Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.4 Madrid abr. 2015
REVIEW
Endoscopic ultrasound in the diagnosis of chronic pancreatitis
Julio Iglesias-García1, José Lariño-Noia1, Björn Lindkvist1,2 and J. Enrique Domínguez-Muñoz1
1Department of Gastroenterology and Foundation for Research in Digestive Diseases (FIENAD). Hospital Universitario de Santiago. Santiago de Compostela. A Coruña, Spain.
2Institute of Medicine. Sahlgrenska Academy. University of Gothenburg. Gothenburg, Sweden
Disclosures: Dr. Julio Iglesias-García is international advisor of Cook-Medical. Dr. J. Enrique Domínguez-Muñoz has acted as international advisor of Pentax Medical Company.
ABSTRACT
Diagnosis of chronic pancreatitis (CP) remains a challenge. Endoscopic ultrasound (EUS) can be considered nowadays as the technique of choice for the morphological diagnosis of this disease. More than three or four EUS defined criteria of CP need to be present for the diagnosis of the disease. The development of the more restrictive Rosemont classification aims to standardize the criteria, assigning different values to different features but its impact on the EUS-based diagnosis of CP is debatable. A combined use of endoscopic function test and EUS has even increased the diagnostic yield. Elastography and FNA may be also of help for diagnosing CP. EUS also provides with very valuable information on the severity of the disease, giving key information that may influence in the treatment. Differential diagnosis of solid pancreatic masses in the context of a CP is also challenging, EUS plays a key role in this context. It provides with the possibility of obtaining specimens for histopathological diagnosis. Nowadays, new developed techniques associated to EUS, like elastography and contrast enhancement, are also showing promising results for the differentiating between these pancreatic lesions.
Key words: Endoscopic ultrasound. Diagnosis. Chronic pancreatitis.
Introduction
Chronic pancreatitis (CP) is a progressive and irreversible inflammation of the pancreatic gland that ultimately leads to fibrosis and destruction of normal tissue resulting in morphological alterations and exocrine as well as endocrine dysfunction (1). The diagnosis is easy to establish in advanced stages of the disease, when the presence of pancreatic calcifications, atrophy of the gland and pancreatic duct dilation can be visualized by conventional imaging techniques such as abdominal ultrasound and computed tomography. Early CP, on the other hand, remains a major diagnostic challenge today. Pathological specimens from the pancreas are very difficult to obtain and there is no clear international consensus of a histological or clinical definition of CP.
Endoscopic retrograde cholangiopancreatography (ERCP) has previously been considered as the gold standard for the diagnosis of CP. However, due to the possible and serious complications related to the procedure and the fact that the parenchyma is not visualized, ERCP is no longer considered the method of choice (2). Among pancreatic function tests, the secretin test has been demonstrated to have a high sensitivity and specificity for CP (3). The use of this test has been limited since it is difficult to perform and not widely available (4). Endoscopic ultrasonography (EUS) has emerged as a promising diagnostic technique for pancreatic disease since it is able to detect pancreatic parenchymal and ductal changes with high sensitivity. Furthermore, fine needle biopsies can be obtained by EUS for cytological or histological evaluation, and CP related complications could be treated with EUS guided interventions. The use of EUS for the diagnosis of CP will be reviewed in this article.
EUS in the diagnosis of chronic pancreatitis
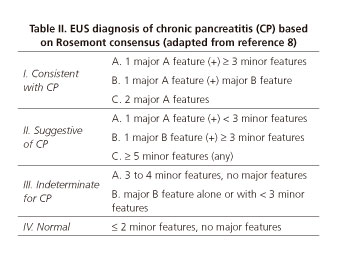
EUS has the ability to produce high-resolution ultrasonography images of the pancreas due to the proximity of the transducer to the gland, avoiding interference by air in the intestine. EUS diagnosis of CP is based on specific criteria that have been described by the International Working Group for Minimum Standard Terminology in Gastrointestinal Endoscopy (5). These comprise five parenchymal criteria (hyperechoic foci, hyperechoic strands, parenchymal lobularity, cysts, calcifications) and five ductal criteria (pancreatic duct dilation, pancreatic duct irregularity, hyperechoic pancreatic duct walls, visible pancreatic side branches, intraductal calcifications) (Fig. 1). The number of criteria that is needed to establish the diagnosis of CP and the relative weight of each criterion has been a matter of debate for several years. The first attempts to create an integrated evaluation of EUS based CP findings simply used the sum of positive criteria and defined EUS findings consistent with CP as a certain minimum number of positive criteria (6,7). In an attempt to allow for differentiated weighting of CP criteria and to harmonize EUS based diagnosis of CP, the Rosemont classification was published in 2009 (8). The Rosemont classification is a definition of EUS based CP criteria produced by a group of endosonography experts at an international consensus conference. Ductal and parenchymal EUS findings are divided into major A, major B and minor criteria (Table I). As opposed to the previous simple counting of criteria, the Rosemont classification gives different weight to different findings. Based on the number and character of positive EUS criteria, EUS evaluation is classified as "consistent with CP", "suggestive of CP", "indeterminate for CP", or "normal" (8) (Table II). This system agrees with the standard classification in 74% of cases, increasing to 84% when "suggestive of CP" was included as CP (8).
