsibility of an endoscopist, anesthesiologist or intensivist should also be made explicit. The informed consent represents a medical, legal and ethical aspect not amenable to scientific research, hence no "scientific evidence" exists to establish recommendations thereupon. Its regulation depends on national laws, in this case the Spanish Basic Law of Patient Autonomy (84), and on the jurisprudence thereof. It is "scientifically" considered an expert opinion with the lowest grade of recommendation, but recommendations are both legally and ethically mandatory.
Medico-legal implications of sedation administered by non-anesthetists
In Spain, any Graduate of Medicine and Surgery is entitled to perform any medical act for which he or she has acquired appropriate training and skills, including sedation without a specialist's degree in Anesthesiology and Resuscitation. However, these clinicians must be aware of their own limitations and seek the help of expert colleagues whenever it is advisable. Under the Spanish legal system (86-91) that of "physician" is the only "medical profession" acknowledged. There is no "medical specialist" profession. "Specialties" are variations within a single medical profession. The profession of "physician" is acquired by obtaining the academic degree of Graduate of Medicine and Surgery, which entitles to practice the medical profession in its totality (87), in any or all of its branches but without claiming a specialist's degree in any of them. A specialist physician degree does not establish the specialty's sphere of competence (88), and no limits exist between medical specialties (89,90). No law expressly restricts to specialist physicians the performance of any specific activities of procedures (91). Academic degrees (graduate) and official degrees (specialist) do not grant: a) Necessary competence in an automatic, indefinite way; b) immunity against negligence or misjudgement; c) the right to exclusively exploit any specific procedure; and d) the monopoly to practice in a specific field. Physicians are entitled to unlimited professional practice, unless they act in ethically unsound ways (92). The Criminal Code (93) defines the crime of unauthorized practice as "the performance of activities specific of a profession by a person not licensed to do so", hence no graduate of medicine and surgery may be charged with this crime. Unauthorized practice is nonexistent between medical specialties (91).
Recommendations:
1. A specific informed consent must be obtained whereby the patient receives information on the characteristics of sedation, the staff responsible for it, its risks, and the available alternatives (evidence level 4; recommendation grade D).
2. The patient may withdraw his or her consent at any time by informing of his or her decision in writing (evidence level 4; recommendation grade D).
3. To perform sedation for endoscopy appropriate competence must be acquired and maintained through initial and continuing training programs (evidence level 4; recommendation grade D).
4. The endoscopist must be aware of the limits of his or her own competence, and seek the help of a competent colleague (anesthetist or otherwise) whenever a sedation process goes beyond his or her expertise (evidence level 4; recommendation grade D).
References
1. López-Rosés L, Sociedad Española de Endoscopia Digestiva. Guía de sedoanalgesia en endoscopia. Rev Esp Enferm Dig 2006;98:685-92. [ Links ]
