My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.4 Madrid Apr. 2014
A Spanish multicenter study to estimate the prevalence and incidence of chronic pancreatitis and its complications
Estudio español multicéntrico de estimación de la prevalencia e incidencia de la pancreatitis crónica y sus complicaciones
J. Enrique Domínguez-Muñoz1, Alfredo Lucendo2, L. Fernando Carballo3, Julio Iglesias-García1, and José María Tenías4 on behalf of the Working Group on Pancreatic Diseases, Spanish Society of Gastroenterology (SEPD)
1Department of Digestive Diseases. Complejo Hospitalario Universitario de Santiago. Santiago de Compostela, A Coruña. Spain
2Department of Digestive Diseases. Hospital General de Tomelloso. Ciudad Real, Spain
3Department of Digestive Diseases. Hospital Clínico Universitario Virgen de la Arrixaca. Murcia, Spain
4Research Unit. Hospital General La Mancha-Centro. Alcázar de San Juan. Ciudad Real, Spain
ABSTRACT
Background and objective: No nation-wide epidemiological study on the incidence and prevalence of chronic pancreatitis (CP) had been thus far carried out in Spain. Our goal is to estimate the prevalence and incidence of CP, as well as to determine the diagnostic and therapeutic criteria used in Spanish pancreas units.
Methods: An observarional, descriptive study of hospital pancreas units in Spain. CP-related epidemiology, etiology, manifestations, diagnostic tests, functional complications, and treatments were all assessed using a structured questionnaire. Overall results were estimated by weighting cases in each site.
Results: Information was collected from six pancreas units with a sample frame of 1,900,751 inhabitants. Overall prevalence was 49.3 cases per 105 population (95 % CI, 46 to 52) and incidence was 5.5 cases per 105 inhabitant-years (95 % CI, 5.4 to 5.6). Most common etiologies included tobacco and alcoholism, which were associated with three in every four cases. The most prevalent symptoms were recurring pain (48.8 %) and chronic abdominal pain (30.6 %). The most widely used diagnostic method was echoendoscopy (79.8 %), CT (computerized tomography) (58.7 %), and MRI (magnetic resonance imaging)/MRCP (magnetic resonance cholangiopancreatography) (55.9 %). Most prevalent morphologic findings included calcifications (35 %) and pseudocysts (27 %). Exocrine (38.8 %) and endocrine (35.2 %) pancreatic insufficiency had both a similar frequency. Treatments used were rather heterogeneous among sites, with enzyme replacement therapy (40.7 %) and insulin (30.9 %) being most commonly used.
Conclusions: Pancreas units amass a significant number of both prevalent and incident CP cases. Patients seen in these units share a similar typology, and differences between units are greater regarding diagnostic and therapeutic strategies.
Key words: Chronic pancreatitis. Sanitary surveys. Hospital units.
RESUMEN
Antecedentes y propósito: en España no se ha llevado a cabo hasta ahora ningún estudio epidemiológico nacional sobre la incidencia y prevalencia de la pancreatitis crónica (PC). El objetivo es estimar la prevalencia e incidencia de casos de PC, así como los criterios diagnósticos y terapéuticos utilizados en las unidades de páncreas españolas.
Métodos: estudio observacional, descriptivo de las unidades de páncreas de ámbito hospitalario en España. Mediante un cuestionario estructurado se valoró la epidemiología de la PC, la etiología, sintomatología, pruebas diagnósticas, complicaciones funcionales y los tratamientos utilizados. Los resultados globales se estimaron mediante la ponderación por la casuística de cada centro.