One of the most important weaknesses of EUS in the diagnosis of CP is concern about poor interobserver agreement (9). Interobserver agreement differs between EUS criteria. Duct dilation and lobularity (10) was demonstrated to have the highest agreement in one study while hyperechoic strands and parenchymal cysts were found to have the highest agreement in another study (11). Inter observer agreement for standard EUS classification versus Rosemont classification for CP has been evaluated in a multicenter study. Fourteen experts evaluated 50-recorded videos using the standard EUS criteria (CP diagnosis if ≥ 3) and the Rosemont classification (considering "suggestive of CP" and "consistent with CP" as positive findings). Kappa score for inter observer agreement on the Rosemont classification was 0.65, and the kappa score for standard classification was 0.54 (n.s.). Best agreement was noted for calcifications (standard scoring), pancreatic duct calcifications (Rosemont classification) and pancreatic duct dilation (both systems). The poorest agreement was seen for lobularity without honeycombing (Rosemont classification). Patients were correctly classified as definite CP in 91.2% of cases according to standard scoring and 83.5% according to Rosemont classification; as mild CP in 50% according to standard scoring and 42.9% according to Rosemont classification; and not CP in 83.3% and 95.2% of cases respectively (12). The inability of the Rosemont classification to improve inter-observer agreement compared to standard EUS criteria has thereafter been confirmed in a recent study (13). The use of radial or linear echoendoscopes does not have a significant impact on inter observer agreement (k = 0.50 and 0.61 respectively) (14).
EUS vs. pancreatic function test and EUS plus endoscopic function test
Pancreatic function test have been used for diagnosis of early CP. The pancreatic function test with the highest sensitivity for CP is the secretin/cholecystokinin (CCK) stimulation test with aspiration of duodenal content by a dreilling tube or an endoscope during at least 45-60 minutes. The sensitivity and specificity of this test for diagnosing CP both exceed 90% (4). A high agreement between EUS and the secretin test has been demonstrated in several studies. By using 1-2 EUS criteria for mild pancreatitis, 3-5 for moderate pancreatitis, and > 5 for severe forms, agreement between classic secretin test and EUS was 100% for normal parenchyma and severe disease, 50% for moderate CP, and 13% for mild disease (3). Stevens et al used 4 EUS criteria as cut-off and observed a sensitivity of around 70% and a specificity of around 90% of EUS for prediction of a pathological endoscopic function test, depending on if CCK or secretin was used to simulate pancreatic secretion (15). Comparison of EUS (3-5 criteria for diagnosis) and ERCP showed quite similar sensitivity (72% vs. 68%) and specificity (76% vs. 79%) for either mild or severe CP with the endoscopic secretin test as the reference. EUS worked significantly better for establishing the presence of pancreatic exocrine insufficiency (PEI) (16). Six criteria were needed to obtain the best specificity and best negative predictive value, however sensitivity decreased to only 26% (17,18).
A combined use of endoscopic function test and EUS has recently been brought forward as a sensitive and accurate method for early diagnosis of CP (19,20). The concept is theoretically appealing since both morphology and exocrine function is evaluated. A standard EUS is performed, secretin is administered intravenously and duodenal fluid is subsequently collected at 15, 30, and 45 min. In a study including 252 patients for suspected minimal change CP (no calcifications), 160 (63.5%) had both normal EUS and endoscopic function test results, excluding CP. Thirty-two patients (12.7%) had abnormal EUS and abnormal endoscopic test results, confirming the diagnosis. The remaining 60 patients had discordant results (21). Patients with abnormal EUS and normal endoscopic function test may have CP with preserved exocrine function, or a false positive result of EUS for CP. The significance of normal EUS with abnormal function test is uncertain, but may suggest a very early form of CP prior to the development of structural changes, or a false positive result of function test for CP (21). Pancreatic morphology can also be dynamically evaluated with EUS after secretin stimulation. The pancreatic duct dilates after secretin stimulation in the normal pancreas. Dynamic EUS has demonstrated reduced pancreatic duct compliance as a consequence of duct fibrosis in CP, most pronounced in the tail of the pancreas, and duct compliance is negatively associated with bicarbonate secretion (22).
