My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.3 Madrid Mar. 2014
CLINICAL NOTES
Type II intrapancreatic choledochal malignant cyst in adults: Duodenopancreatectomy
Quiste de colédoco tipo II intrapancreático del adulto malignizado: duodenopancreatectomía
Miguel Ángel Jiménez-Ballester1, Victoriano Soria-Aledo1, Juan Gervasio Martín-Lorenzo1, José Ramón Olalla-Muñoz2, Alberto Giménez-Bascuñana3, Eduardo Alcaraz-Mateos3 and José Luis Aguayo-Albasini1
Departments of 1General Surgery, 2Radiology and 3Pathology. Hospital Universitario Morales Meseguer. Campus de Excelencia Internacional "Mare Nostrum". Universidad de Murcia. Murcia, Spain
ABSTRACT
A 62-year-old female patient was admitted for abdominal pain and vomiting. Imaging tests revealed a solid-cystic lesion at the head of the pancreas communicating with the distal bile duct. A Todani type II choledochal cyst was diagnosed with neoplastic degeneration after cytological diagnosis with endoscopic ultrasound-guided puncture. The patient was treated with a cephalic duodenopancreatectomy with curative intention.
Key words: Choledochal cyst. Cancer. Pancreatoduodenectomy.
RESUMEN
Presentamos el caso de una paciente de 62 años que ingresó de urgencias por pancreatitis aguda leve. En las pruebas de imagen se observó una lesión sólido-quística en la cabeza de páncreas comunicante con la vía biliar distal, y se diagnosticó quiste de colédoco tipo II de Todani con degeneración neoplásica en su interior confirmada tras una biopsia por punción en una ecoendoscopia. La paciente fue tratada con una duodenopancreatectomía cefálica con intención curativa.
Palabras clave: Choledochal cyst. Cancer. Pancreatoduodenectomy.
Introduction
Choledochal cysts are a very rare entity in our environment, with an incidence of one in every 2 million. They are more common in females (1-4) and have a higher incidence in Asia (1 in every 150,000 live births).
The classification of choledochal cysts was initially reported by Alonso-Lej (5) in 1959. Today the most commonly used classification is that of Todani et al. (1), which establishes 6 types of choledochal cyst (Table I).
The most frequent types of cyst are I and IV, which make up 80 % of the total (1,4,5); the other types account for less than 5 % each (4,6). The diverticular type, or type II, accounts for 2-3 % of cases (7). Few patients are diagnosed in adulthood and the risk of complications, mainly malignancy, increases with age (7,8).
We report a case of intrahepatic location and proven malignancy which required a cephalic duodenopancreatectomy.
Case report
A 62-year-old woman with no previous history of interest was admitted to emergencies for symptoms of abdominal pain. Laboratory tests including a haemogram, liver function tests (ALT, AST, bilirubin and alkaline phosphatase) and tumour markers (CEA and CA 19.9) were normal.
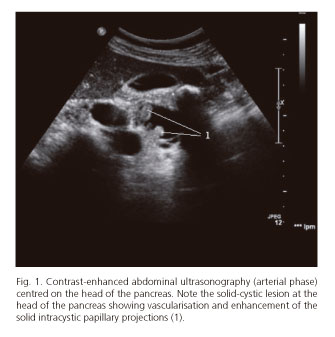
During admission, she underwent abdominal ultrasonography, which revealed a mass with a solid-cystic echo structure, some 4 cm in maximum diameter and intimately related to the common bile duct via a thin pathway (Figs. 1 and 2). The bile duct had a normal calibre, no cholecholedocholithiasis and a slightly dilated main pancreatic duct. The study was completed with a cholangio-NMR (Fig. 3) and abdominal NMR (Fig. 4), with and without i.v. contrast, which confirmed the previous findings of a Todani type II choledochal cyst with probable tumour degeneration.
The thoracic-abdominal-pelvic CT extension study with i.v. contrast did not detect adenopathies or distant metastases. Endoscopic ultrasound-guided fine-needle aspiration was performed. The cytopathological study of the material obtained showed abundant epithelial cellularity, which was atypical and generally arranged in three-dimensional clusters, variably cohesive and often adopting a papillaroid pattern. These were findings compatible with a diagnosis of adenocarcinoma.
With a diagnosis of intracystic neoplastic degeneration we decided on surgical treatment. A midline supra- and infraumbilical laparotomy was performed. No adenopathies or other signs of abdominal neoplastic spread were encountered during the operation. The intrapancreatic choledochal cyst was revealed with a posterior wall intimately related to, but not infiltrating, the superior mesenteric vein. A Whipple cephalic duodenopancreatectomy was performed, which was incident-free. After presenting with severe infection of the central catheter during the postoperative period the patient was discharged at 20 days.
Macroscopic examination of the surgical specimen disclosed a 3.5 cm unilocular cyst formation in the midst of the pancreatic tissue, revealing several polypoid formations at the wall, which were villous in appearance and the largest of which had a maximum diameter of approximately 2.2 cm. The microscopic study showed epithelium with a biliary coating and variable degrees of dysplasia (biliary intraepithelial neoplasia, BilIN), often a high degree (BilIN 3). Additionally, stromal microinfiltration foci were observed. No lymphovascular invasion or perineural infiltration was detected; neither was there involvement of adjacent structures (pancreatic parenchyma, duodenum) or isolated lymph nodes.
Discussion
Choledochal cysts are a very rare pathology in our environment and are mostly diagnosed in childhood or adolescence (only 20-30 % in adults).
The most common symptoms are abdominal pain in the right hypochondrium and jaundice. Adults usually have less florid symptoms, which implies a late diagnosis (5). The classic triad of abdominal pain, jaundice and abdominal tumour presented in 85 % of paediatric patients is a rarity in adults.