Resultados: se recopiló información de seis unidades de páncreas, con un marco muestral de 1.900.751 habitantes. La prevalencia global fue de 49,3 casos por 105 habitantes (IC95 % 46 a 52) y la incidencia de 5,5 casos por 105 habitantes-año (IC95 % 5,4 a 5,6). Las etiologías más frecuentes fueron el tabaco y el alcoholismo que se asociaron a tres de cada cuatro casos. La sintomatología más prevalente fue el dolor recidivante (48,8 %), seguido del dolor abdominal crónico (30,6 %). El método diagnóstico más utilizado fue la ecoendoscopia (79,8 %), la TC (tomografía computerizada) (58,7 %) y la RNM (resonancia magnética)/CPRM (colangiopancreatografía por resonancia magnética) (55,9 %). Los hallazgos morfológicos más prevalentes fueron las calcificaciones (35 %) y pseudoquistes (27 %). Se presentaron con una frecuencia similar la insuficiencia pancreática exocrina (38,8 %) y la endocrina (35,2 %). Los tratamientos utilizados fueron bastante heterogéneos entre centros, siendo los más frecuentemente usados el tratamiento enzimático sustitutivo (40,7 %) y la insulina (30,9 %).
Conclusiones: las unidades especializadas del páncreas acumulan un importante número de casos prevalentes e incidentes de PC. La tipología del paciente atendido en estas unidades es similar con mayores diferencias entre unidades en los métodos diagnósticos y terapéuticos utilizados.
Palabras clave: Pancreatitis crónica. Encuestas sanitarias. Unidades hospitalarias.
Introduction
In a recent review (1) on the epidemiology and socioeconomic impact of chronic pancreatitis (CP), the authors noted the scarcity of multicenter studies estimating the incidence and prevalence of this disease in a defined, representative population. Results to this day showed a wide heterogeneity in prevalence and incidence figures according to region and study date. Problems regarding epidemiologic studies on CP are emphasized by difficulties in establishing a definite diagnosis of the condition, which render chronic pancreatitis a clearly underdiagnosed disease.
As of today 14 multicenter studies have been published, particularly in European (2-9) and Asian (10-14) countries, with only one reported in the US (15). Of all 14 studies, six used the hospital registries available in their countries as information source (1,2,5,7,9,15).
Overall, the annual incidence of CP per 100,000 population is 6 to 7 cases in Europe, 7 to 8 cases in the United States, and 5 to 14.4 cases in Asia (only Japan provides incidence values) (11,12). As regards CP, prevalence is more variable than incidence, even in the same country: China has figures ranging from 3.1 to 13.5 cases per 105 population (14). The prevalence in Japan is estimated as 35.5 cases per 105 population (11), and in Europe oscillates between 13 cases per 105 population in Finland (3) and 26.4 cases per 105 population in France (6). These data reflect the difficulties entailed by CP diagnosis and long-term patient follow-up.
While the incidence of CP may be relatively well estimated based on patients admitted for flare-ups or through databases at endoscopy or radiology units (computed tomography, magnetic resonance pancreatography), its prevalence is definitely challenging. In fact, many of these patients are not followed up by hospital departments but by primary care practitioners, which renders these patients less visible for epidemiologic studies. Bearing in mind that the mean survival of patients diagnosed with CP is 20 years (16,17), reported prevalence figures -between 3 and 35 cases per 105 inhabitants- are far removed from the values expected for a reported incidence of 5 to 14 cases per 105 inhabitants per year.
No nation-wide epidemiologic study has been thus far performed in Spain on the incidence and prevalence of CP. The Sociedad Española de Patología Digestiva (SEPD) has established a CP task force with the goal of promoting the setup of a prospective registry of patients in order to estimate the incidence and prevalence of the disease, to characterize the diagnostic criteria used in its identification, and to explore associations with a variety of risk factors.
A multicenter survey of Spanish hospitals with specific pancreatic health care services was initially performed to estimate the prevalence and incidence of attended chronic pancreatitis patients, as well as the diagnostic and therapeutic criteria used.
Material and methods
Study design
An observational, descriptive study of hospital pancreas units in Spain.
Inclusion criteria
Units specialized in the health care of pancreatic conditions for at least 5 years were included, regardless of their organic dependence on gastroenterology departments.