EUS vs. ERCP
ERCP has previously been considered as the reference method for early diagnosis of CP. Early studies on EUS have used ERCP as gold standard for diagnosis of CP. These studies have demonstrated a good overall agreement between the tests and a sensitivity of 70-100% and a specificity of 80-100% of EUS (using > 2 criteria cut-off) (6,18). Ductal stones and parenchymal calcifications are the EUS findings that are associated with the highest probability of an abnormal ERCP. Later studies have demonstrated that ERCP may not be the appropriate reference method for early diagnosis of CP and that EUS actually may be more sensitive than ERCP (23). Kahl et al. identified 38 patients with normal ERCP but EUS findings suggesting CP in a cohort of 130 patients evaluated for known or suspected CP. During follow-up, 69% of these patients with initially normal findings on ERCP developed an abnormal pancreatogram (24).
EUS vs. magnetic resonance imaging
Magnetic resonance imaging (MRI) enhanced by gadolinium contrast after secretin stimulation together with magnetic resonance cholangiopancreatography (MRCP) is a highly accurate method for evaluation of CP (25). EUS has been compared with MRI/MRCP for the diagnosis of CP and similar sensitivity but a slightly superior specificity of EUS has been indicated (26). In the presence of both abnormal EUS and MRI/MRCP the specificity for CP diagnosis was 100% in that study (26). In our experience, there is a very good correlation between EUS and secretin MRCP in the evaluation of patients with a suspected CP both in the global evaluation for diagnosing the disease (both for parenchymal and ductal analysis). In fact, in 81% of the cases, information provided by both techniques was equivalent.
EUS vs. histology
Compared to pancreatic specimens, > 3 EUS standard criteria predict histological findings of CP (27). However, these EUS features have also been demonstrated in elderly persons without signs of CP (28) and in 59% of asymptomatic alcohol abusers (20). Using histologic findings from surgical specimens as reference, > 5 versus > 3 standard EUS criteria diagnosed CP with a sensitivity of 60% versus 87% and specificity of 83% versus 64% (29). Varadarajulu et al. demonstrated in a similar study where EUS findings were compared to histology from surgical specimens that hyperechogenic foci, stranding, lobularity or any ductal aberrations were the EUS features that were significantly associated with histological findings of CP. Four or more standard criteria was the cut-off for CP diagnosis that provided the best accuracy in that study (30). In yet another study on EUS findings versus surgical specimens, Chong et al. found that 3 or more criteria was the cut-off that best differentiated abnormal from normal pancreas (27). Standard EUS criteria appear as a poor predictor of histological severity in these studies. Varadarajulu et al. did not find any correlation between the number of EUS criteria and histological severity and Chong et al. found only a weak, although statistically significant, correlation between the number of EUS criteria and the histological fibrosis score (27,30). However, in a recent study, Leblanc et al. showed that certain EUS criteria were associated with a severe CP, as correlated with histological findings. These criteria were lobularity with honeycombing, hyperechoic foci with shadowing, dilated MPD, irregular MPD, and dilated side branches. Authors also state that the importance of pancreatic ductal changes should not be minimized in the evaluation of CP (31).
EUS-guided fine needle aspiration and/or fine needle biopsy
EUS-guided fine needle aspiration (FNA) and/or fine needle biopsy (FNB) has a clear and well investigated role in the differential diagnosis between mass forming chronic pancreatitis and pancreatic cancer but studies on the use of EUS guided tissue sampling in differentiating early CP from normal tissue are scares. The possible and severe complications related to the procedure and the lack of a generally agreed histologic definition of CP further limits today the use of EUS-guided FNA/FNB in the diagnosis of early CP. Hollerbach et al investigated the value of adding a 22-gauge needle FNA to standard EUS evaluation in a series of 37 patients with a suspicion of CP with ERCP as reference method. The addition of EUS-guided FNA improved the negative predictive value of EUS (32). In a small series of fourteen patients with alcohol related CP undergoing EUS-guided FNA, we have observed presence of inflammatory cells in all cases (33). Preserved pancreatic acini were observed in patients with mild to moderate EUS changes of CP. In contrast, biopsies from more severe cases (8-10 EUS criteria) showed only ductal epithelium and fibrosis (33). Thus, it is possible that EUS-guided FNA can be useful for both diagnosis and staging of CP. However, to date it is not clear if the benefits of FNA/FNB outweighs the risks for complications related to the procedure and the clinical use of FNA/FNB for diagnosis and staging of CP remains to be established.