2. Harbour R, Miller J, for the Scottish Intercollegiate Guidelines Network Grading Review Group. A new system for grading recommendations in evidence based guidelines. BMJ 2001;323:334-6. [ Links ]
3. American Society of Anesthesiologists. Distinguishing Monitored Anesthesia Care ("MAC") from Moderate Sedation/Analgesia (Conscious Sedation) (Approved by the ASA House of Delegates on October 27, 2004). Available at: http://www.asahq.org/For-Healthcare-Professionals/Standards-Guidelines-and-Statements.aspx Accessed April 22, 2008. [ Links ]
4. Guidelines for conscious sedation and monitoring during gastrointestinal endoscopy. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc 2003;58:317-22. [ Links ]
5. Guidelines for the use of deep sedation and anesthesia for GI endoscopy. American Society For Gastrointestinal Endoscopy. Gastrointest Endosc 2002;56: 613-6. [ Links ]
6. Carlsson U, Grattidge P. Sedation for upper gastrointestinal endoscopy: A comparative study of propofol and midazolam. Endoscopy 1995;27:240-3. [ Links ]
7. Patterson KW, casey PB, Murray JP, O'Boyle CA, Cunningham AJ. Propofol sedation for outpatient upper gastrointestinal endoscopy: Comparison with midazolam. Br J Anaesth 1991;67:108-11. [ Links ]
8. Jung M, Hofmann C, Kiesslich R, Brakhertz A. Improved sedation in diagnostic and therapeutic ERCP: Propofol is an alternative to midazolam. Endoscopy 2000;32:233-8. [ Links ]
9. Wehrmann T, Kokapick S, Lembcke B, Caspary WF, Seifert H. Efficacy and safety of intravenous propofol sedation for routine ERCP: A prospective controlled study. Gastrointest Endosc 1999;49:677-83. [ Links ]
10. Vargo JJ, Zuccaro G, Dumot JA, Shermock KM, Morrow JB, Conwell DL, et al. Gastroenterologist-administered propofol versus meperidine and midazolam for ERCP and EUS: A randomized, controlled trial with cost effectiveness analysis. Gastroenterology 2002;123:8-16. [ Links ]
11. Multisociety sedation curriculum for gastrointestinal endoscopy. Gastrointest Endosc 2012;76:1-25. [ Links ]
12. European Curriculum for Sedation Training in Gastrointestinal Endoscopy: Position Statement of the European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA). Endoscopy 2013;45:495-503. [ Links ]
13. Training in patient monitoring and sedation and analgesia. Communication from the ASGE Training Committee. Gastrointestl Endosc 2007;66:7-10. [ Links ]
14. Practice guidelines for sedation and analgesia by non-anesthesiologists. American Society of Anestesthesiologists Task Force on Sedation and Analgesia by Non Anesthesiologists. Anesthesiology 2002;96:1004-17. [ Links ]
15. Sedation and anesthesia in GI endoscopy. ASGE Guideline. Gastrointest Endosc 2008;68:815-26. [ Links ]
16. López Rosés L. Sedación moderada. En: De la Morena E, Cacho G, editores. Sedación en Endoscopia Digestiva. Madrid: EDIMSA; 2011. p. 111-8. [ Links ]
17. Cohen LB, Delegge MH, Aisenberg J, Brill JV, Inadomi JM, Kochman ML, et al. AGA Institute review of endoscopy sedation. Gastroenterology 2007;133:675-701. [ Links ]
18. Simón MA, Bordas JM, Campo R, González-Huix F, Igea F, Monés J. Documento de consenso de la Asociación Española de Gastroenterología sobre sedoanalgesia en la endoscopia digestiva. Gastroenterol Hepatol 2006;29:131-49. [ Links ]
19. Robertson DJ, Jacobs DP, Mackenzie TA, Oringer JA, Rothstein RI. Clinical trial: A randomized study comparing meperidina (pethidine) and fentanyl in adult gastrointestinal endoscopy. Aliment Pharmacol Ther 2009;29:817-23. [ Links ]