Measurements
The following domains were assessed with a structured 16-item questionnaire:
- Epidemiology of chronic pancreatitis in the geographic areas served by each hospital: The number of both currently identified patients (prevalent cases) and of patients identified in 2011 (incident cases) was estimated. Prevalence and incidence were estimated according to population size in each reference area. Similarly, mortality in the same period -both related to chronic pancreatitis and from all causes- was also estimated.
- Chronic pancreatitis etiology: Each respondent provided the frequency of the various chronic pancreatitis etiologies identified for the patients cared for in their unit. The following etiologies were distinguished in accordance to the TIGAR-O etiopathogenic classification (18): Toxic (alcohol and/or tobacco), hereditary (PRSS1), genetic because of SPINK1 or CFTR mutation, autoimmune, obstructive, severe and/or recurring acute pancreatitis, metabolic (CRF, hypercalcemia), and idiopathic.
- Manifestations: The most prevalent presentation among attended patients was estimated according to symptom frequency.
- Diagnostic procedures used: Abdominal ultrasounds, CT, MRI/MRCP, echoendoscopy (EUS), fecal elastase, and other. These procedure are not exclusive, hence more than one may be used for a given patient.
- Local complications: The proportion of patients developing pseudocysts, biliary stenosis, duodenal stenosis, and vascular complications (thrombosis of the porto-splenic axis and pseudoaneurysm) was collected. In addition, the frequency of chronic calcifying pancreatitis as a token of advanced disease was specifically probed.
- Functional complications: The prevalence of exocrine and/or endocrine insufficiency was calculated based on the methods usually applied by each site.
- Frequency of use for various therapeutic approaches: Including the drug therapies, endoscopic treatments, and surgical procedures available for these patients.
Data analysis strategy
Epidemiologic data were estimated according to the area served by each institution. Prevalence and incidence estimates for chronic pancreatitis were expressed as cases per 100,000 inhabitants, with the corresponding 95 % confidence intervals.
Clinical characteristics were reported as relative frequencies (%) for ach site, and using weights related to patient numbers in overall calculations.
Calculations were performed using the PSW 18.0 (SPSS Inc) and EPIDAT 3.1 (OPS/Xunta de Galicia) software packages.
Results
Six pancreas units were recruited with a global sample frame of 1,900,751 inhabitants (Fig. 1). The overall prevalence was 49.3 cases per 105 inhabitants (95 % CI: 46 to 52 cases per 105 inhabitants), with a variance of 25 to 85 cases per 105 inhabitants among units (Table I). Incidence in 2011 involved 5.5 cases per 105 inhabitants per year (95 % CI: 5.4 to 5.6 per 105 inhabitants per year) with variations that paralleled those seen regarding prevalence. Disease-related mortality was low (8 cases: 0.8 %), and mortality from other causes was slightly higher (26 cases: 2.8 %).
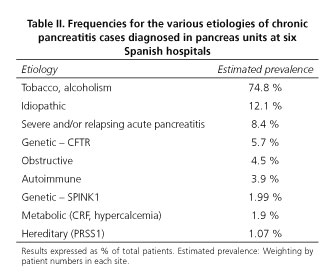
The etiological distribution of cases does not differ significantly between sites. Thus, the most common etiology was toxicity (tobacco and/or alcohol), which was considered to be the cause of disease for three in every four chronic pancreatitis patients. The remaining etiologies were much less common, as shown in table II. The cause of disease cannot be established in 12.1 % of cases (idiopathic chronic pancreatitis).
Most prevalent symptoms included recurring pain, with flare-ups (48.8 %) and painless periods in between, followed by chronic abdominal pain (30.6 %). Chronic diarrhea, as a symptom consistent with exocrine pancreatic insufficiency, is seen in around one in every five patients (21.5 %). On the other hand, 4.7 % of patients manifest vomiting.
The extent to which diagnostic confirmation methods were used was highly heterogeneous from one unit to the next (Fig. 2). The most commonly used approach was EUS (weighted frequency of 79.8 %), followed by CT (58.7 %), MRI/MRCP (55.9 %), fecal elastase testing (43.1 %), and abdominal ultrasounds (38.7 %).