Diagnosis of choledochal cyst is established by imaging techniques. Ultrasound and CT usually show a cystic lesion, independent of the gallbladder, located in the subhepatic space between the duodenum and the portal confluence (4,5). As an initial imaging test ultrasound is a useful technique for assessing the biliopancreatic tree, gallbladder and pancreas. Moreover, contrast-enhanced ultrasonography provides real-time information on tumour perfusion and is useful, as in our case, for demonstrating uptake by the small intracystic papillary projections.
Cholangio-NMR is the method of choice for completely mapping the bile duct. It has a high sensitivity and specificity: some 90-100 % and 73-100 % respectively (4). In our case, it enabled the cyst to be characterised.
Malignant transformation is the most serious complication and has a very poor prognosis for survival. It occurs in less than 1 % of paediatric patients and in 10-30 % of adults; it can even reach 50 % in patients aged over 50 years following internal drainage as their only treatment (1,3,8,9).
Todani type I seems to be the most commonly associated with cancer, followed by type IV. The most common site for development of the carcinoma is the wall of the cyst, although it can occur at any level of the biliary tree.
This high probability of complications and malignant degeneration justifies surgery as elective treatment. The best method is complete resection with a biliodigestive anastomosis; simple drainage of the cyst without complete resection is associated with the development of complications and does not reduce the malignancy potential of the disease. Complete resection of the extrahepatic bile duct, together with cholecystectomy, considerably reduces the risk of neoplastic degeneration, which drops to 0.7 % (4).
Bismuth and Krissat (7) found that seven of every eight patients with cancer associated with choledochal cysts had previously been given expectant management with internal drainage or without complete resection of the cyst, which highlights the need to select an adequate treatment once the cyst is diagnosed.
If neoplastic degeneration is shown to affect the distal portion of the bile duct, the usual techniques for treating choledochal cysts, with excision of the cyst or the whole bile duct (depending on the case) and association of a hepaticojejunostomy, are no longer valid (13,14). Metastatic disease must be ruled out initially, as well the absence of infiltration to important adjacent structures such as the portal vein, and surgery must be performed with a curative intention (R0). A Whipple cephalic duodenopancreatectomy with a sufficient safety margin is the technique of choice in cases suspected with neoplastic degeneration of the cyst (12).
Curative resections are associated with a 5-year survival rate of 25-50 %, the primary determinants of these poor results being positive margins and lymph node involvement (11). It is also important to mention the patchy nature of these lesions, as they can occur at other levels of the biliary tree and require appropriate clinical and radiological follow-up.
References
1. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg 1977;134: 263-9. [ Links ]
2. Chaudhary A, Dhar P, Sachdev A, Kumar N, Vij JC, Sarin SK, et al. Choledochal cysts-differences in children and adults. Br J Surg 1996;83:186-8. [ Links ]
3. Martínez-Ordaz JL, Niño-Solis J. Choledochal cysts in adults. Cir Cir 2010;78;61-6. [ Links ]
4. Domínguez-Comesaña E. Dilataciones congénitas de la vía biliar. Revisión de conjunto. Cir Esp 2010;88:285-91. [ Links ]
5. Yamaguchi M. Congenital choledochal cyst: Analysis on 1433 patients in the Japanese literature. Am J Surg 1980;140:653-7. [ Links ]
6. Kianmanesh R, Regimbeau JM, Belghiti J. Anomalies de la junction bilio-pancreatique et dilatations kystiques congénitales des voies biliaires de l'adulte. J Chir 2001;138:196-204. [ Links ]
7. Bismuth H, Krissat J. Choledochal cystic malignancies. Ann Oncol 1999;10:94-8. [ Links ]
8. Watanabe Y, Toki A, Todani T. Bile duct cancer developed after cyst excision for choledochal cyst. J Hepatobiliary Pancreat Surg 1999;6:207-12. [ Links ]
9. Deziel DJ, Rossi RL, Munsosn L, Braasch JW, Silverman ML. Management of bile ducts cystin adults. Arch Surg 1986;121:410-5. [ Links ]
10. Tsuchiya R, Harada N, Ito T. Malignant tumors in choledochal cyst. Ann Surg 1977;186:22-8. [ Links ]
11. Aljiffry M, Walsh MJ, Molinari M. Advances in diagnosis, treatment and palliation of cholangiocarcinoma: 1990-2009. World J Gastroenterol 2009;15:4240-62. [ Links ]
12. Kallel L, Fritsch J, Boytchev I, Cervoni JP, Sauvanet A, Pelletier G. Carcinoma of remaining intrapancreatic bile duct after excision of a choledochal cyst. Gastroenterol Clin Biol. 2006;30:1109-10. [ Links ]
13. Ohashi T, Wakai T, Kubota M, Matsuda Y, Arai Y, Ohyama T, et al. Risk of subsequent biliary malignancy in patients undergoing cyst excision for congenital choledochal cysts. J Gastroenterol Hepatol 2013;28:243-7. [ Links ]
14. Park SW, Lee SH, Eum YO, Oh HS, Lee D, Jin E, et al. One case of common bile duct cancer mimicking cystic neoplasm of the pancreas, arising 9 years after excision of a choledochal cyst. Clin Endosc 2012;45:435-9. [ Links ]
![]() Correspondence:
Correspondence:
Miguel Ángel Jiménez Ballester.
Servicio de Cirugía General y Aparato Digestivo.
Hospital Universitario Morales Meseguer.
Avda. Marqués de los Vélez, s/n.
30008 Murcia, Spain
e-mail: majb8a@gmail.com
Received: 14-03-2013
Accepted: 10-06-2013











 text in
text in