My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.6 Madrid Jun. 2014
CLINICAL NOTE
Endoscopic management of common patologies with a new suturing system
Tratamiento endoscópico de enfermedades comunes con un nuevo sistema de sutura
Fernando González-Panizo-Tamargo1, Álvaro Rojas-Sánchez1, Pablo Miranda-García1, Diego Juzgado-Lucas1 and Enrique Vázquez-Sequeiros1,2
1Endoscopy Unit. Digestive Diseases Department. University Hospital Quirón. Madrid, Spain.
2Endoscopy Unit. Gastroenterology Department. University Hospital Ramón y Cajal. Madrid, Spain
ABSTRACT
Background: Overstitch endoscopic suturing system (Apollo Endosurgery. Austin, Texas) was created for NOTES procedures. As it demonstrated to be feasible, secure and effective in this field, further studies have evaluated its use in common gastrointestinal disorders in which current therapeutic tools, endoscopic or not, are not efficient or safe enough. Published results are promising. We present our initial experience with this system in the management of pathologies we usually face in our clinical practice.
Method: Suturing system was evaluated for: 1. Endoscopic fixation of metallic stent to prevent migration in patients with gastrointestinal non-neoformative pathology. 2. Outlet reduction in patients with weight regain following Roux-en-Y gastric bypass.
Results: During a period of 6 months Overstitch endoscopic suturing system was used in 5 patients: For stent fixation in 3 and for outlet reduction in 2. Technical success: Suture was performed in all the patients. Only 1 stitch was lost. Effectiveness: Stent fixation and outlet reduction were achieved in all the patients. However, in 1 patient the final anastomotic size was not close enough. Clinical success: Clinical recovery was achieved in all the patients in whom endoscopic stent fixation was performed. The patient which appropriated outlet closure developed a significant weight loss. The patient in which final size was not close enough did not lose weight.
Conclusions: We found Overstitch endoscopic suturing system feasible, safe and effective, as it has been previously described. We encourage the publication of further studies evaluating the real utility of this tool, mostly taking into account that it allows a successful management of usual disorders for which there are not current effective therapies.
Key words: Endoscopic suturing system. Stent. Weight.
Background
Overstitch endoscopic suturing system (Apollo Endosurgery. Austin, Texas) was initially designed for the closure of gastrointestinal wall lacks performed during NOTES procedures (1). Approved by FDA in 2008, in the last years few studies have evaluated it in humans in form of isolated cases or, at most, small series. All these studies have described this system as feasible, effective and safe (2-5). The spread of this new technique and these results encouraged other endoscopists to evaluate it in problems usually founded in the clinical practice, such as anastomotic dehiscence, fistula or stent migration, for which endoscopic or surgical therapies are not effective enough or too risky (6-11). Results published in these studies demonstrated safe and feasibleness of Apollo Overstitcht system, and a high effective suture. In Europe this system is available since 2013 and the few data published are comparable (12). The knowledge of this system and the theoretical benefits it can provide in the clinical practice have motivated us to try it in our patients. We present the results obtained applying this suturing system for the resolution of common pathologies for which current endoscopic therapies are not efficient enough while surgical options involve an elevated morbidity.
Methods
Initial experience with Apollo Overstitch Endoscopic Suturing System carried out in Quirón Madrid Universitary Hospital. Indications were: a) Metallic autoexpandible stent fixation in non-neoplastic pathology; and b) gastric outlet reduction in patients with weight regain following Roux-en-Y gastric bypass. Data collected to evaluate the utility of this system were: Basal features of the patients and data related to the proceeding: Duration, number of stitches, technical success (fulfillment of the suture), efficacy (achievement of the aim of the suture: fixation of the stent and gastric outlet reduction), clinical success (achievement of the therapeutic aim: Resolution of the symptoms and weight loss).
- Endoscopic suturing procedure: All the explorations were performed under general anesthesia, with antibiotic prophylaxis (Amoxiciline-Clavulanic Acid 1 g/8 h e.v.) and with the help of an overtube to avoid mucosal lacerations due to the suturing system.
