My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 n.5 Madrid May. 2015
CASE REPORTS
Epiphrenic and middle esophageal diverticula: A rare cause of esophageal dysphagia. Esophageal high resolution manometry findings
Divertículos epifrénicos y medio esofágicos: una causa poco frecuente de disfagia esofágica. Hallazgos en la manometría esofágica de alta resolución
Constanza Ciriza-de-los-Ríos, Fernando Canga-Rodríguez-Valcárcel, José Modesto Dutari-Valdés and Isabel Castel-de-Lucas
Department of Gastroenterology. Hospital Universitario 12 de Octubre. Madrid, Spain
RESUMEN
Los divertículos esofágicos (DE) constituyen una patología poco frecuente siendo en su mayoría asintomáticos. Cuando ocasionan síntomas, la disfagia suele ser el más frecuente como consecuencia del tamaño del divertículo y de las alteraciones de la motilidad concomitantes. La manometría de alta resolución (MAR) permite diagnosticar con mayor precisión los trastornos motores subyacentes que se asocian con los DE y comprender su mecanismo fisiopatogénico. Se presentan seis pacientes con disfagia que fueron diagnosticados de DE asociado a un trastorno motor esofágico en la MAR.
Palabras clave: Divertículos esofágicos. Disfagia. Manometría esofágica de alta resolución.
Introduction
Esophageal diverticula (ED) constitute a rare pathology, with a prevalence ranging between 0.06% and 4% (1,2). According to its anatomical location it is classified as pharyngo-esophageal, middle esophageal and epiphrenics ED (3). The pathophysiologic mechanism differs in diverticula caused by traction, due to an inflammatory process involving the esophagus, or pulsion, associated with a concomitant motility disorder (4-6).
Case report
Case report 1
A 58-year-old male, without relevant clinical antecedents, presented with progressive esophageal dysphagia in the last 3 months. Two years earlier, he had presented an episode of food impaction. Barium esophagogram (BE) detected a saccular image well delineated of 9 cm, with a hydro-aero level, in the lower esophageal third (Fig. 1A). Thoracic-abdominal computed tomography (CT) corroborated the findings described in the BE (Fig. 1B). The gastroscopy showed a dual lumen image large in size with semi-solid food content inside (Fig. 1C).
Case report 2
A 78-years-old male patient with no clinical antecedents was forwarded from ear-nose-throat department for pharyngo-laryngeal foreign body sensation to rule out GERD. The BE revealed the presence of a saccular image in the epiphrenic region (Fig. 1D), which was confirmed endoscopically.
Case report 3
A 77-year-old male, with clinical antecedents of chronic hepatitis C and hiatal hernia, presenting with progressive esophageal dysphagia over the last 6 months associated with occasional episodes of food regurgitation and heartburn. The BE identified a 3 cm saccular image, located in the last 10 cm of the esophagus and a sliding hiatal hernia (Fig. 2A). Upper endoscopy confirmed the presence of a diverticulum containing food inside, located 30 cm from the incisors (Fig. 2B).
Case report 4
A 68-year-old woman, diagnosed with systemic lupus erythematosus (SLE), presenting with progressive esophageal dysphagia over the last two months, with frequent episodes of food regurgitation and 10 kg weight loss. The thoracic CT showed esophageal lumen dilatation at the height of the carina, with a diameter of 5.2 x 3.1 cm and food content inside. The EB detected a saccular image of 4.5 x 3.7 cm in the middle esophagus that compressed the esophageal lumen diminishing the intra-luminal esophageal caliber with slowing of the barium pass at this location (Fig. 2C). An upper endoscopy identified a large esophageal diverticulum located 25 cm from the incisors with food inside. The esophageal biopsies were consistent with amyloidosis AA.
Case report 5
A 68-year-old woman with chronic renal failure antecedents presented with progressive esophageal dysphagia to solids and liquids over two years and bronchoaspiration episodes. EB detected tertiary contractile activity in the lower esophagus and an ED in the inferior and right posterior side of 2.9 x 2.8 cm of diameter (Fig. 3A) this was confirmed with endoscopic examination.
Caso report 6
A 68-year-old woman with antecedents of total thyroidectomy for endothoracic multinodular goiter, pill induced esophagitis in 2011, ED (Fig. 3B) and small hiatal hernia. She presented with dysphagia, mainly to liquids that provoked her admission into hospital for bronchoaspiration on 3 occasions. In the last admission we confirmed the ED located at 28 cm from the incisors by upper endoscopy (Fig. 3C).