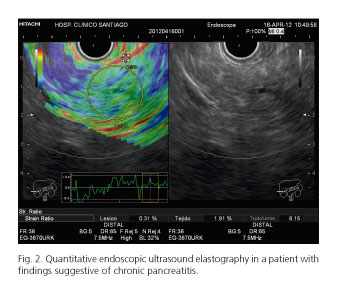
EUS-guided elastography and contrast enhancement
Elastography evaluates tissue strain resulting from compression and that strain is smaller in harder tissue than in softer tissue. Different tissue elasticity patterns are marked supplementary on the grey-color scale with different colors (blue for hard tissue and red for soft tissue). Today elastography can also be evaluated in a quantitative manner by calculating the ratio between the strain in the region of interest and a reference area in surrounding soft tissue (strain ratio) (34). The typical finding on qualitative elastography in CP is a heterogeneous coloration with green areas and blue strands, as opposed to normal pancreas that presents a homogeneous, predominantly green and yellow pattern (35). The accuracy of quantitative EUS-elastography for the diagnosis of CP has been recently investigated. A high correlation was found between the number of EUS criteria and the pancreatic strain ratio. In addition, a significant difference in strain ratio between different Rosemont classification categories was observed, with increasing strain ratio when passing from normal pancreas to indeterminate for CP to suggestive for CP to consistent for CP (36,37) (Fig. 2). More recently, a new study has shown a very good correlation between the strain ratio, as evaluated by quantitative EUS-elastography, and the probability of suffering from exocrine pancreatic insufficiency (38). The role of contrast enhanced EUS for the diagnosis of CP has not been yet well established. Only one study has evaluated the role of contrast enhanced EUS in this setting. Contrast enhanced EUS enhances the lobular pattern seen by conventional EUS in CP patients. Furthermore, the washout of contrast is markedly faster in CP patients compared to controls.
EUS for evaluating the severity degree of chronic pancreatitis
Visible side branches, duct dilation, duct irregularity, and calcifications have been demonstrated to be associated with severe CP on ERCP (39) according to the Cambridge classification (40). One study has shown that odds ratio for pancreatic exocrine insufficiency (PEI) (severe CP) by EUS was, in the presence of minimal and severe structural changes 4.9 and 24, respectively (16). In a recent study, the probability of PEI in relation to EUS criteria of CP was analyzed. The percentage of patients with PEI increased linearly with the number of EUS criteria. The presence of intraductal calcifications, hyperechogenic foci with shadowing, and dilation of the main pancreatic duct were significantly and independently associated to PEI (Fig. 3). The probability of PEI in the presence of calculi in the main pancreatic duct is 80% and increases to 82.8% if, in addition, the main duct is dilated. Thus EUS allows predicting the probability of PEI and thus need for enzyme replacement therapy in patients with CP (41).
Differential diagnosis of mass forming chronic pancreatitis and pancreatic cancer
Differential diagnosis of solid pancreatic masses includes primary or secondary pancreatic tumor, focal CP and autoimmune pancreatitis. Despite high-resolution images produced by conventional EUS, differentiation between benign inflammatory masses and malignant tumors based on B-mode images remains a challenge. EUS-FNA/FNB, contrast enhanced harmonic EUS and EUS elastography are new tools to improve of the diagnostic accuracy of EUS for the evaluation of solid pancreatic masses.
EUS-guided FNA and FNB
The role of EUS-guided FNA in the diagnosis of solid pancreatic tumors has been evaluated in several studies. Reported sensitivity and accuracy for malignancy ranges from 75 to 92% and from 79 to 92%, respectively (42). This accuracy may be even higher using on-site evaluation of the sample by an experienced pathologist (43). However, it should be kept in mind that the sensitivity of EUS-guided FNA for malignancy is lower (between 54% and 74%) if the lesion is detected in the context of CP compared to when the surrounding parenchyma is normal (44-47). Furthermore, in some cases EUS-guided FNA maybe not feasible due to technical difficulties or the EUS-FNA samples are of low quality for diagnosis. In total, EUS-guided FNA does not allow reaching the pathological diagnosis of pancreatic masses in 8% to 25% of cases (48). In order to optimize tissue retrieval of EUS-guided biopsy, various new needles, like Tru-Cut and the new ProcoreTM have been tested (49).
