Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.4 Madrid abr. 2014
Peri-ileostomy pyoderma gangrenosum. Case report
Pioderma gangrenoso peri-ileostomía
Carlos Cerdán-Santacruz1, María Rosario Caparrós-Sanz2, Margarita Lancharro-Bermúdez2, Juan Luis Mendoza-Hernández3 and Javier Cerdán-Miguel1
1Colorectal Surgery. General Surgery Department. Clínica Santa Elena. Madrid, Spain
2Stoma Therapy Unit. Hospital Clínico San Carlos. Madrid, Spain
3Gastroenterology Department. Inflammatory Bowel Disease Unit. Hospital Clínico San Carlos. Instituto de Investigación Sanitaria del Hospital Clínico San Carlos (IdISSC). Madrid, Spain
ABSTRACT
Pyoderma gangrenosum is one of the most severe complications that can occur following stoma placement. Despite few cases reported in the literature, it is considered an underdiagnosed entity.
We present a case of peri-ileostomy pyoderma gangrenosum (PPG) in a patient who underwent a pancoloproctectomy and permanent ileostomy due to ulcerative colitis (UC).
Treatment was based on local cures, proper fitting of ostomy devices, topical tacrolimus and systemic corticosteroids, adalimumab and antibiotics. Satisfactory resolution was achieved in eight weeks.
Key words: Inflammatory bowel disease. Ulcerative colitis. Crohn's disease. Pyoderma ganrenosum. Stoma.
RESUMEN
El pioderma gangrenoso es una de las complicaciones más graves que se pueden presentar tras la realización de un estoma. A pesar de los pocos casos descritos en la literatura, se considera que está infradiagnosticado.
Se presenta un caso de pioderma gangrenoso peri-ileostomía en una paciente sometida a pancoloproctectomía e ileostomía definitiva por colitis ulcerosa.
El tratamiento se basó en curas locales, adecuación de los dispositivos colectores, aplicación tópica de tacrolimus y administración sistémica de corticoides, adalimumab y antibióticos. La curación se produjo en ocho semanas de manera satisfactoria.
Palabras clave: Enfermedad inflamatoria intestinal. Colitis ulcerosa. Enfermedad de Crohn. Pioderma gangrenoso. Estoma.
Introduction
Peri-ileostomy pyoderma gangrenosum (PPG) is one of the most severe complications that can occur following stoma placement. It is estimated that constitutes 15 % of all kinds of pyoderma gangrenosum (PG) (1-3).
Described by McGarity (4) in 1984 in three patients with Crohn's disease (CD), it is considered to be a rare lesion with less than 60 cases published up to 2012 (5). However, it is considered to be an underdiagnosed entity due to lack of knowledge or confusion with other peristomal dermatological lesions (3,4,6-8). The diagnosis is mainly clinical; therefore it is important for surgeons, gastroenterologists and stoma therapists to know how to identify it in order to start treatment as soon as possible.
We present a case of PPG that occurred in a patient after undergoing a pancoloproctectomy due to ulcerative colitis (UC) that was refractory to medical treatment.
Case report
46-year-old female with previous history of hypothyroidism secondary to Graves-Basedow disease, rheumatoid arthritis and corticosteroid-dependent UC that was refractory to treatment with thiopurine immunosuppressant drugs and anti-TNF. Other associated complications were erythema nodosum and perianal disease that required abscess drainage and a loose seton placement one year early.
The patient, being followed up in the Inflammatory Bowel Disease (IBD) Unit, was refractory to treatment, with evident endoscopic and histological lesions in addition with significant involvement of overall conditions and quality of life, so surgical treatment was recommended. Given the perianal disease, a pancoloproctectomy and end ileostomy in the right iliac fossa was performed. Pathologic study of the specimen confirmed the diagnosis of UC.
Postoperative course complicated with a urinary tract infection and paralytic ileus that required a nasogastric tube placement.
Thiopurine and anti-TNF treatment was discontinued after surgery and the patient was weaned off corticosteroids. The patient was discharged asymptomatic 35 days after the intervention.
Seven days later, the patient came in to the stoma therapy clinic presenting ulceration of anfractuous borders and a subcutaneous abscess in the vicinity of the stoma that caused intense pain and difficulty for the application of the ostomy device.