Most prevalent local complications included calcifications (35 %) and pseudocysts (27 %) (Table III). Among functional complications exocrine (38.8 %) and endocrine (35.2 %) pancreatic insufficiency occurred with a similar rate.
In addition to replacement therapies for exocrine and endocrine pancreatic insufficiency, 21.7 % of patients received opioid painkillers, 20.2 % required some sort of surgical procedure, whether bypassing or resective, and 9.4 % of patients underwent some sort of endoscopic treatment (Table IV).
Discussion
We report here the data from a multicenter survey to assess the epidemiology and clinical management of chronic pancreatitis patients in Spanish institutions with specific pancreas units. In this paper we show that, despite its being restricted to monographic units in one country, both the incidence and most particularly the prevalence of chronic pancreatitis is significantly variable. Alcohol ingestion and tobacco smoking represent the risk factor most commonly associated with the disease, which most commonly presents with abdominal pain, whether relapsing or chronic. A high percentage of patients cared for in specialized pancreas units in our country have complications and both structural and functional evidence of advanced disease. Lastly, heterogeneity is significant regarding diagnostic procedures and therapeutic approaches among the various sites.
Chronic pancreatitis is clearly an underdiagnosed condition. Most diagnostic criteria considered specific for the disease, including duct irregularity and dilation, parenchymal atrophy, calcifications, and pseudocysts, are late findings, hence early chronic pancreatitis is currently an uncommon diagnosis. On the other hand, symptoms such as epigastric pain, dyspepsia, or an irritable bowel-like syndrome are nonspecific and require a high degree of suspicion in order to establish a diagnosis (19,20). This accounts for the fact that, even in the specialized pancreas units included in the study, most diagnosed patients present with recurring pain in the setting of exacerbations, where diagnostic suspicion is straightforward. On the other hand, the presence of risk factors for chronic pancreatitis also increases suspicion, and therefore renders diagnosis easier. This is why, in the present study, most cases are associated with alcohol drinking and tobacco smoking, whereas recent series in other countries reveal lower rates of toxic etiologies as the etiopathogenic understanding of the disease increases (21-24). The result of the diagnostic challenge still entailed by chronic pancreatitis is the differing prevalence in surveyed areas, which oscillates from 25 to 86 cases per 100,000 population with no differences in toxic or dietary habits to account for it. Furthermore, considering that mean survival is 20 years following a diagnosis with chronic pancreatitis, the incidence of 5.5 cases per 105 inhabitants per year is associated with a prior prevalence of 110 cases per 105 inhabitants, which is clearly higher than found in the present study.
Compared to prior studies in other countries, our results are similar regarding incidence though clearly higher for prevalence (1-15). In the study by Levy et al. (6), which because of its design and its being performed in a country akin to ours may be considered most appropriate for a comparison with our findings, the authors requested from a significant proportion of French gastroenterologists information on the number of visits for chronic pancreatitis during a 3-month period, and the number of newly diagnosed cases during the same lapse. Whereas the estimated incidence of the condition was 7.8 cases per 105 inhabitants per year, superior to that in the present study, the prevalence was clearly lower at only 26.4 cases per 105 inhabitants (6). This divergence is at least partly accounted for by the sample of surveyed specialists in each study, general gastroenterologists in the study by Levy versus specific pancreas unit specialists in our research, which entails varying adherence to patient follow-up. It must be highlighted that, despite its likely being inferior to actual figures, the prevalence found in the present study is more in accordance with incidence figures as compared to the study by Levy and colleagues (6), hence they most probably represent the actual prevalence of this condition more accurately.