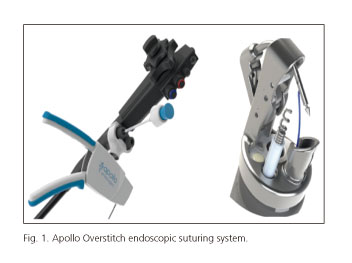
Overstitch suturing system was put in a double-channel therapeutic endoscope (Olympus, GIF-2TH180). Figure 1 shows the assembly of the suturing system: The metallic cap placed in the tip of the endoscope presents a mobile curved arm that will hold the needle that can perform a continue suture or isolated stitch. A plastic piece with the control of the suturing system is fixed close to the proximal access of the working channel, through which the thread and needle will be passed (in our cases, 2-0 non-reabsorbable polipropylen thread) to reach the curved arm at the tip. Through the other working channel a secondary tool called helix will be passed to be anchored in the gastrointestinal wall, spinning clockwise 4 times, that will allow strength traction of this towards the needle to facilitate the full-thickness suture and avoid accidental blind puncture of structures around the digestive tube. Once the last stitch has been placed, the proximal and distal blocks of the suture are released: a plastic piece and the suturing needle respectively (Fig. 1).
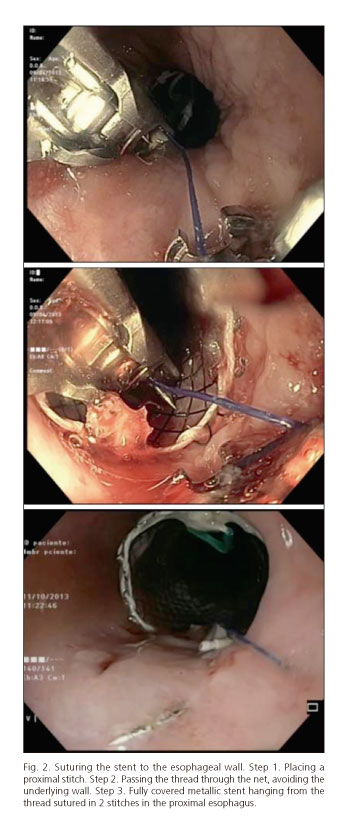
- Stent fixation procedure: Metallic stent was placed as usual, assisted by a guidewire an under endoscopic and radiologic control. Once it was correctly released, the proximal end was sutured to the wall hanging it to 2 stitches in the proximal mucosa, 2-3 cm above the stent. An intermediate thread between the stitches was passed through the stent net, avoiding the underlying mucosa (Fig. 2).
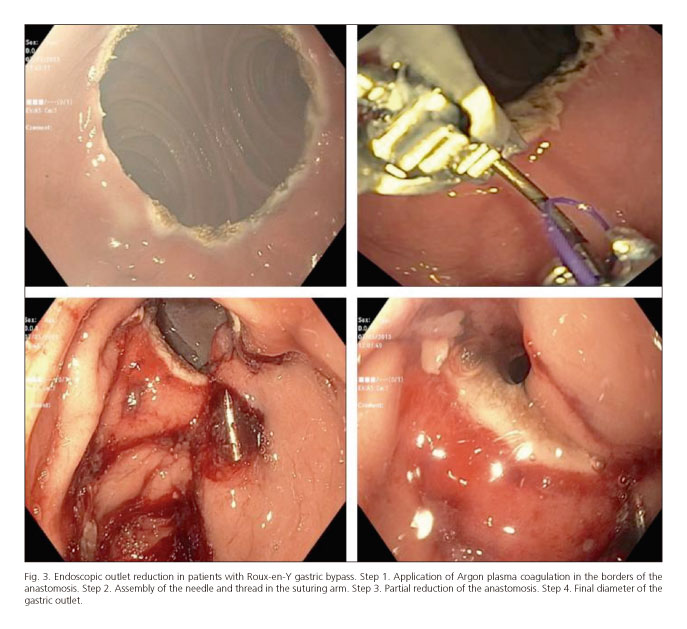
- Gastric outlet reduction proceeding: First step was the fulguration of the anastomotic borders with APC to estimulate the subsequent cicatrization. Afterwards, depending of the anastomosis diameter, 2-3 stitches were put in opposite borders to try to achieve a final caliber < 10 mm (Fig. 3).