20. Bo LL, Bai Y, Bian JJ, Wen PS, Li JB, Deng XM. Propofol vs traditional sedative agents for endoscopic retrograde cholangiopancreatography: A meta-analysis. World J Gastroenterol 2011;17:3538-43. [ Links ]
21. Qadeer MA, Vargo JJ, Khandwala F, Lopez R, Zuccaro G. Propofol versus traditional sedative agents for gastrointestinal endoscopy: A meta-analysis. Clin Gastroenterol Hepatol 2005;3:1049-56. [ Links ]
22. Igea F, Maestro S, Germade A, Ibáñez M, Castillo RS, Geneux KDJ, et al. Dosificación del propofol en infusión continua: validación de una fórmula de uso útil para todos los pacientes. Comunicación a las XXXV Jornadas de la Sociedad Española de Endoscopia Digestiva. Madrid 14-16 Noviembre, 2013. [ Links ]
23. Chun SY, Kim KO, Park DS, Kim SY, Park JW, Baek IH, et al. Safety and efficacy of deep sedation with propofol alone or combined with midazolam administrated by nonanesthesiologist for gastric endoscopic submucosal dissection. Gut Liver 2012;6:464-70. [ Links ]
24. Julián-Gómez L, Rodríguez-Gómez SJ, Fuentes-Coronel A, Ochoa-Sangrador C, Fradejas-Salazar P, Martín-Garrido E, et al. Ensayo clínico comparando propofol vs. propofol más midazolam en endoscopia digestiva alta diagnóstica: resultados preliminares. Endoscopy 2011;43-A40. [ Links ]
25. Murphy A, Campbell DE, Baines D, Mehr S. Allergic reactions to propofol in egg-allergic children. Anesth Analg 2011;113:140-4. [ Links ]
26. Dumonceau JM, Riphaus A, Aparicio JR, Beilenhoff U, Knape JT, Ortman M, et al. European Society of gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates, and European Society of Anaesthesiology Guideline: Non-anesthesiologist administration of propofol for GI endoscopy. Endoscopy 2010;42:960-74. [ Links ]
27. Külling D, Orlandi M, Inauen W. Propofol sedation during endoscopic procedures: How much staff and monitoring are necessary? Gastrointest Endosc 2007;66:443-9. [ Links ]
28. Jain R, Ikenberry SO, Anderson MA, Appalaneni V, Ben-Menachem T, Decker GA, Fanelli RD, et al. ASGE Standards of Practice Committee. Minimum staffing requirements for the performance of GI endoscopy. Gastrointest Endosc 2010;72:469-70. [ Links ]
29. Vargo JJ. DeLegge MH, Feld AD, Gerstenberger PD, Kwo PY, Lightdale JR, et al. Multisociety sedation curriculum for gastrointestinal endoscopy. Gastrointest Endosc 2012;76: e1-e25. [ Links ]
30. Ramsay MA, Huddleston P, Hamman B, Tai S, Matter G. The patient state index correlates well with the Ramsay sedation score in ICU patients. Anesthesiology 2004;101:A338. [ Links ]
31. Gottlieb KT, Banerjee S, Barth BA, Bhat YM, Desilets DJ, Maple JT, et al. Monitoring equipment for endoscopy. Gastrointest Endosc 2013;77:175-80. [ Links ]
32. King CA, Ogg M. Safe injection practices for administration of propofol. AORN J 2012;95:365-72. [ Links ]
33. Chris JJ, Mulder CJJ, Jacobs MAJ, Leicester RJ, Reddy DN, Shepherd LEA, et al. Guidelines for designing a digestive disease endoscopy unit: Report of the World Endoscopy Organization. Dig Endosc 2013;25:365-75. [ Links ]
34. Lee CK, Lee SH, Chung IK, Lee TH, Park SH, Kim EO, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc 2011;73:206-14. [ Links ]
35. Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc 2007;66:27-34. [ Links ]
36. Cohen LB. Patient monitoring during gastrointestinal endoscopy: Why, when, and how? Gastrointest Endosc Clin N Am 2008;18:651-63. [ Links ]