Of note in the present study is the fact that, despite the availability of national clinical guidelines on this disease (25,26) and the inclusion of only specialized pancreas units, the use of diagnostic procedures is highly variable. In fact, methods such as abdominal sonography, abdominal CT or fecal elastase testing are used for 100 % of patients in some centers but hardly ever or never in others. This reflects distinct habits and protocols for the diagnostic approach of this disease, besides a different availability of the various methods. However, none of the above methods is highly sensitive for the diagnosis of chronic pancreatitis, particularly in non-advanced stages (27,28). Therefore, the variability of methods considered nowadays of choice for the diagnosis of non-calcifying chronic pancreatitis, including MRCP/MRI and EUS (29-33), which are used with a range of 22 % to 100 % and 50 % to 92 %, respectively, is even more remarkable. Anyway, since the effectiveness of both tests is superimposable in expert groups, the use of either one likely reflects their availability in each of the participating centers. As these centers were chosen because of their experience and patient load as regards this disease, such variability demonstrates there is a need for clinical guidelines on the diagnosis of chronic pancreatitis, both to enhance clinical suspicion and to help use appropriate diagnostic procedures.
Similarly to the above regarding diagnosis, the therapeutic approach is highly divergent from one site to the next. This is less obvious regarding the use of pancreatic enzymes and insulin to treat exocrine and endocrine pancreatic insufficiency than in pain management. In this regard, the frequent use of opioid analgesics is inversely proportional to the frequency of surgery, which is most likely related to the expertise of each center's surgical team in the management of this condition. Also noteworthy is the low frequency of the endoscopic approach for these patients, lower than 10 %, with only two centers using this procedure more routinely (in 19.7 % and 26.7 % of patients, respectively). This fact is surely consistent with the expertise of endoscopy teams regarding therapeutic pancreatic endoscopy, as well as the increasingly higher frequency of conservative management choices for these patients.
The primary limitation of the present study is its observational design based on data collection via a questionnaire, which may result in some information bias. Most data were provided by each unit's head, and their quality and accuracy greatly depend on the availability of local registries to facilitate data collection. Nevertheless, regarding unexpected or conflicting data we contacted the provider for confirmation or amendment. Furthermore, restricting the study to centers with highly experienced pancreas units should result in highly accurate figures for our country's population. Finally, this study methodology has been commonly applied in prior epidemiological studies on chronic pancreatitis.
Our results provide highly relevant information for the understanding of chronic pancreatitis in Spain. On the one hand, they should serve as reference for centers and regions with no or newly set up pancreas units. On the other hand, they show the relevant effort still needed to make knowledge on this condition widespread. The significant inter-unit variability of results, both in the epidemiological and clinical practice aspects, reveals a need for the development of chronic pancreatitis-specific clinical practice guidelines. Furthermore, results are compelling as regards the need to increase awareness and diagnostic suspicion in order to solve, to the extent possible, the relevant underdiagnosis of this disease.
To conclude, chronic pancreatitis is a disease that in our setting has a prevalence of 55.8 cases per 100,000 inhabitants. Alcohol drinking and tobacco use are the most commonly associated risk factors, and may help increase the degree of diagnostic suspicion. Variability in diagnostic and therapeutic approaches is significant among pancreas units in our country, which reveals a need for the development of disease-specific clinical practice guidelines.
Other members of the working group on pancreatic diseases, Spanish Society of Gastroenterology (SEPD)
- José Lariño-Noia. Servicio de Aparato Digestivo. Complejo Hospitalario Universitario de Santiago. Santiago de Compostela, A Coruña. Spain.
- Ángeles Pérez Aisa. Agencia Sanitaria Costa del Sol. Marbella, Málaga. Spain.
- Isabel Pascual. Hospital Clínico de Valencia. Valencia, Spain.
- Carlos Marra-López. Hospital Universitario Araba - Sede Txagorritxu. Vitoria, Álava. Spain.
- Aurelio López-Martín. Hospital Universitario Morales Meseguer. Murcia, Spain.
- Enrique de Madaria. Hospital General Universitario de Alicante. Alicante, Spain.
