My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.106 n.8 Madrid Dec. 2014
LETTERS TO THE EDITOR
Dermatitis herpetiformis in Brazilan male celiac disease patients: a case series
Dermatitis herpetiforme en hombres brasileños con enfermedad celiaca: una serie de casos
Key words: Dermatitis herpetiformis. Celiac disease. Dapsone. Autoimmune bullous disease. Gluten-free diet.
Dear Editor,
Celiac disease (CD) is a chronic autoimmune systemic disease triggered and maintained by gluten proteins. CD can begin at any age with a higher prevalence among the female gender (ratio 2:1/3:1) (1,2). Due to minor prevalence in male gender, CD has been less studied in this group (2).
Dermatitis herpetiformis (DH) is an autoimmune blistering cutaneous disease considered as the specific phenotypic expression of a gluten-sensitive enteropathy on the skin, immunohistochemicaly indistinguishable from CD (3,4). DH is considered rare, (3) except in celiac patients, among whom it is present in 15 to 25 % (5). Gender can influence the onset, clinical presentation, progression, and outcome of some autoimmune diseases (6). Although controversial, clinical presentation of several autoimmune diseases in males can be more severe (7).
The present study aims to report the clinical aspects of male Brazilian patients with both CD and DH, also showing their laboratory and histological findings, treatment and follow-up information.
Patients and methods
This study with an observational, descriptive and retrospective design analyzed a series of consecutively diagnosed celiac patients; it was approved by the Institutional Ethic Committee.
Of a total of eighty-seven men, all with European ascendancy, diagnosed with CD and attended by a single physician in a private office between 1992 and 2012, fourteen (16.1 %) had a diagnosis of DH. All data were collected from patients' charts. CD was diagnosed based on clinical, serological, and histological findings (Marsh's classification) (1). Diagnoses of DH was based on clinical and histological findings in skin biopsies. The follow-up of the patients consisted in interviews, clinical examination and serological tests. All the evaluations were conducted by the same physician at the moment of diagnosis, once a month up to the 6th month after diagnosis, and then every six months.
Results
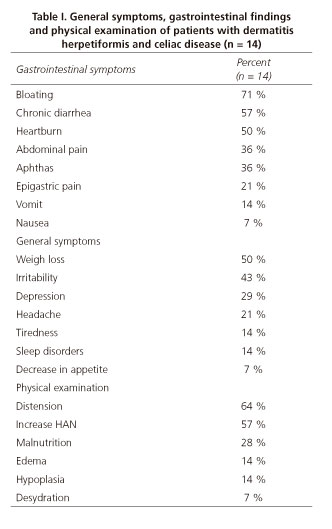
Fourteen male patients, with a median age of 34 (rank 17 to 55 years) were diagnosed with both CD and DH. Their general and gastrointestinal complaints are shown in table I. Demographical data of patients are shown in table II.
All patients were diagnosed as having DH due to a typical skin lesion presentation. Despite the presence of classical features of DH, a delay in the diagnosis, ranging from 0 to 240 months (median: 30 months) was documented. Immunoglobulin A antiendomisial antibodies (IgA-EmA) were investigated in 9 cases, being 5 (55.5 %) positive. Duodenal biopsies confirmed CD in all the patients, and the histological evaluation showed severe enteropathy in 11 cases (78.6 %), mild mucosal changes in 3 (21.4 %), who also exhibited normal intraepithelial lymphocytes counts (Table II).
Every patient was treated with a GFD; 7 (50 %) also received oral dapsone, and in one case, adding azathioprine was necessary. One patient presented jaundice after being treated with dapsone and this drug was discontinued.
Anemia was observed in 25 % (3/12) of patients. Nine patients were investigated for thyroid diseases, and 4 (44.4 %) presented hypothyroidism. One patient (7.1 %) presented lymphoma (54 years old) after 35 years of being diagnosed of CD.
Five patients had another first-degree relative with a gluten-related disorder: DH was reported in one father and in one sister, CD was reported in one sister and one daughter, and one patient had twin daughters with both CD and DH.
Discussion
Our study documented that DH is commonly associated to CD in Brazilian male patents in a similar way that reported from European and North American studies, suggesting that geographic differences are not influenced in these diseases (2,4). The same was observed regarding the mean age of occurrence (third or fourth decade), as well as with diagnostic delay (4,8) (Table II).
According to some authors, about 5 % of CD patients will present DH at any moment in their lives, before or after the diagnosis of CD (6) as observed in the present study (Table II). The mechanisms that trigger overt symptoms are not well understood. In Brazil, the only report on this subject is credited to Kotze, who referred DH in 11.5 % of the 157 studied CD patients of both genders (1).