37. Gonzalez-Huix F, Aldeguer X, Fort E, Salinas E, Figa M, Hombrados M. Sedation without anesthesiologist in 5250 endoscopic procedures: Midazolam vs. midazolam + dolantine vs. propofol. Gastrointestinal Endoscopy 2004;59(Supl.):AB 133. [ Links ]
38. Rex DK, Deenadayalu VP, Eid E, Imperiale TF, Walker JA, Sandhu K, et al. Endoscopist-directed administration of propofol: A worldwide safety experience. Gastroenterology 2009;137:1229-37; quiz 518-9. [ Links ]
39. Agostoni M, Fanti L, Gemma M, Pasculli N, Beretta L, Testoni PA. Adverse events during monitored anesthesia care for GI endoscopy: An 8-year experience. Gastrointest Endosc 2011;74:266-75. [ Links ]
40. Dietrich CG, Kottmann T, Diedrich A, Drouven FM. Sedation-associated complications in endoscopy are not reduced significantly by implementation of the German S-3-guideline and occur in a severe manner only in patients with ASA class III and higher. Scand J Gastroenterol 2013;48:1082-7. [ Links ]
41. Gonzalez-Huix Llado F, Gine Gala JJ, Loras Alastruey C, Martinez Bauer E, Dolz Abadia C, Gomez Oliva C, et al. Position statement of the Catalan Society of Digestology on sedation in gastrointestinal endoscopy. Gastroenterol Hepatol 2012;35:496-511. [ Links ]
42. Rex DK, Heuss LT, Walker JA, Qi R. Trained registered nurses/endoscopy teams can administer propofol safely for endoscopy. Gastroenterology 2005;129:1384-91. [ Links ]
43. Munro J, Booth A, Nicholl J. Routine preoperative testing: A systematic review of the evidence. Health Technol Assessment 1997;1:1-62. [ Links ]
44. Mallampati SR, Gatt SP, Guigino LD, Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anesth Soc J 1985;32:429-34. [ Links ]
45. Vargo JJ, Cohen LB, Rex DK, Kwo PY. Position statement: Non-anesthesiologist administration of propofol for GI endoscopy. Gastrointest Endosc 2009;70:1053-9. [ Links ]
46. Cohen LB, Ladas SD, Vargo JJ, Paspatis D, Bjorkman DJ, Van der Linden, et al. Sedation in digestive endoscopy: The Athens international position statement. Alimentary Pharmacol Ther 2010;32:425-42. [ Links ]
47. Position Statement: Non-anesthesiologist administration of propofol for GI Endoscopy. Gastroenterology 2009;137:2161-7. [ Links ]
48. Ladas SD, Satake Y, Mostafa I, Morse J. Sedation Practices for Gastrointestinal Endoscopy in Europe, North America, Asia, Africa and Australia. Digestion 2010;82:74-6. [ Links ]
49. Lichtenstein DR, Jagannath S, Baron TH, Anderson MA, Benerjee S, Dominitz JA, et al. Sedation and anesthesia in GI endoscopy. Standards of Practice Committee. Gastrointest Endosc 2008;68:815-26. [ Links ]
50. Queshi WA, Rajan E, Adler DG, Davila RE, Hirota WK, Jacobson BC, et al. ASGE Guideline: Guidelines for endoscopy in pregnant and lactating women. Gastrointest Endosc 2005;61:357-62. [ Links ]
51. Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth 1995;7:89-91. [ Links ]
52. Palanisamy A. Maternal anesthesia and fetal neurodevelopment. Int J Obstet Anesth 2012;21:152-62. [ Links ]
53. Shergill AK, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, Evans JA, et al. ASGE Standard of Practice Committee, Guidelines for endoscopy in pregnant and lactating women. Gastrointest Endosc 2012;76:18-24. [ Links ]
54. Cohen-Kerem R, Railton C, Oren D, Lishner M, Koren G. Pregnancy outcome following non-obstetric surgical intervention. Am J Surg 2005;190:467-73. [ Links ]
55. Duncan PG, Pope WD, Cohen MM, Greer N. Fetal risk of anesthesia and surgery during pregnancy. Anesthesiology 1986;64:790-4. [ Links ]