References
1. Jupp J, Fine D, Johnson CD. The epidemiology and socioeconomic impact of chronic pancreatitis. Best Practice & Research Clinical Gastroenterology 2010; 24:219-31. [ Links ]
2. Johnson CD, Hosking S. National statistics for diet, alcohol consumption, and chronic pancreatitis in England and Wales, 1960-88. Gut 1991;32:1401-5. [ Links ]
3. Jaakkola M, Nordback I. Pancreatitis in Finland between 1970 and 1989. Gut 1993;34:1255-60. [ Links ]
4. Dite P, Stary K, Novotny I, Precechtelova M, Dolina J, Lata J, et al. Incidence of chronic pancreatitis in the Czech Republic. European Journal of Gastroenterology & Hepatology 2001;13:749-50. [ Links ]
5. Tinto A, Lloyd DA, Kang JY, Majeed A, Ellis C, Williamson RC, et al. Acute and chronic pancreatitis-diseases on the rise: A study of hospital admissions in England 1989/90-1999/2000. Aliment Pharmacol Ther 2002;16:2097-105. [ Links ]
6. Levy P, Barthet M, Mollard BR, Amouretti M, Marion-Audibert AM, Dyard F. Estimation of the prevalence and incidence of chronic pancreatitis and its complications. Gastroenterologie Clinique et Biologique 2006;30:838-44. [ Links ]
7. Spanier BW, Dijkgraaf MG, Bruno MJ. Trends and forecasts of hospital admissions for acute and chronic pancreatitis in the Netherlands. European Journal of Gastroenterology & Hepatology 2008;20:653-8. [ Links ]
8. Frulloni L, Gabbrielli A, Pezzilli R, Zerbi A, Cavestro GM, Marotta F, et al. Chronic pancreatitis: Report from a multicenter Italian survey (PanCroInfAISP) on 893 patients. Dig Liver Dis 2009;41:311-7. [ Links ]
9. Joergensen M, Brusgaard K, Cruger DG, Gerdes AM, de Muckadell OB. Incidence, prevalence, etiology, and prognosis of first-time chronic pancreatitis in young patients: A nationwide cohort study. Dig Dis Sci 2010;55:2988-98. [ Links ]
10. Ryu JK, Lee JK, Kim YT, Lee DK, Seo DW, Lee KT, et al. Clinical features of chronic pancreatitis in Korea: a multicenter nationwide study. Digestion 2005;72:207-11. [ Links ]
11. Otsuki M, Tashiro M. 4. Chronic pancreatitis and pancreatic cancer, lifestyle-related diseases. Internal Medicine 2007;46:109-13. [ Links ]
12. Nishimori I, Tamakoshi A, Otsuki M, Research Committee on Intractable Diseases of the Pancreas MoHL, Welfare of J. Prevalence of autoimmune pancreatitis in Japan from a nationwide survey in 2002. Journal of Gastroenterology 2007;42(Supl. 18):6-8. [ Links ]
13. Balakrishnan V, Unnikrishnan AG, Thomas V, Choudhuri G, Veeraraju P, Singh SP, et al. Chronic pancreatitis. A prospective nationwide study of 1,086 subjects from India. JOP 2008;9:593-600. [ Links ]
14. Wang LW, Li ZS, Li SD, Jin ZD, Zou DW, Chen F. Prevalence and clinical features of chronic pancreatitis in China: a retrospective multicenter analysis over 10 years. Pancreas 2009;38:248-54. [ Links ]
15. Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Archives of Internal Medicine 2008;168:649-56. [ Links ]
16. Lowenfels AB, Maisonneuve P, Cavallini G, Ammann RW, Lankisch PG, Andersen JR, et al. Prognosis of chronic pancreatitis: an international multicenter study. International Pancreatitis Study Group. Am J Gastroenterol 1994;89:1467-71. [ Links ]
17. Lankisch PG, Lohr-Happe A, Otto J, Creutzfeldt W. Natural course in chronic pancreatitis. Pain, exocrine and endocrine pancreatic insufficiency and prognosis of the disease. Digestion 1993;54:148-55. [ Links ]