- Discharge: After the suturing procedure, patients with bariatric disorder were discharged later that day, with liquid diet until they were controlled at 15 days. Then normal diet was progressively introduced and patient was revised at 1 month. In those patients which stent fixation, after 24 hours of fasting, oral intake was introduced and, if it was appropriate and no complications were identified, patients were discharged unless their basal pathology did not permitted it. All the patients received a discharging report including 5-day antibiotic treatment.
Results
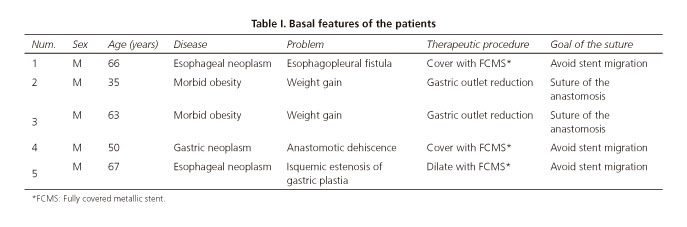
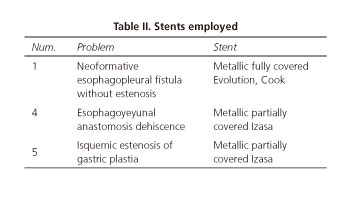
During a period of 6 months suture was performed in 5 patients: stent fixation in 3 cases and gastric outlet reduction in 2 cases (Table I). Table II shows the type of stent used according to the main aim. Suturing procedure time was 44 and 34 minutes in gastric outlet reduction (case 2 and 3 respectively) and 27, 20 and 19 minutes in stent fixation cases (1, 4 and 5 respectively). 3 and 2 stitches were used in both indications respectively. Anastomotic diameters were initially 5 and 3 cm (patients 2 and 3 respectively). Technical success: All the stitches were succesfully put excepting 1 of them in which the thread broke (patient 2). Effectiveness: Stent was adequately anchored in the 3 cases. Significant gastric outlet reduction was achieved in both cases. In patient number 2 final diameter of the anastomosis was almost 10 mm. Clinical success: In patient n.o 1, bronchial symptoms resolved and the pleural drainage could be removed since the stent was fixed until the patient dead 3 months later due to complications related to his basal disease. In patient n.o 2 significant weight reduction was not achieved. At this moment he is waiting for a new suturing procedure. Patient n.o 3 lost 12 kg the first month after the suture. At this moment he is waiting for a new check-up. Patients n.o 4 and 5 could normalize oral intake after stent fixation. No dysphagia symptoms have been related during the follow-up (1 and 2 months respectively). Clinical monitoring was performed in all cases, and also radiologic in those patients with stent. If there were no clinical complications, it was assumed that the suture was doing her job, so endoscopic exam was not performed. In patient n.o 2, as weight loss was not achieved, endoscopic evaluation was performed 1 month after the procedure, noting that anastomotic diameter was not close enough. Complications: During the procedure all the patients presented minor bleeding comparable to other endoscopic non-complicated procedures. Both patients with bariatric pathology presented controlled vomits the first 24 h, as it is common after bariatric procedures. Patients with stent fixation felt the typical stent-related discomfort the first hours. During the follow-up no other complications were related.