Although all DH patients presented gluten sensitivity, the great majority were asymptomatic regarding the digestive point of view. Alonso-Llamazares et al. (8), described that 13 % of patients with DH reported digestive complaints. In our study, bloating, chronic diarrhea and abdominal pain were the main digestive symptoms referred. General symptoms of patients mainly included weight loss, malnutrition, and peripheral edema (Table I).
Physical examination by itself may provide a suspicion of DH; however, additional testing is usually required. Some authors related that small bowel biopsies are usually not necessary in a DH workup (3). Additionally, we recommend obtaining duodenal biopsies because this first evaluation of the intestinal mucosa is useful for the future, especially if a suspicion of malignancy (lymphoma) exists (1,3). Intestinal biopsies performed in patients with DH also reveal signs of gluten-related enteropathy in 60 % to 75 %, ranging from a normal-appearing epithelium to a flat mucosa (Marsh I to III) (8). Bolotin and Petronic (10) reported that about 20 % of DH patients had an apparently normal small-bowel mucosal architecture, but patients can show findings consistent with a latent CD, as demonstrated in our study (Table II).
Screening of patients' relatives must be recommended at the time of diagnosis, and, in the present study, the discovery of first-degree relatives having CD or DH in 5 patients reinforces our assertion, as the majority of them were asymptomatic or undiagnosed.
Hervonen et al. reported a 1.0 % prevalence of lymphoma in 1,104 CD cases from Finland (8). This malignancy can occur both in and outside the gastrointestinal tract as a nodal or extranodal disease. It is remarkable that among our 14 patients with DH, lymphoma was diagnosed in one patient with a long-life CD plus DH, on a GFD. Whether GFD protects against the development of lymphoma in CD is controversial. In DH patients, the adherence of a GFD could be lenient and could increase the risk of cancer. On the other hand, survival rates in patients with DH do not appear to differ from those of the general population.
Gastroenterologists treating patients with CD must be alert for skin manifestations of gluten sensitivity and other associated diseases. On the other hand, dermatologists may be aware of digestive implications of DH.
Lorete Maria da Silva Kotze1, Luiz Alexandre Dalla Vecchia2, Renato Nisihara2 and Luiz Roberto Kotze1
1Service of Gastroenterology. Hospital Universitário Cajuru. Pontifícia Universidade Católica do Paraná. Brazil.
2Department of Medicine. Universidade Positivo. Curitiba-Paraná, Brazil
References
1. Kotze LMS. Celiac disease in Brazilian patients: associations, complications and causes of death. Forty-years of clinical experience. Arq Gastroenterol 2009;46:261-9. [ Links ]
2. Bardella MT, Fredella C, Saladino V, Trovato C, Cesana BM, Quatrini M, et al. Gluten intolerance: Gender- and age-related differences in symptoms. Scad J Gastroenterol 2005;40:15-9. [ Links ]
3. Caproni M, Antiga E, Melani L, Fabbri P. The Italian Group for Cutaneous Immunopathology. Guidelines for the diagnosis and treatment of dermatitis herpetiformis. J Eur Acad Dermatol Venereol 2009;23:633-8. [ Links ]
4. Zone JJ. Skin manifestations of celiac disease. Gastroenterology 2005;128:S87-91. [ Links ]
5. Oxentenko AS, Murray JA. Celiac disease and dermatitis herpetiformis: The spectrum of gluten sensitive enteropathy. Int J Dermatol 2002;42:585-7. [ Links ]
6. Ortona E, Margutti P, Matarrese P, Franconi F, Malorni W. Redox state, cell death and autoimmune diseases: A gender perspective. Autoimmun Rev 2008;7:579-84. [ Links ]
7. Nussinovitch U, Shoenfeld Y. The role of gender and organ specific autoimmunity. Autoimmun Rev 2012;11:A377-85. [ Links ]
8. Alonso-Llamazares J, Gibson LE, Rogers III RS. Clinical, pathologic, and immunopathological features of dermatitis herpetiformis: Review of the Mayo Clinic experience. Int J Dermatol 2007;46:910-9. [ Links ]
9. Hervonen K, Vornanen M, Kautiainen H, Collin P, Reunala T. Lymphoma in patients with dermatitis herpetiformis and their first-degree relatives. Brit J Dermatol 2005;152:82-6. [ Links ]
10. Bolontin D, Petronic-Rosic V. Dermatitis herpetiformis: part I. Epidemiology, pathogenesis, and clinical presentation. J Am Acad Dermatol 2011; 64:1017-24. [ Links ]