Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.5 Madrid may. 2014
LETTERS TO THE EDITOR
Intraductal papillary neoplasm of the bile duct
Neoplasia intraductal papilar de la vía biliar: a propósito de un caso
Key words: Cystic lesions of the liver. Cystoadenocarcinoma. Intraductal papillary lesions of the bile duct. Communication with the bile duct. Caroli's disease.
Palabras clave: Lesiones quísticas hepáticas. Cistoadenocarcinoma. Lesiones papilares intraductales de la vía biliar. Comunicación con la vía biliar. Enfermedad de Caroli.
Dear Editor,
Cystadenocarcinoma of the liver is an exceptional tumor that, along with cystadenoma, represents less than 5% of cystic tumors of the liver (1).
Case report
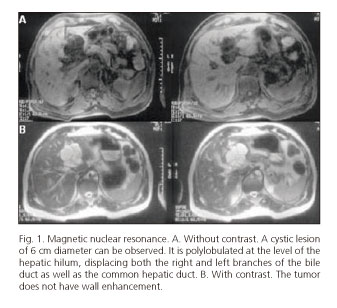
A 67 year-old-men, with personal history of left hemifacial spasm, suffered from abdominal pain in the epigastric and right upper quadrant as well as fever and coluria over the last four years. The physical examination revealed upper quadrant pain with a negative Murphy, and a slight increase in transaminase in the blood test. In the ultrasound, a 4 cm cyst at the hepatic hilum was observed. A CT scan of the abdomen revealed a dilation of the bile duct with a hypodense lesion in the hepatic hilum. The MRI showed a polylobulated cyst of 6 cm of diameter compressing the intrahepatic bile duct (Fig. 1A), without wall enhancement after intravenous contrast (Fig. 1B).
Due to episodes of cholangitis, the patient was diagnosed with Caroli's disease. Exploratory laparotomy was performed, revealing an intrahepatic cystic tumor in segments IV-III, which after intraoperative choliangiography showed communication with the main bile duct. A regulated left hepatectomy and cholecystectomy was performed with a favorable postoperative evolution.
The histology showed a lesion consisting of multiple fibrous-wall cysts, lined with mucosecretor epithelium with flat areas, papillary projections, cytologic atypia, and a solid nodule with focal infiltration of the cyst wall, reaching neither the liver parenchyma nor the surgical margins (Fig. 2). There was no evidence of ovarian stroma. All of this was compatible with a diagnosis of biliary cystadenocarcinoma.
Five years later, the patient was asymptomatic with no radiological signs of recurrence.
Discussion
Cystadenocarcinoma is a biliary cystic neoplasm with an incidence of 0.4 % (2,3), formed by biliary epithelia with cellular atypia, papillary projections and, in some cases, invasive growth (1,4). Its etiology is unknown, but it could derive from ectopic embryonic remains of the bile ducts, a cystadenoma, ectopic ovarian tissue or intrahepatic congenital malformations (5). On the other hand, Caroli's disease consists of cystic dilations of the intrahepatic biliary ducts (6).
They are classically divided into two subgroups based on whether or not ovarian stroma is present. The first are more frequent, common in women and with a better prognosis. The second appear in both sexes, are more aggressive, and have a poorer prognosis.
Cases with communication with the bile duct are exceptional. It is not clear if tumors with or without communication with the bile ducts could be indicative of two different tumors or two clinical manifestations of the same tumor. In the pancreas, they are considered as two types of tumors: Mucinous cystic tumors, which occur in females, do not have communication with the pancreatic duct, and present with ovarian-like stroma, and intraductal papillary mucinous neoplasms (IPMN), which occur in both sexes and communicate with the pancreatic duct (7). Zen et al. concluded that the term cystadenoma/cystadenocarcinoma should be restricted to true cystic tumors of the liver with ovarian-like stroma (8). Currently, cases of ovarian stroma without communication with the bile ducts are called mucinous cystic neoplasms (MCN), classified by their degree of atypia as low, moderate or high in non-invasive cases, and in MCN cases with associated invasive carcinoma when there is an invasive component (9). The presence of ovarian stroma is characteristic of MCN. However, cases such as ours are considered as intraductal papillary neoplasms of the bile duct (IPN-B) because there is communication with the bile duct and there is no ovarian-like stroma (8-10).