Discussion
Fully or partially covered metallic stents are easy to put and remove, safe and leacktightness. For these reasons they are considered the main tool not only for the management of benign obstructions, but also in the sealing of digestive wall lacks (anastomotic dehiscence, fistula...). The major disadvantage of this kind of stent is an elevated migration rate (up to 40 %) (13,14). Several sorts of endoscopic sutures to fix the stent have been previously tested with unfortunate results (15-19). Few studies evaluating Overstitch suturing system for this aim have described a success stent fixation, with a significant reduction in the migration rate, in an easy and safe way (7-9). However, stent migration still happens (up to 21 % with Overstitch), and this despite Apollo Overstitch allows a non-reabsorbable full-thickness suture. Investigators argue that, in many of this cases, the sutures are not well performed, not as deep as this system allows, increasing the risk of loss. We suggest that this problem is related to the fact that all the studies suture directly the stent to the wall, where the stent net interfere in the movement of the curved arm and the helix, making it more difficult to make a full-thickness suture. Instead of this hard technique, we have placed 2 stitches in the proximal mucosa, where they can be easily placed appropriately, and we have anchored the stent to them. The thread that join both stitches passes only through the net of the stent avoiding the underlying wall (Fig. 2). No migration was described with our system, so we suggest this easier proceeding can simplify the suture and avoid or reduce previously described problems.
The weight regain following Roux-en-Y gastric bypass has been related with the dilation of the pouch and anastomosis. Though several studies have evidenced that the reduction of the anastomosis again < 10 mm is directly related with new weight loss, surgical reintervention presents high morbidity (12). Overstitch suturing system has been previously used for the creation of endoscopic gastric tubulization. This motivated investigators to evaluate its use for the closure of those dilated anastomoses. In a study with 25 patients followed over 1 year, authors described 100 % technical success without significant complications. Overstitch demonstrated to be effective to reduce the anastomosis diameter below 10 mm (average = 6 mm), what clinically meant a significant weight loss, maintained over the following period. In the 2 patients in which we have carried out this proceeding, significant diameter reduction was achieved, and when it was less than 10 mm (6 mm in our case), it was related with a significant weight loss. The only failure we have had placing the stitches happened with the first bariatric patient (patient n.o 2) when the thread broke due to an excessive traction. Afterwards 2 more stitches were placed successfully in that patient and anastomosis diameter could be reduced to nearly 1 cm. That measure was then considered close enough to be effective, and no additional stitches were used. Unfortunately this closure was not clinically significant. This suturing system is very intuitive and the learning curve is fast, but we think those mistakes were related with our inexperience: an excessive traction and the decision of not narrowing that anastomosis. In the second patient (patient n.o 3) stitches were correctly placed and the final diameter of the anastomosis was far below of 10 mm (6 mm). This patient presented a weight lost > 10 kg during the first month.
In this initial experience we founded Overstitch endoscopic suturing system easy to manipulate and, with the addition of the helix, safe and effective. This tool allows a significant traction of the gastrointestinal wall close to the needle minimizing the risk of accidental blind puncture of adjacent structures. It also allows a deep suture what is one of the most important advantages of this system as we think. Taking into account the published experience, we agree with previous authors that Overstitch is a promising endoscopic suturing system that needs new evidence with large and well-designed studies to confirm the promising results obtained. We also think that the absence of therapeutic alternatives at this moment to treat these problems, so common in the daily clinical practice, should increase the interest of endoscopists in the evaluation of this tool.