EUS-guided elastography
Pathological processes like cancer and fibrosis alter tissue elasticity and will therefore induce changes in elastographic appearance. Qualitative elastography can differentiate malignant from benign solid pancreatic lesions with a sensitivity, specificity, positive and negative predictive values, and overall accuracy of 100%, 85.5%, 90.7%, 100% and 94.0%, respectively (50). Quantitative EUS-elastography is a more objective and accurate method than qualitative EUS-elastography. In a previous study including 86 consecutive patients with solid pancreatic masses, the sensitivity and specificity of quantitative EUS-elastography for the differentiation of malignant from benign lesions were 100% and 92.9% respectively (51) (Fig. 4). Mean hue histogram value is an alternative measure for quantitative elastography. A first study showed a sensitivity, specificity, and accuracy in differentiation of malignant from benign masses of 91.4%, 87.9%, and 89.7%, respectively (52). A multicenter study, using the same methodology, showed a sensitivity of 93.4%, a specificity of 66.0%, a positive predictive value of 92.5%, a negative predictive value of 68.9%, and an overall accuracy of 85.4% for the diagnosis of pancreatic malignancy (53).
Contrast enhanced EUS
Administration of contrast agents is another way to improve EUS-based diagnosis of solid pancreatic tumors. Today, the most widely used is contrast enhanced harmonic EUS (CEHEUS), technique that detects signals from micro bubbles delivered by new contrast agents in vessels with very slow flow without the burden of Doppler-related artifacts (54). With this technique pancreatic cancer appears as a low enhanced lesion with a rapid washout, while mass forming CP uses to appear as an isoenhanced lesion. A hypoenhanced pattern has a high sensitivity for adenocarcinoma (89-96%) but the specificity is lower since advanced mass-forming CP also may be hyperenhanced (55,56). Tissue perfusion after contrast administration can be quantified using time intensity curve analysis. A recent study has indicated that this quantitative method may have a high sensitivity and specificity for differentiation between pseudotumoral CP and pancreatic cancer (57). Further larger multicenter studies are warranted in order to investigate the role of quantitative and qualitative contrast enhanced EUS in the diagnosis of pancreatic cancer.
Conclusions
Diagnosis of CP remains a challenge. EUS can be considered nowadays as the technique of choice for the morphological diagnosis of this disease. More than three or four EUS defined criteria of CP need to be present for the diagnosis of the disease. The development of the more restrictive Rosemont classification aims to standardize the criteria, assigning different values to different features but its impact on the EUS-based diagnosis of CP is debatable. A combined use of endoscopic function test and EUS has even increased the diagnostic yield for the diagnosis of CP. Elastography and FNA may be of help for diagnosing CP. EUS also provides with very valuable information on the severity of the disease, giving key information that may influence in the treatment.
Differential diagnosis of solid pancreatic masses in the context of a CP is also challenging, EUS plays a key role in this context. It provides with the possibility of obtaining specimens for histopathological diagnosis, improving its diagnostic yield. Nowadays, new developed techniques associated to EUS, like elastography and contrast enhancement, are also showing promising results for the differentiating between these pancreatic lesions.