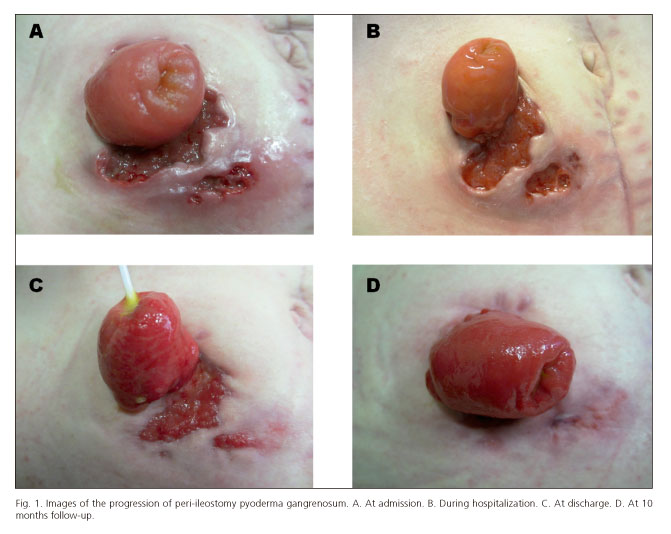
Physical examination revealed a deep ulceration, with irregular and indurated edges, extremely painful, affecting a large part of the medial border of the stoma. In proximity, there was a small purulent collection that revealed another ulceration upon drainage, necrotic erythematous margins, tunneled by a small dermal bridge to the previous ulceration (Fig. 1A).
The patient was diagnosed with PPG and admitted for treatment and monitoring.
Samples were taken for culture and histological study. No abnormal organisms were found and the pathology study reported nonspecific inflammation.
Treatment was started with topical tacrolimus in a 0.3 %, solution applied once daily; adalimumab: 80 mg induction dose followed by 40 mg subcutaneously every two weeks for maintenance; methylprednisolone: 32 mg orally on a tapered regimen of 8 mg every 14 days; and metronidazole and ciprofloxacin at regular dosages for two weeks.
In addition to general treatment, local dressing changes were carried out by the Stoma Therapy Unit by applying a transparent hydrocolloid absorbent pad (carboxymethylcellulose and polyurethane film), over which a double system ileostomy device with drawstring was fitted, with daily changes for application of topical tacrolimus.
Clinical progress was satisfactory with complete resolution of the pyoderma at eight weeks of treatment (Figs. 1. B-D). The patient was seen in outpatient follow-up. The lesions had disappeared ten months later and the patient did not require maintenance medical therapy.
Discussion
Development of PPG represents one of the most severe stoma complications due to significant local involvement, difficulty in managing ostomy devices and the severe impact on the patient's quality of life, as well as to the torpid progress and resistance to treatment.
The time of onset varies from a few days to 25 years after placement of the stoma (3,7-9). Uchino (5) describes two types of PPG: "R" type, explosive, fast-spreading, that develops within six days after surgery and mainly occurs in UC, and "G" type, which is indolent, slowly progressive appearing within an average of 52 days found preferably in CD. Uchino The author states that this division should have therapeutic implications.
The etiopathogenesis is unknown. It is more frequent in women (1,2,7,8), though the reason for this predominance is not known. The normal age of onset is between 20 and 50 years of age (1,7,9); it is uncommon prior to 18 years of age and can also occur in the elderly (10). 70 % of cases occur related to ileostomies (1,6).
Initially associated with inflammatory bowel disease (IBD), it is estimated to occur between 1.5 and 4.3 % of individuals requiring a stoma (2-5, 8-11); it has also been confirmed in other processes such as diverticulitis, abdominal neoplasms and neurological disorders (1,6). Although it is more common in CD, there is no unanimity on its predominance over UC.
The phenomenon of pathergy has also been postulated as a possible explanation, caused by repeated microtraumatisms to the peristomal skin during cleaning and changing the ostomy device, in addition to an autoimmune problem associated with IBD (3-5,7).
Cultures do not reveal any pathogen apart from normal dermal and fecal flora.
