Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.4 Madrid abr. 2015
PICTURES IN DIGESTIVE PATHOLOGY
An elderly woman with obstructive symptoms: A surprising diagnosis
Teresa Pinto-Pais, Rolando Pinho, Adélia Rodrigues and João Carvalho
Department of Gastroenterology and Hepatology. Centro Hospitalar de Gaia/Espinho. Gaia, Portugal
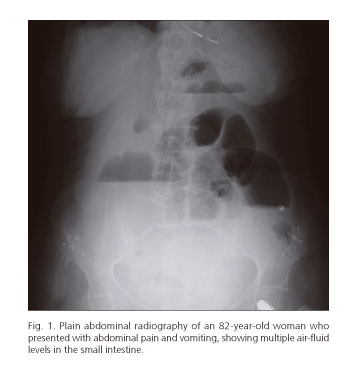
An 82-year-old woman was admitted with 24-hour colicky abdominal pain and vomiting. She reported three months of nausea, abdominal pain and distension, without fever, hematoquezia or weight loss. Her past medical history was mostly unremarkable. Of note, she denied non-steroid anti-inflammatory drugs (NSAIDs) consumption. Physical examination revealed diffuse abdominal tenderness and hyperactive bowel sounds, without peritoneal signs. Laboratory investigation disclosed iron-deficiency anaemia (haemoglobin 10.2 g/dl), leucocytosis (17,000/µL) and elevated C-reactive protein (6.51 mg/dL, normal range < 0.5 mg/dL). Abdominal X-ray displayed multiple air-fluid levels in the small intestine (Fig. 1). Subsequent computed tomography scan revealed several small-bowel stenotic segments, with concentric wall thickening, intense mucosal enhancement, and pre-stenotic dilatation (Fig. 2). Serum and faecal microbiological assays were negative. We proceeded to perform an anterograde single-balloon enteroscopy (SBE). Several ulcerated luminal strictures (Fig. 3) and irregularly shaped ulcers (Fig. 4) were observed; the interposed mucosa was intact. Biopsies revealed irregular villous architecture, discontinuous inflammation and focal crypt irregularity (Fig. 5); acid-fast bacilli smear and culture were negative. The diagnosis of stricturing small-bowel Crohn's disease (CD) was established by clinical evaluation and a combination of endoscopic, histological, radiological and biochemical investigations (A3L1B2, Montréal classification). The patient recovered uneventfully with conservative management. She was started on immunosuppressive therapy with azathioprine.
Diagnosis of inflammatory bowel disease in this age group is difficult because it can be easily confused with other diseases, including infections, ischemia, vasculitis, cancer and drug-associated enteritis, particularly NSAIDs (1). Prior studies describing elderly-onset CD are limited to small number of patients. Even in Dr. Crohn's own experience, only 7 out of 530 patients were diagnosed after age 60 years (2). Although CD has a bimodal distribution in incidence, very few are diagnosed beyond the eighth decade (3). In this case, assessment of small-bowel with SBE was crucial. Current guidelines recommend that in the suspicion of stricturing CD, direct visualization by balloon-assisted enteroscopy allows discrimination of active inflammation within the stenotic segment, and is the method of choice to obtain endoscopic and histological confirmation (4,5).
References
1. Picco MF, Cangemi JR. Inflammatory bowel disease in the elderly. Gastroenterol Clin North Am 2009;38:447-62. [ Links ]
2. Freeman HJ. Crohn's disease initially diagnosed after age 60 years. Age Ageing 2007;36:587-9. [ Links ]
3. Ruel J, Ruane D, Mehandru S, et al. IBD across the age spectrum-is it the same disease? Nat Rev Gastroenterol Hepatol 2014;11:88-98. [ Links ]
4. Pohl J, Delvaux M, Ell C, et al. European Society of Gastrointestinal Endoscopy (ESGE) Guidelines: Flexible enteroscopy for diagnosis and treatment of small-bowel diseases. Endoscopy 2008;40:609-18. [ Links ]
5. Annese V, Daperno M, Rutter MD, et al. European Crohns and Colitis Organization (ECCO) evidence based consensus for endoscopy in inflammatory bowel disease. J Crohns Colitis 2013;7:982-1018. [ Links ]