References
1. Sarles H. Definitions and classifications of pancreatitis. Pancreas 1991;6(4):470-4. [ Links ]
2. Choueiri NE, Balci NC, Alkaade S, et al. Advanced imaging of chronic pancreatitis. Current gastroenterology reports 2010;12:114-20. [ Links ]
3. Catalano MF, Lahoti S, Geenen JE, et al. Prospective evaluation of endoscopic ultrasonography, endoscopic retrograde pancreatography, and secretin test in the diagnosis of chronic pancreatitis. Gastrointest Endosc 1998;48:11-7. [ Links ]
4. Dominguez Munoz JE. Diagnosis of chronic pancreatitis: Functional testing. Best Pract Res Clin Gastroenterol 2010;24:233-41. [ Links ]
5. Aabakken L, Rembacken B, LeMoine O, et al. Minimal standard terminology for gastrointestinal endoscopy - MST 3.0. Endoscopy 2009;41:727-8. [ Links ]
6. Wiersema MJ, Hawes RH, Lehman GA, et al. Prospective evaluation of endoscopic ultrasonography and endoscopic retrograde cholangiopancreatography in patients with chronic abdominal pain of suspected pancreatic origin. Endoscopy 1993;25:555-64. [ Links ]
7. Wiersema MJ, Wiersema LM. Endosonography of the pancreas: Normal variation versus changes of early chronic pancreatitis. Gastrointest Endosc Clin N Am 1995;5:487-96. [ Links ]
8. Catalano MF, Sahai A, Levy M, et al. EUS-based criteria for the diagnosis of chronic pancreatitis: the Rosemont classification. Gastrointest Endosc 2009;69:1251-61. [ Links ]
9. Kalmin B, Hoffman B, Hawes R, et al. Conventional versus Rosemont endoscopic ultrasound criteria for chronic pancreatitis: Comparing interobserver reliability and intertest agreement. Can J Gastroenterol 2011;25:261-4. [ Links ]
10. Wallace MB, Hawes RH, Durkalski V, et al. The reliability of EUS for the diagnosis of chronic pancreatitis: Interobserver agreement among experienced endosonographers. Gastrointest Endosc 2001;53:294-9. [ Links ]
11. Gardner TB, Gordon SR. Interobserver agreement for pancreatic endoscopic ultrasonography determined by same day back-to-back examinations. J Clin Gastroenterol 2011;45:542-5. [ Links ]
12. Stevens T, Lopez R, Adler DG, et al. Multicenter comparison of the interobserver agreement of standard EUS scoring and Rosemont classification scoring for diagnosis of chronic pancreatitis. Gastrointest Endosc 2010;71:519-26. [ Links ]
13. Del Pozo D, Poves E, Tabernero S, et al. Conventional versus Rosemont endoscopic ultrasound criteria for chronic pancreatitis: interobserver agreement in same day back-to-back procedures. Pancreatology 2012;12:284-7. [ Links ]
14. Stevens T, Zuccaro G, Jr., Dumot JA, et al. Prospective comparison of radial and linear endoscopic ultrasound for diagnosis of chronic pancreatitis. Endoscopy 2009;41:836-41. [ Links ]
15. Stevens T, Dumot JA, Zuccaro G, Jr., et al. Evaluation of duct-cell and acinar-cell function and endosonographic abnormalities in patients with suspected chronic pancreatitis. Clin Gastroenterol Hepatol 2009;7:114-9. [ Links ]
16. Stevens T, Conwell DL, Zuccaro G, Jr., et al. Comparison of endoscopic ultrasound and endoscopic retrograde pancreatography for the prediction of pancreatic exocrine insufficiency. Dig Dis Sci 2008;53:1146-51. [ Links ]
17. Conwell DL, Zuccaro G, Purich E, et al. Comparison of endoscopic ultrasound chronic pancreatitis criteria to the endoscopic secretin-stimulated pancreatic function test. Dig Dis Sci 2007;52:1206-10. [ Links ]
18. Sahai AV, Zimmerman M, Aabakken L, et al. Prospective assessment of the ability of endoscopic ultrasound to diagnose, exclude, or establish the severity of chronic pancreatitis found by endoscopic retrograde cholangiopancreatography. Gastrointest Endosc 1998;48:18-25. [ Links ]
19. Stevens T, Conwell DL, Zuccaro G, Jr., et al. A prospective crossover study comparing secretin-stimulated endoscopic and Dreiling tube pancreatic function testing in patients evaluated for chronic pancreatitis. Gastrointest Endosc 2008;67:458-66. [ Links ]