Many attempts have been made to identify risk factors for its development, although it has happened to be a very difficult task given most of published data come from isolated case reports or retrospective reviews that encompass many years. Among subjects with IBD, Wu (1) found a higher incidence of PPG in women, those with autoimmune disorders and high body mass index (BMI).
Macroscopically, PPG consists of tender inflammatory ulceration that starts as pustules or erythematous papules that rapidly ulcerate and grow with irregular erythematous and indurated margins that lead to several ulcerated foci with necrotic beds that form interconnected fistula tracts (5,8,9,12).
This characteristic appearance allows the early diagnosis, as in our case, and treatment to be started immediately. However, histology study is recommended in order to rule-out other processes; the findings are usually a nonspecific inflammatory reaction characterized by massive neutrophil infiltration without microbiological infection (1,3,5-7,12).
Due to the lack of definitive laboratory and histological data, the diagnosis is based on the clinical criteria mentioned above (2,5); it should be suspected immediately once a peristomal ulcer is seen (1). In addition, every diagnostic test should be done to confirm or rule-out any underlying systemic disease eventually associated with it.
There is no definitive treatment for PPG that categorically offers satisfactory results. McGarity (4), in the original description, states: "Optimal treatment has not been established and needs to be adapted to each patient". This assertion remains valid thirty years later.
Therefore, treatment has to be compulsory established individually, among a multidisciplinary team concerning surgeons, gastroenterologists, dermatologists and stoma therapists.
There is, however, unanimity on starting treatment as soon as possible (5,9) and with a double target: Local and systemic. Various options are sometimes required and, given the intense pain especially at the onset of the lesions, as intense analgesia as required will be administered in each case.
Local treatment is based on debridement and cleaning of the ulcers under local anesthesia in order to eliminate detritus and necrotic areas, reducing exudation, pain and promoting healing. In addition, proper fitting ostomy devices that cause the least amount of trauma and permit secretions absorption should be applied in combination with the most appropriate local treatment.
The most used local treatment, with highly variable results, is topic corticosteroids, both occlusive dressings application or intradermal injection (1,3,5,7,9).
More recently, and especially in refractory cases, tacrolimus 0.3 % has been used with topical benzocaine (Orabase) (3,5,6,11,13). Lyon (13) performed a comparative study with corticosteroids; the study found a much better response with local application of tacrolimus 0.3 % in sodium carmelose, especially in ulcers larger than 2 cm so, together with systemic treatment, is considered the treatment of choice in these cases.
For this reason, given the characteristics of our patient's lesion, with one large extremely painful ulcer and significant impact on quality of life, we decided to apply it from the beginning together with systemic treatment. Side effects of its use have not been described in the literature.
Stomal relocation is not recommended except in exceptional cases given the high rate of recurrence PPG (2,3,6-8).
Whenever feasible, closure of the stoma may lead to healing (8). In the same manner, eradication of the underlying disease may be effective and lead to a definitive cure (2).
Regarding systemic treatment, the inability to carry out a prospective study due to the low prevalence of this kind of lesion has led to a wide variety of regimens based on the physicians judgment and experience that are obviously adapted to new options and possibilities (1,2,5,7,8).
Treatment is based on three pillars: antibacterial, anti-inflammatory and immunosuppressant drugs. The most widely antibiotics used are ciprofloxacin and metronidazole with various duration and dosage regimens adapted to each patient.
When talking about anti-inflammatories, most authors recommend starting with corticosteroids such as prednisone at a dosage of 0.6 to 1 mg per kilogram per day, with dose reduction every two weeks based on the patient's progress.
Finally, immunosuppressants have been incorporated, either alone or combined with corticosteroids. These include: azathioprine, mycophenolate mofetil, dapsone, 6-mercaptopurine, cyclosporine, minocycline, thalidomide and methotrexate, as well as biological treatments including anti-TNF agents such as infliximab, adalimumab, certolizumab and etanercept (14), with variable outcomes (1).
Very recently, for refractory cases, other monoclonal antibodies such as ustekinumab (15) have been used with good results.
The time to start systemic treatment is not well defined: It can be at the moment of diagnosis, in combination with local treatment, or once the local treatment has failed. In our patient, given the significant local involvement and overall impact, we decided to combine both treatments from the onset, with satisfactory response.