56. Czeizel AE, Pataki T, Rockenbauer M. Reproductive outcome after exposure to surgery under anesthesia during pregnancy. Arch Gynecol Obstet 1998;261:193-9. [ Links ]
57. Konieczko KM, Chapple JC, Nunn JF. Fetotoxic potential of general anaesthesia in relation to pregnancy. Br J Anaesth 1987; 59:449-54. [ Links ]
58. Higuchi H, Adachi Y, Arimura S, Kanno M, Satoh T. Early pregnancy does not reduce the C(50) of propofol for loss of consciousness. Anesth Analg 2001;93:1565-9. [ Links ]
59. Sachs HC; Committee on drugs. The transfer of drugs and therapeutics into human breast milk: An update on selected topics. Pediatrics 2013; 132:e796-809. [ Links ]
60. Nitsun M, Szokol JW, Saleh HJ, Murphy GS, Vender JS, Luong L, et al. Pharmacokinetics of midazolam, propofol, and fentanyl transfer to human breast milk. Clin Pharmacol Ther 2006;79:549-57. [ Links ]
61. Steer PL, Biddle CJ, Marley WS, Lantz RK, Sulik PL. Concentration of fentanyl in colostrum after an analgesic dose. Can J Anaesth 1992;39:231-5. [ Links ]
62. Bar-Oz B, Bulkowstein M, Benyamini L, Greenberg R, Soriano I, Zimmerman D, et al. Use of antibiotic and analgesic drugs during lactation. Drug Saf 2003;26:925-35. [ Links ]
63. Havidich JE, Cravero JP. The current status of procedural sedation for pediatric patients in out-of-operating room locations. Curr Opin Anaesthesiol 2012;25:453-60. [ Links ]
64. Lalwani K, Michel M. Pediatric sedation in North American children's hospitals: A survey of anesthesia providers. Paediatr Anaesth 2005;15:209-13. [ Links ]
65. Doctor K, Roback MG, Teach SJ. An update on pediatric hospital-based sedation. Curr Opin Pediatr 2013;25:310-6. [ Links ]
66. Couloures KG, Beach M, Cravero JP, Monroe KK, Hertzog JH. Impact of provider specialty on pediatric procedural sedation complication rates. Pediatrics 2011;127:e1154-60. [ Links ]
67. van Beek EJ, Leroy PL. Safe and effective procedural sedation for gastrointestinal endoscopy in children. J Pediatr Gastroenterol Nutr 2012;54:171-85. [ Links ]
68. Anderson MA, Baron TH, Banerjee S, Cash BD, Dominitz JA, Lee KK, et al. ASGE standards of practice committee. Modifications in endoscopic practice for pediatric patients. Gastrointest Endosc 2008;67:1-9. [ Links ]
69. Disma N, Astuto M, Rizzo G, Rosano G, Naso P, Aprile G, et al. Propofol sedation with fentanyl or midazolam during oesophagogastroduodenoscopy in children. Eur J Anaesth 2005; 22: 848-52. [ Links ]
70. Paspatis GA, Charoniti I, Manolaraki M, Vardas E, Papanikolaou N, Anastasiadou A, et al. Synergistic sedation with oral midazolam as a premedication and intravenous propofol versus intravenous propofol alone in upper gastrointestinal endoscopies in children: A prospective, randomized study. J Pediatr Gastroenterol Nutr 2006; 43: 195-9. [ Links ]
71. Motamed F, Aminpour Y, Hashemian H, Soltani AE, Najafi M, Farahmand F. Midazolam-ketamine combination for moderate sedation in upper GI endoscopy. J Pediatr Gastroenterol Nutr 2012;54:422-6. [ Links ]
72. Oh JE, Lee HJ, Lee YH. Propofol versus midazolam for sedation during Esophagogastroduodenoscopy in Children. Clin Endosc 2013;46:368-72. [ Links ]
73. Khoshoo V, Thoppil D, Landry L, Brown S, Ross G. Propofol versus midazolam plus meperidine for sedation during ambulatory esophagogastroduodenoscopy. J Pediatr Gastroenterol Nutr 2003;37:146-9. [ Links ]
74. Scheiber G, Ribeiro FC, Karpienski H, Strehl K. Deep sedation with propofol in preschool children undergoing radiation therapy. Paediatr Anaesth. 1996;6:209-13. [ Links ]