20. Stevens T, Conwell DL, Zuccaro G, Jr., et al. A randomized crossover study of secretin-stimulated endoscopic and dreiling tube pancreatic function test methods in healthy subjects. Am J Gastroenterol 2006;101:351-5. [ Links ]
21. Stevens T, Dumot JA, Parsi MA, et al. Combined endoscopic ultrasound and secretin endoscopic pancreatic function test in patients evaluated for chronic pancreatitis. Dig Dis Sci 2010;55:2681-7. [ Links ]
22. Gardner TB, Purich ED, Gordon SR. Pancreatic duct compliance after secretin stimulation: A novel endoscopic ultrasound diagnostic tool for chronic pancreatitis. Pancreas 2012;41:290-4. [ Links ]
23. Hastier P, Buckley MJ, Francois E, et al. A prospective study of pancreatic disease in patients with alcoholic cirrhosis: Comparative diagnostic value of ERCP and EUS and long-term significance of isolated parenchymal abnormalities. Gastrointest Endosc 1999;49:705-9. [ Links ]
24. Kahl S, Glasbrenner B, Leodolter A, et al. EUS in the diagnosis of early chronic pancreatitis: A prospective follow-up study. Gastrointest Endosc 2002;55:507-11. [ Links ]
25. Balci C. MRI assessment of chronic pancreatitis. Diagn Interv Radiol 2011;17:249-54. [ Links ]
26. Pungpapong S, Wallace MB, Woodward TA, et al. Accuracy of endoscopic ultrasonography and magnetic resonance cholangiopancreatography for the diagnosis of chronic pancreatitis: A prospective comparison study. J Clin Gastroenterol 2007;41:88-93. [ Links ]
27. Chong AK, Hawes RH, Hoffman BJ, et al. Diagnostic performance of EUS for chronic pancreatitis: A comparison with histopathology. Gastrointest Endosc 2007;65:808-14. [ Links ]
28. Bhutani MS, Arantes VN, Verma D, et al. Histopathologic correlation of endoscopic ultrasound findings of chronic pancreatitis in human autopsies. Pancreas 2009;38:820-4. [ Links ]
29. Zimmerman MJ, Mishra G, Lewin D, et al. Comparison of EUS findings with histopathology in chronic pancreatitis. Gastrointest Endosc 1997;45:AB185. [ Links ]
30. Varadarajulu S, Eltoum I, Tamhane A, et al. Histopathologic correlates of noncalcific chronic pancreatitis by EUS: A prospective tissue characterization study. Gastrointest Endosc 2007;66:501-9. [ Links ]
31. LeBlanc JK, Chen JH, Al-Haddad M, et al. Endoscopic ultrasound and histology in chronic pancreatitis: How are they associated? Pancreas 2014;43:440-4. [ Links ]
32. Hollerbach S, Klamann A, Topalidis T, et al. Endoscopic ultrasonography (EUS) and fine-needle aspiration (FNA) cytology for diagnosis of chronic pancreatitis. Endoscopy 2001;33:824-31. [ Links ]
33. Iglesias-Garcia J, Abdulkader I, Larino-Noia J, et al. Histological evaluation of chronic pancreatitis by endoscopic ultrasound-guided fine needle biopsy. Gut 2006;55:1661-2. [ Links ]
34. Iglesias Garcia J, Lindkvist B, Larino Noia J, et al. Endoscopic ultrasound elastography. Endosc Ultrasound 2012;1:8-16. [ Links ]
35. Janssen J, Schlorer E, Greiner L. EUS elastography of the pancreas: feasibility and pattern description of the normal pancreas, chronic pancreatitis, and focal pancreatic lesions. Gastrointest Endosc 2007;65:971-8. [ Links ]
36. Iglesias-Garcia J, Larino-Noia J, Dominguez-Munoz JE. Elastography in the evaluation of chronic pancreatitis. Gastroenterol Hepatol 2011;34:629-34. [ Links ]
37. Iglesias-Garcia J, Dominguez-Munoz JE, Castineira-Alvarino M, et al. Quantitative elastography associated with endoscopic ultrasound for the diagnosis of chronic pancreatitis. Endoscopy 2013;45:781-8. [ Links ]
38. Dominguez-Munoz JE, Iglesias-Garcia J, Castineira Alvarino M, et al. EUS elastography to predict pancreatic exocrine insufficiency in patients with chronic pancreatitis. Gastrointest Endosc 2015; 81:136-42. [ Links ]
39. Irisawa A, Katakura K, Ohira H, et al. Usefulness of endoscopic ultrasound to diagnose the severity of chronic pancreatitis. J Gastroenterol 2007;42(Supl. 17):90-4. [ Links ]
40. Sarner M, Cotton PB. Classification of pancreatitis. Gut 1984;25: 756-9. [ Links ]