PPG appears to be an exceptional entity, but it is probably underdiagnosed. It should be suspected when any ulcerous lesion around a stoma is presented in order to start the appropriate treatment as soon as possible.
Besides local dressing changes and proper care by the Stoma Therapy Unit with application of corticosteroids or tacrolimus, there is no well defined patterns in relation to the onset, way or kind of medication to use. Treatment should be based on corticosteroids, immunosuppressive and biological therapy according to the experience of the multidisciplinary team and the patient's characteristics.
References
1. Wu X, Mukewar S, Kiran RP, Remzi FH, Hammel J, Shen B. Risk factors for peristomal pyoderma gangrenosum complicating inflammatory bowel disease. J Crohn's Colitis 2013;7:e171-7. [ Links ]
2. Sheldon D, Thirlby RC, Kozarek R. Peristomal pyoderma gangrenosum. Arch Surg 2000;135:564-9. [ Links ]
3. Hughes AP, Jackson JM, Callen JP. Clinical features and treatment of peristomal pyoderma gangrenosum. JAMA 2000;284:1546-8. [ Links ]
4. Mc Garity WC, Robertson DB y McKeown PP. Pyoderma gangrenosum at the parastomal site in patients with Crohn's disease. Arch Surg 1984;119:1186-8. [ Links ]
5. Uchino M, Ikeuchi H, Matsuoka H, Bando T, Takahashi Y, Takesue Y, et al. Clinical features and management of parastomal pyoderma gangrenosum in inflammatory bowel disease. Digestion 2012;85:295-301. [ Links ]
6. Lyon CC, Smith AJ, Beck MH, Wong GA, Griffiths CE. Parastomal pyoderma gangrenosum: Clinical features and management. J Am Acad Dermatol 2000;42:992-1002. [ Links ]
7. Kiran RP, O'Brien-Ermlich B, Achkar JP, Fazio VW, Delaney CP. Management of peristomal pyoderma gangrenosum. Dis Colon Rectum 2005;48:1397-403. [ Links ]
8. Poritz LS, Lebo MA, Bobb AD, Ardell CM, Koltun WA. Management of peristomal pyoderma gangrenosum. J Am Coll Surg 2008;206:311-5. [ Links ]
9. Funayama Y, Kumagai E, Takahashi K, Fukushima K, Sasaki I. Early diagnosis and early corticosteroid administration improves healing of peristomal pyoderma gangrenosum in inflammatory bowel disease. Dis Colon Rectum 2009;52:311-4. [ Links ]
10. Cerdán J, Cantero R, Martínez S, García C, Torres-Melero J, Balibrea JL. Pyoderma gangrenosum at the colostomy site in a patient with Crohn's disease. Coloproctology 1994;16:407-10. [ Links ]
11. Khurrum Baig M, Marquez H, Nogueras JJ, Weiss EG, Wexner SD. Topical tacrolimus (FK506) in the treatment of recalcitrant parastomal pyoderma gangrenosum associated with Crohn's disease: Report of two cases. Colorectal Disease 2004;6:250-3. [ Links ]
12. Bafford AC, Irani JL . Management and complications of stomas. Surg Clin N Am 2013;93:145-66. [ Links ]
13. Lyon CC, Stapleton M, Smith AJ, Mendelsohn S, Beck MH, Grif CEM. Topical tacrolimus in the management of peristomal pyoderma gangrenosum. J Dermatol Treat 2001;12:13-17. [ Links ]
14. Kim FS, Pandya AG. The use of etanercept in the treatment of peristomal pyoderma gangrenosum. Clin Experimental Dermatology 2012;37:442-3. [ Links ]
15. Fahmy M, Ramamoorthy S, Hata T, Sandborn WJ. Ustekinumab for peristomal pyoderma gangrenosum. Am J Gastroenterol 2012;107:794-5. [ Links ]
![]() Correspondence:
Correspondence:
Carlos Cerdán Santacruz
Colorectal Surgery
General Surgery Department
Clínica Santa Elena
C/ De la Granja, 8
28003 Madrid, Spain
e-mail: carloscerdansantacruz@hotmail.com
Received 10-01-2013
Accepted 15-01-2014











 texto en
texto en