Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 no.8 Madrid dic. 2014
LETTERS TO THE EDITOR
Ectopic pancreas as a rare cause of obstructive jaundice
Páncreas ectópico como causa rara de ictericia obstructiva
Key words: Jaundice. Obstructive. Heterotopic tissue.
Dear Editor,
The authors describe a case of a 68-year-old man presenting in the emergency room with a one-week history of jaundice, pruritus and weight loss. Patient had history of hypertension (on therapy with telmisartan), alcohol (75 g/day), and tobacco consumption.
On physical examination only jaundice was noticed. Blood tests showed elevation of total and conjugated bilirubin (21.1 and 13.3 mg/dL), ALT (493 IU/L), AST (522 IU/L), alkaline phosphatase (542 IU/L), gamma-glutamyl transpeptidase (2102 IU/L) and carbohydrate antigen 19-9 (229 IU/mL). Contrast-enhanced helicoidal computed tomography and magnetic resonance cholangiography demonstrated dilation of intrahepatic ducts and distal common bile duct (CBD) (16 mm) ending in an abrupt stenosis, without an apparent cause. Liver, pancreas and Wirsung were normal.
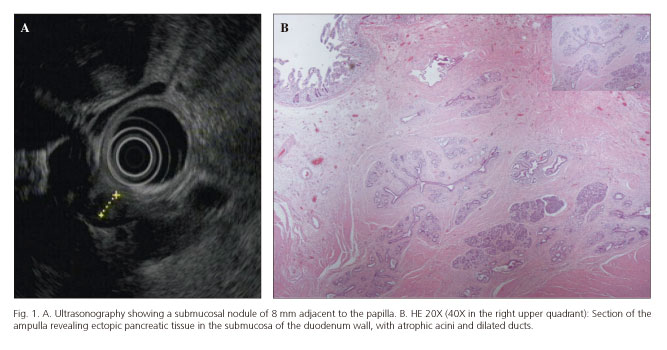
Endoscopic retrograde cholangiopancreatography revealed a slightly enlarged papilla and a stenosis in the CBP, where a 10 Fr plastic stent was placed; brush cytology of the CBD and biopsies of the ampulla were normal. In endoscopic ultrasonography (EUS), a hypoechoic submucosal nodule of 8 mm was seen in the area of the ampulla (Fig. 1A).
There was clinical and laboratory improvement and patient was discharged. He returned one month after with an episode of cholangitis.
The case was then discussed with surgeons and as a neoplastic cause could not be ruled out based on the imagiologic and endoscopic findings (repeated twice), the decision was to perform a pancreaticoduodenectomy.
Macroscopic examination revealed dilated bile ducts and normal pancreas. In section of the ampulla, there was an expansion of the submucosa composed of ectopic pancreatic tissue with features of chronic pancreatitis (Fig. 1B).
The patient remains asymptomatic after a year of follow-up.
Discussion
Ectopic pancreas is a rare condition defined as pancreatic tissue abnormally situated, without contact with normal pancreas and with its own ductal system and blood supply (1). The most common locations are duodenum, stomach and jejunum (2). Periampullary location has been described in less than 25 reports (3). Clinical presentation is usually asymptomatic or, in case of inflammation, obstructive jaundice can occur.
Accurate preoperative diagnosis using endoscopic or radiologic imaging is difficult because the findings are not pathognomonic. The presence of a central umbilication of the ampulla in endoscopy, although characteristic, is infrequent (4). EUS may be important at the diagnosis showing a hypoechoic and heterogeneous nodule with indistinct margins, generally in the submucosa (4,5).
Local excision may be the treatment of choice. However, as the correct diagnosis is sometimes difficult and this situation can mimic a neoplasia, pancreaticoduodenectomy is performed in the majority of cases (3,5,6).
We describe this case of periampullary ectopic pancreas, where the clinical doubt about etiology (malignant or not) ended in a radical surgery. Although the findings in EUS can be recognized as a feature of this disease, a fine needle aspiration or a biopsy of the nodule would not be conclusive because, in the presence of pancreatic tissue in this location, we would probably interpret it as an error sample.
We admit that the possibility of ectopic pancreas, although rare, should be included in the differential diagnosis of obstructive jaundice and that EUS can show a typical image and help in the diagnosis.
Rita Carvalho1, Paulo Freire1, Francisco Portela1, Dário Gomes1, Paulo Andrade1,
Ana Bento2, Hamilton Batista2, M. Augusta Cipriano3 and Carlos Sofia1
1Gastroenterology Department,
2General Surgery Department and
3Pathology Department.
Coimbra University Hospital. Portugal
References
1. Hsu SD, Chan DC, Hsieh HF, Chen TW, Yu JC, Chou SJ. Ectopic pancreas presenting as ampulla of Vater tumor. American Journal of Surgery 2008;195:498-500. [ Links ]
2. Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue. A study of 212 cases. Archives of Surgery 1974;109:762-5. [ Links ]
3. Biswas A, Husain EA, Feakins RM, Abraham AT. Heterotopic pancreas mimicking cholangiocarcinoma. Case report and literature review. Journal of the Pancreas 2007;8:28-34. [ Links ]
4. Chen CH, Yang CC, Yeh YH, Chou DA, Kuo CL. Ectopic pancreas located in the major duodenal papilla: Case report and review. Gastrointestinal Endoscopy 2001;53:121-3. [ Links ]
5. Rao RN, Kamlesh Y, Pallav G, Singla N. Ectopic pancreas presenting as periampullary tumor with obstructive jaundice and pruritus is a rare diagnostic and therapeutic dilemma. A case report. Journal of the Pancreas 2011;12:607-9. [ Links ]
6. Molinari M, Ong A, Farolan MJ, Helton WS, Espat NJ. Pancreatic heterotopia and other uncommon causes of non-malignant biliary obstruction. Surgical Oncology 2000;9:135-42. [ Links ]