Radical resection offers the best results in terms of rate of recurrence and survival (1,4). Lauffer recommends hepatic resection for any multilocular cystic lesion (5). Our patient benefited from radical surgery. Neither chemotherapy nor radiotherapy are effective adjuvant therapies (4).
Differential diagnosis among the rest of the cystic lesions is complex, requiring a high degree of suspicion, and confirmation after histological study. We consider this case relevant because of its described peculiarities that highlight the new classification and the importance of radical surgery for the patient's prognosis.
Yurena Caballero1, Javier Larrea1, Rocío Romero1, Mercedes Cabrera1,
Gabriel Plaza1, Juan Luis Afonso2 and Juan Ramón Hernández1
Departments of 1General Surgery and Digestive Diseases, and 2Pathology.
Hospital Universitario Insular de Gran Canaria. Las Palmas de Gran Canaria, Las Palmas. Spain
References
1. Ramia JM, de La Plaza R, Figueras J, García-Parreño J. Benign non-parasitic hepatic cystic tumours. Cir Esp 2011;89:565-73. [ Links ]
2. Bernardos-García C, Alarcón Del Agua I, Casado-Maestre MD, Serrano-Borrero I, Alamo-Martínez JM. Hepatic cystoadenocarcinoma. Differential diagnosis of hepatic cystic tumors. Rev Esp Enferm Dig 2009;101:369-71. [ Links ]
3. Zhang M, Yu J, Yan S, Zheng SS. Cystoadenocarcinoma of the liver: A case report. Hepatobiliary Pancreat Dis Int 2005;4;464-7. [ Links ]
4. Yu Q, Chen T, Wan YL, Min J, Cheng Y, Guo H. Intrahepatic biliary cystadenocarcinoma: Clinical analysis of 4 cases. Hepatobiliary Pancreat Dis Int 2009;8:71-4. [ Links ]
5. Läuffer JM, Baer HU, Maurer CA, Stoupis C, Zimmerman A, Büchler MW. Biliary cystadenocarcinoma of the liver: The need for complete resection. Eur J Cancer 1998;34:1845-51. [ Links ]
6. Söreide K, Körner H, Havnen J, Söreide JA. Bile duct cysts in adults. Br J Surg 2004;91:1538-48. [ Links ]
7. Goh BK, Tan Ym, Chung Yf, Chow PK, Cheow PC, Wong WK, et al. A review of mucinous cystic neoplasm of the pancreas defined by ovarian-type stroma: Clinicopathological features of 334 patients. World J Surg 2006;30:2236-45. [ Links ]
8. Zen Y, Fujii T, Itatsu K, Nakamura K, Konishi F, Masuda S, et al. Biliary cystic tumors with bile duct communication: a cystic variant of intraductal papillary neoplasm of the bile duct. Mod Pathol 2006;19:1243-54. [ Links ]
9. Tsui WMS, Adsay NV, Crawford JM, Hruban R, Kloppel G, Wee A. En: Bosman FT, Mucinous cystic neoplasms of the liver. Carneiro F, Hruban RH, Theise ND, editores. WHO Classification of the tumours of the digestive system. International Agency for research on cancer; Lyon 2010. p. 236-8. [ Links ]
10. Makino I, Yoshimitsu Y, Sakuma H, Nakai M, Ueda H. A large cystic tumor with bile duct communication originating around the hepatic hilum. J Gastrointestin Liver Dis 2010;19:77-80. [ Links ]











 texto en
texto en