75. Buehrer S, Immoos S, Frei M, Timmermann B, Weiss M. Evaluation of propofol for repeated prolonged deep sedation in children undergoing proton radiation therapy. Br J Anaesth 2007;99:556-60. [ Links ]
76. Strauss JM, Giest J. Total intravenous anesthesia. On the way to standard practice in pediatrics. Anaesthesist 2003;52:763-77. [ Links ]
77. Meining A, Semmler V, Kassem AM, Sander R, Frankenberger U, Burzin M, et al. The effect of sedation on the quality of upper gastrointestinal endoscopy: An investigator-blinded, randomized study comparing propofol with midazolam. Endoscopy 2007;39:345-9. [ Links ]
78. Radaelli F, Meucci G, Sgroi G, Minoli G; Italian Association of Hospital Gastroenterologists (AIGO). Technical performance of colonoscopy: The key role of sedation/analgesia and other quality indicators. Am J Gastroenterol 2008;103:1122-30. [ Links ]
79. Zakko SF, Seifert HA, Gross JB. A comparison of midazolam and diazepam for conscious sedation during colonoscopy in a prospective double-blind study. Gastrointest Endosc 1999;49:684-9. [ Links ]
80. Baudet JS, Borque P, Borja E, Alarcón-Fernández O, Sánchez-del-Río A, Campo R, et al. Use of sedation in gastrointestinal endoscopy: A nationwide survey in Spain. Eur J Gastroenterol Hepatol 2009;21:882-8. [ Links ]
81. Dzeletovic I, Harrison ME, Crowell ME, Ramirez FC, Yows CR, Harris LA, et al. Impact of fentanyl in lieu of meperidine on endoscopy unit efficiency: A prospective comparative study in patients undergoing EGD. Gastrointest Endosc 2013;77:883-7. [ Links ]
82. Koshy G, Nair S, Norkus EP, Hertan HI, Pitchumoni CS. Propofol versus midazolam and meperidine for conscious sedation in GI endoscopy. Am J Gastroenterol 2000;95:1476-9. [ Links ]
83. McQuaid KR, Laine L. A systematic review and meta-analysis of randomized, controlled trials of moderate sedation for routine endoscopic procedures. Gastrointest Endosc 2008;67:910-23. [ Links ]
84. Ley básica reguladora de la autonomía del paciente y de derechos y obligaciones en materia de información y documentación clínica. BOE núm. 274 de 15 de Noviembre de 2002. [ Links ]
85. Código de Deontología Médica. Guía de Ética Médica de la Organización Médica Colegial de España (2011) [ Links ]
86. Constitución Española (1978). [ Links ]
87. Ley de 20 de julio de 1955 sobre enseñanza, títulos y ejercicio de las especialidades médicas. [ Links ]
88. Ley de ordenación de las profesiones sanitarias BOE núm. 280 de 22 de Noviembre de 2003. [ Links ]
89. Real Decreto por el que se regula la formación médica especializada y la obtención del título de Médico Especialista. BOE núm. 26, de 31 de enero de 1984. [ Links ]
90. Real Decreto por el que se determinan y clasifican las especialidades en Ciencias de la Salud. BOE núm. 45, de 21 de febrero de 2008. [ Links ]
91. Sentencias de la Sala de lo Contencioso-Administrativo y de lo Penal del Tribunal Supremo y de la Sala Primera del Tribunal Constitucional. [ Links ]
92. Estatutos Generales de la Organización Médica Colegial de España (2012). [ Links ]
93. Artículo 403 del Código Penal Español (1996). [ Links ]
![]() Correspondence:
Correspondence:
Leopoldo López Rosés.
Department of Digestive Diseases.
Hospital Universitario Lucus Augusti.
Avda. Dr. Ulises Romero, s/n.
27003 Lugo, Spain
e-mail: leolopezroses@gmail.com
Received: 06-05-2013
Accepted: 15-07-2013











 texto en
texto en