References
1. Banerjee S, Barth BA, Bhat YM, Desilets DJ, Gottlieb KT, Maple JT, et al. ASGE Technology Committee Endoscopic closure devices. Gastrointest Endosc 2012;76 (2): 244-51. [ Links ]
2. Rajan E, Gostout CJ, Aimore Bonin E, Moran EA, Locke RG, Szarka LA, et al. Endoscopic full-thickness biopsy of the gastric wall with defect closure by using an endoscopic suturing device: survival porcine study. Gastrointest Endosc 2012; 76(5):1014-9. [ Links ]
3. Armengol JR, Abu-Suboh M, Dot-Bach J, Masachs M, Armengol J, Benages, ET AL. Comparison of endoscopic suturing techniques for closure of the transgastric entrance site for NOTES procedure. Endoscopy 2012;44-A02. [ Links ]
4. Armengol JR, Dot-Bach J, Abu-Suboh M, Armengol J, Masachs M, Benages A, et al. Endoscopic closure of iatrogenic colonic perforations: randomized controlled trial on animal model and initial clinical experience. Gastrointest Endosc 2013;77 (5S):AB461. [ Links ]
5. Armengol JR, Abu-Suboh M, Dot-Bach J, Armengol J, Masachs M, Benages A, et al. Full-thickness endoscopic resection of gastrointestinal cancer: from animal experiments to humans. Abstract Mo1650. Gastrointest Endosc 2013;77(5S): AB458. [ Links ]
6. Abu Dayyeh BK, Rajan E, Gostout CJ Endoscopic sleeve gastroplasty: A potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity.Gastrointest Endosc 2013;78(3):530-5. [ Links ]
7. Fujii LL, Bonin EA, Baron TH, Gostout CJ, Wong Kee Song LM. Utility of an endoscopic suturing system for prevention of covered luminal stent migration in the upper GI tract. Gastrointest Endosc 2013;78(5):787-93. [ Links ]
8. Sharaiha RZ, Kumta NA, Doukides TP, Equia V, Gonda TA, Widmer JL, et al. Esophageal Stenting With Sutures: Time to Redefine Our Standards? J Clin Gastroenterol. 2014 Aug 8 (Epub ahead of print). [ Links ]
9. Kantsevoy SV, Bitner M. Esophageal stent fixation with endoscopic suturing device. Gastrointest Endosc 2012;76(6):1251-5. [ Links ]
10. Kantsevoy SV, Thuluvath PJ. Successful closure of a chronic refractory gastrocutaneous fistula with a new endoscopic suturing device. Gastrointest Endosc 2012;75(3):688-90. [ Links ]
11. Fogel R. Endoscopic vertical gastroplasty using an endoscopic suturing technique for the treatment of obesity. Gastrointest Endosc 2013;77(5S):AB460. [ Links ]
12. Jirapinyo P, Slattery J, Ryan MB, Abu Dayyeh BK, Lautz DB, Thompson CC. Evaluation of an endoscopic suturing device for transoral outlet reduction in patients with weight regain following Roux-en-Y gastric bypass. Endoscopy 2013;45(7):532-6. [ Links ]
13. Langer FB, Schoppmann SF, Prager G et al. Temporary placement of self expanding oesophageal stents as bridging for neo-adjuvant therapy. Ann Surg Oncol 2010;17:470-5. [ Links ]
14. Bakken JC, Wong Kee Song LM, de Groen PC, et al. Use of a fully covered self-expandable metal stent for the treatment of benign esophageal diseases. Gastrointest Endosc 2010;72:712-20. [ Links ]
15. Bonavina L, Bona D, et al. Endoscopic clipping: a helpful tool for positioning self-expanding esophageal stents. Endoscopy 1995;27:348. [ Links ]
16. Sriram PV, Das G, Rao GV, et al. Another novel use of endoscopic clipping: to anchor an esophageal endoprosthesis. Endoscopy 2001;33:724-6. [ Links ]
17. Babor R, Talbot M, Tyndal A. Treatment of upper gastrointestinal leaks with a removable, covered, self-expanding metallic stent. Surg Laparosc Endosc Percutan Tech 2009;19:e1-4. [ Links ]
18. Blackmon SH, Santora R, Schwarz P et al. Utility of removable esophageal covered self-expanding metal stents for leak and fistula management. Ann Thorac Surg 2010;89:931-6. [ Links ]
19. Vanbiervliet G, Filippi J, Karimdjee BS, et al. The role of clips in preventing migration of fully covered metallic esophageal stents: a pilot comparative study. Surg Endosc 2012;26:53-9. [ Links ]
![]() Correspondence:
Correspondence:
Fernando González-Panizo-Tamargo.
Endoscopy Unit.
Digestive Diseases Department.
University Hospital Quirón.
c/ Diego de Velázquez, 1. 28223
Pozuelo de Alarcón, Madrid. Spain
e-mail: fernandogpanizo@gmail.com
Received: 03-12-2013
Accepted: 18-02-2014