41. Dominguez-Munoz JE, Alvarez-Castro A, Larino-Noia J, et al. Endoscopic ultrasonography of the pancreas as an indirect method to predict pancreatic exocrine insufficiency in patients with chronic pancreatitis. Pancreas 2012;41:724-8. [ Links ]
42. Iglesias Garcia J, Dominguez-Munoz JE. Endoscopic ultrasound-guided biopsy for the evaluation of pancreatic tumors. Gastroenterol Hepatol 2007;30:597-601. [ Links ]
43. Iglesias-Garcia J, Dominguez-Munoz JE, Abdulkader I, et al. Influence of on-site cytopathology evaluation on the diagnostic accuracy of endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) of solid pancreatic masses. Am J Gastroenterol 2011;106:1705-10. [ Links ]
44. Ardengh JC, Lopes CV, Campos AD, et al. Endoscopic ultrasound and fine needle aspiration in chronic pancreatitis: Differential diagnosis between pseudotumoral masses and pancreatic cancer. JOP 2007;8:413-21. [ Links ]
45. Barthet M, Portal I, Boujaoude J, et al. Endoscopic ultrasonographic diagnosis of pancreatic cancer complicating chronic pancreatitis. Endoscopy 1996;28:487-91. [ Links ]
46. Fritscher-Ravens A, Brand L, Knofel WT, et al. Comparison of endoscopic ultrasound-guided fine needle aspiration for focal pancreatic lesions in patients with normal parenchyma and chronic pancreatitis. Am J Gastroenterol 2002;97:2768-75. [ Links ]
47. Varadarajulu S, Tamhane A, Eloubeidi MA. Yield of EUS-guided FNA of pancreatic masses in the presence or the absence of chronic pancreatitis. Gastrointest Endosc 2005;62:728-36. [ Links ]
48. Iglesias-Garcia J, Lindkvist B, Larino-Noia J, et al. The role of EUS in relation to other imaging modalities in the differential diagnosis between mass forming chronic pancreatitis, autoimmune pancreatitis and ductal pancreatic adenocarcinoma. Rev Esp Enferm Dig 2012; 104:315-21. [ Links ]
49. Iglesias-Garcia J, Poley JW, Larghi A, et al. Feasibility and yield of a new EUS histology needle: results from a multicenter, pooled, cohort study. Gastrointest Endosc 2011;73:1189-96. [ Links ]
50. Iglesias-Garcia J, Larino-Noia J, Abdulkader I, et al. EUS elastography for the characterization of solid pancreatic masses. Gastrointest Endosc 2009;70:1101-8. [ Links ]
51. Iglesias-Garcia J, Larino-Noia J, Abdulkader I, et al. Quantitative endoscopic ultrasound elastography: An accurate method for the differentiation of solid pancreatic masses. Gastroenterology 2010;139:1172-80. [ Links ]
52. Saftoiu A, Vilmann P, Gorunescu F, et al. Neural network analysis of dynamic sequences of EUS elastography used for the differential diagnosis of chronic pancreatitis and pancreatic cancer. Gastrointest Endosc 2008;68:1086-94. [ Links ]
53. Saftoiu A, Vilmann P, Gorunescu F, et al. Accuracy of endoscopic ultrasound elastography used for differential diagnosis of focal pancreatic masses: A multicenter study. Endoscopy 2011;43:596-603. [ Links ]
54. Kitano M, Kudo M, Sakamoto H, et al. Endoscopic ultrasonography and contrast-enhanced endoscopic ultrasonography. Pancreatology 2011;11(Supl. 2):28-33. [ Links ]
55. Napoleon B, Alvarez-Sanchez MV, Gincoul R, et al. Contrast-enhanced harmonic endoscopic ultrasound in solid lesions of the pancreas: Results of a pilot study. Endoscopy 2010;42:564-70. [ Links ]
56. Fusaroli P, Spada A, Mancino MG, et al. Contrast harmonic echo-endoscopic ultrasound improves accuracy in diagnosis of solid pancreatic masses. Clin Gastroenterol Hepatol 2010;8:629-34. [ Links ]
57. Gheonea DI, Streba CT, Ciurea T, et al. Quantitative low mechanical index contrast-enhanced endoscopic ultrasound for the differential diagnosis of chronic pseudotumoral pancreatitis and pancreatic cancer. BMC Gastroenterol 2013;13:2. [ Links ]
![]() Correspondence:
Correspondence:
Julio Iglesias-García.
Gastroenterology Department.
Foundation for Research in Digestive Diseases (FIENAD).
Hospital Universitario de Santiago.
c/ Choupana, s/n.
15706 Santiago de Compostela. A Coruña, Spain
e-mail:
julio.iglesias.garcia@sergas.es
Received: 23-12-2014
Accepted: 21-01-2015