My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 n.1 Madrid Jan. 2015
LETTERS TO THE EDITOR
Correlation between location of amyloid deposits and endoscopic and clinical manifestations in symptomatic gastrointestinal amyloidosis
Correlación entre la localización del depósito amiloide y las manifestaciones endoscópicas y clínicas en amiloidosis digestiva sintomática
Key words: Gastrointestinal amyloidosis. Gastrointestinal endoscopy. Clinical manifestations.
Palabras clave: Amiloidosis digestiva. Endoscopia digestiva. Manifestaciones clínicas.
Dear Editor,
Amyloidosis is defined as the presence of an amorphous homogenous extracellular deposit of a fibril-structured protein polysaccharide complex called amyloid substance, which leads to alterations in organ structure and functionality (1). This deposit may be local or systemic, with the latter being more common.
We present a retrospective descriptive study of 24 patients with symptomatic gastrointestinal amyloidosis who were diagnosed in our service between 2002 and 2011.
Our objective was to try and establish an association between the histological type and location of the amyloid deposit with the endoscopic findings.
The diagnosis of amyloidosis of the gastrointestinal tract is made by histopathology study of endoscopic biopsies using Congo red stain (2,3). We excluded those patients in whom duodenal or rectal biopsies were done in patients with no gastrointestinal symptoms who underwent gastrointestinal biopsy to confirm the diagnosis of systemic amyloidosis, as well as those patients who had gastrointestinal symptoms but did not undergo biopsy. For the statistical analysis, nonparametric methods such as the Wilcoxon W for quantitative variables and Fisher's test for qualitative variables were used, as well as the Chi-squared test where applicable.
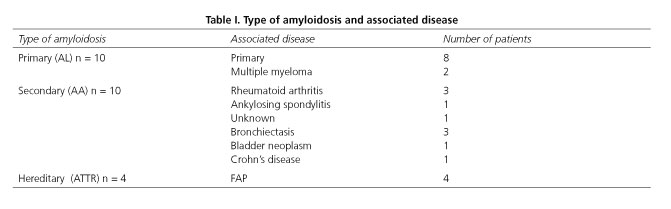
The population studied consisted of 13 women and 11 men with a mean age at diagnosis of 62.04 ± 13.3 (range 35-81) years. The mean age for primary amyloidosis (AL) was 62.9 ± 12.2, for secondary amyloidosis (AA) it was 66.3 ± 13.8 and in the familial amyloid polyneuropathy group it was 49.25 ± 14.9.
Amyloidosis-associated disease can be seen in table I.
It is already known that gastrointestinal tract involvement is very common and is usually subclinical, with the small intestine most often being affected (4-6). Diarrhea is the most frequent clinical manifestation, which was also the case in our patients (12/24, 50 %). Table II shows the remaining symptoms as they relate to the type of amyloidosis.
The kidney is the most affected extraintestinal site. Thirteen patients, 10 with AA amyloidosis plus three with AL amyloidosis, presented with renal failure at the moment of amyloidosis diagnosis, with hemodialysis required in 9 of them.
With regards to survival, all patients with FAP underwent transplant (two of which were domino transplants), with only one expiring due to transplant-related complications, while the other 3 are still alive following a mean post-transplant follow-up of 35 months.
Thirteen of the 20 remaining patients (with AA and AL amyloidosis) have expired, with a one-year survival of 60 %.
Regarding the location of the deposit and the endoscopic findings, we found that among the patients with submucosal infiltration, five had a thickened or nodular mucosa on endoscopy, one patient has superficial edema-like lesions or erosions and the remaining 4 did not have any alterations on endoscopy.
Among the patients with lamina propria infiltration, superficial lesions such as edema, friability, erosions and ulcers predominated (11/14, 78.5 %). One patient had a nodular mucosa and two patients had normal endoscopies.
We have found that when the mucosa is granular or thickened, submucosal infiltration predominates (5/6, 83.3 %) (p = 0.028, OR: 14.2 [1.2-142], while in patients with lamina propria infiltration (11/12, 91.6 %) superficial lesions predominate (p = 0.001; OR: 33 [2.9-374]).
Conversely, we did not find an association between the type of amyloidosis and the endoscopic findings.
Therefore, our series describes a significant correlation between the location of the amyloid and the endoscopic findings given that 92.3 % of patients with superficial lesions on endoscopy had an amyloid deposit in the lamina propria on pathology studies. Meanwhile, 85.7 % of cases of granular or thickened mucosa had a submucosal deposit.
To date, there is only one study (7) that associates amyloid deposits and endoscopic manifestations. This study revealed that the AL amyloid deposit usually occurs on the submucosal level and it manifests endoscopically as mucosal thickening, polyps, nodules that manifest clinically as constipation, mechanical obstruction or chronic intestinal pseudo-obstruction. Tada et al. (7,8) found an association between AL amyloidosis, submucosal deposits and subocclusive symptoms in 37.5 % of cases. Meanwhile, out of the 20 AA amyloidosis patients, 70 % had lamina propria involvement and a correlation with the presence of diarrhea.
In conclusion, amyloidosis continues to be an entity with a poor prognosis in patients with gastrointestinal signs or symptoms. In our series, we found a correlation between the location of the amyloid deposit and the endoscopic findings, but this did not serve to differentiate which amyloid substance was present as there was no correlation between the type of amyloidosis and the location of the infiltration.
Alfonso Alcalde-Vargas, Eduardo Leo-Carnerero, Norberto Rojas-Mercedes,
Claudio Trigo-Salado, José Manuel Herrera-Justiniano and José Luis Márquez-Galán
Department of Gastroenterology. Hospital Virgen del Rocío. Sevilla, Spain
References
1. Glenner GG. Amyloid deposits and amyloidosis. The B-fibrilloses. N Engl J Med 1980;302:1283-333. [ Links ]
2. Westermark P. Aspects on human amyloid forms and their fibril polypeptides. FEBS J 2005;272:5942-9. [ Links ]
3. Levine RA. Amyloid disease of the liver: Correlation of clinical, functional, and morphological features in fortyseven patients. Am J Med 1962;33:349-57. [ Links ]
4. Sattianayagam PT, Hawkins PN, Gillmore JD. Systemic amiloidosis and the gastrointestinal tract. Nat Rev Gastroenterol Hepatol 2009;6:608-17. [ Links ]
5. Lewis WD, Skinner M. Liver transplantation for familial amyloidotic polyneuropathy: A potential curative treatment. Int J Exp Clin Invest 1994;1:143-4. [ Links ]
6. Lachmann HJ, Goodman HJ, Gilbertson JA, Gallimore JR, Sabin CA, Gillmore JD, et al. Natural history and outcome in systemic AA amyloidosis. N Engl J Med 2007;356:2361-71. [ Links ]
7. Tada S, Iida M, Iwashita A, Matsui T, Fuchigami T, Yamamoto T, et al. Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis. Gastrointest Endosc 1990;36:10-4. [ Links ]
8. Tada S, Iida M, Yao T, Kawakubo K, Yao T, Okada M, et al. Endoscopic features in amyloidosis of the small intestine: Clinical and morphologic differences between chemical types of amyloid protein. Gastrointest Endosc 1994;40:45-50. [ Links ]











 text in
text in