18. Etemad B, Whitcomb DC. Chronic pancreatitis: Diagnosis, classification, and new genetic developments. Gastroenterology 2001;120:682-707. [ Links ]
19. Leeds JS, Hopper AD, Sidhu R, Simmonette A, Azadbakht N, Hoggard N, et al. Some patients with irritable bowel syndrome may have exocrine pancreatic insufficiency. Clin Gastroenterol Hepatol 2010;8:433-8. [ Links ]
20. Lee YT, Lai AC, Hui Y, Wu JC, Leung VK, Chan FK, et al. EUS in the management of uninvestigated dyspepsia. Gastrointest Endosc 2002;56:842-8. [ Links ]
21. Masson E, Chen JM, Audrezet MP, Cooper DN, Ferec C. A conservative assessment of the major genetic causes of idiopathic chronic pancreatitis: Data from a comprehensive analysis of PRSS1, SPINK1, CTRC and CFTR genes in 253 young French patients. PloS one 2013;8:e73522. [ Links ]
22. Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 2013;144:1252-61. [ Links ]
23. Spicak J, Pulkertova A, Kralova-Lesna I, Suchanek P, Vitaskova M, Adamkova V. Alcoholic chronic pancreatitis and liver cirrhosis: Coincidence and differences in lifestyle. Pancreatology 2012;12:311-6. [ Links ]
24. Lowenfels AB, Maisonneuve P. Defining the role of smoking in chronic pancreatitis. Clin Gastroenterol Hepatol 2011;9:196-7. [ Links ]
25. Martinez J, Abad-Gonzalez A, Aparicio JR, Aparisi L, Boadas J, Boix E, et al. The Spanish Pancreatic Club recommendations for the diagnosis and treatment of chronic pancreatitis: part 1 (diagnosis). Pancreatology 2013;13:8-17. [ Links ]
26. de-Madaria E, Abad-Gonzalez A, Aparicio JR, Aparisi L, Boadas J, Boix E, et al. The Spanish Pancreatic Club's recommendations for the diagnosis and treatment of chronic pancreatitis: Part 2 (treatment). Pancreatology 2013;13:18-28. [ Links ]
27. Dominguez Munoz JE. Diagnosis of chronic pancreatitis: Functional testing. Best Practice & Research Clinical Gastroenterology 2010;24:233-41. [ Links ]
28. Choueiri NE, Balci NC, Alkaade S, Burton FR. Advanced imaging of chronic pancreatitis. Curr Gastroenterol Rep 2010;12:114-20. [ Links ]
29. Catalano MF, Sahai A, Levy M, Romagnuolo J, Wiersema M, Brugge W, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: The Rosemont Classification. Gastrointest Endosc 2009;69:1251-61. [ Links ]
30. Balci C. MRI assessment of chronic pancreatitis. Diagnostic and Interventional Radiology 2011;17:249-54. [ Links ]
31. Iglesias-Garcia J, Dominguez-Munoz JE, Castineira-Alvarino M, Luaces-Regueira M, Larino-Noia J. Quantitative elastography associated with endoscopic ultrasound for the diagnosis of chronic pancreatitis. Endoscopy 2013;45:781-8. [ Links ]
32. Stevens T. Role of endoscopic ultrasonography in the diagnosis of acute and chronic pancreatitis. Gastrointest Endosc Clin N Am 2013;23:735-47. [ Links ]
33. Iglesias-Garcia J, Lindkvist B, Larino-Noia J, Dominguez-Munoz JE. The role of EUS in relation to other imaging modalities in the differential diagnosis between mass forming chronic pancreatitis, autoimmune pancreatitis and ductal pancreatic adenocarcinoma. Rev Esp Enferm Dig 2012;104:315-21. [ Links ]
![]() Correspondence:
Correspondence:
J. Enrique Domínguez-Muñoz
Department of Digestive Diseases
Hospital Clínico Universitario de Santiago
c/ Choupana, s/n
15706 Santiago de Compostela
A Coruña, Spain
e-mail: enriquedominguezmunoz@hotmail.com
Received 13-06-2014
Accepted 24-06-2014











 text in
text in