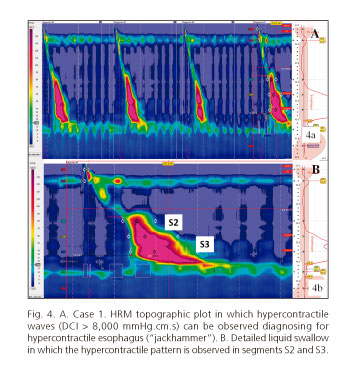
The six patients described underwent a high-resolution manometry (HRM) (Manoscan; Given) that identified a concomitant esophageal motor disorder (EMD) in all cases. The manometric parameters for all of the patients are shown in table I; the reference values used were the current Chicago classification (7). The patient in the first case presented hypercontractile contractions at the esophageal segments S2 and S3, being compatible with the manometric diagnosis of hypercontractile esophagus ("jackhammer" type) (Fig. 4). The HRM of the second patient showed a distal esophageal spasm, with involvement at the level of the S3 segment (Fig. 5A). In the third case, the HRM revealed a EMD weak peristalsis with small breaks in the isobaric contour of 20 mmHg (50% of contractions); also the waves had a prolonged duration and morphology of double and triple peaks in the esophageal segment S3, in 56% and 11% of the swallows, respectively (Fig. 5B). The patient in the 4th case had outflow obstruction of the esophagogastric junction (EGJ) with features of achalasia subtype III (spastic) of probable secondary origin (Fig. 6 A and B); also, great duration of esophageal waves were observed in the S2 segment (about 30 cm of the nostril).
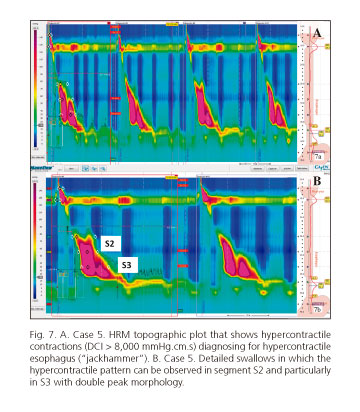
The patient in the 5th case had a hypercontractile ("jackhammer") motor disorder as well, with high amplitude waves in the segment S2 and particularly in S3 (Fig. 7). The 6th case patient, an EMD was observed consisting of outflow obstruction of the EGJ, as well as alteration in the contractile sequence in the anatomic area of the diverticulum where enlargement of the contraction was observed (between segments S2-S3) (Fig. 6 C and D).
The segment predominantly affected in the HRM, coincided with the location of the ED observed in the radiological and endoscopic studies in all cases. Following the completion of the HRM, five of the six patients were referred for assessment for surgical treatment. The first case patient was operated by diverticulectomy that was complicated with esophagopleural fistula that was treated with endoscopic placement of a fully covered self expanding metal stent (WallFlex®).
The second and third case patients decided to continue a conservative management, after rejecting the option for surgical treatment due to the morbidity and mortality associated with it.
The fourth case patient presented an episode of upper gastrointestinal bleeding. A large clot attached to the wall of the diverticulum was detected in the urgent gastroscopy. This accelerated the decision for surgical treatment of the diverticulum, once the episode of bleeding had surpassed. However, in the days after the bleeding event, the patient developed aspiration pneumonia and finally died.
The 5th case patient was treated surgically by performing thoracoscopic diverticulectomy and myotomy. The postoperative was torpid, complicated with mediastinitis caused by esophagopleural fistula that was treated with endoscopic placement of a fully covered self expanding metal stent (WallFlex®).
The 6th case patient was treated with endoscopic injection of botulinum toxin at the level of the EGJ to solve the functional outflow obstruction. This treatment was considered the best option considering the advanced age of the patient, improving the symptoms.
Discussion
The majority of diverticula are asymptomatic and are incidentally diagnosed during the investigation of lesser related symptoms. In 25% of the cases, the ED can be symptomatic, dysphagia being one of the predominant manifestations (8), as a result of the dimensions of the diverticulum and the concomitant esophageal motor disorder. The complications of ED, such as ulcers and bleeding, are infrequent (3). However, middle esophageal diverticula in particular, have a high prevalence of aspiration (45%), as well as a considerable potential for pulmonary complications that can be life threatening to the patients (15%) (9), as in one of our patients (case 4).
Epiphrenics and medium ED can be associated with a concomitant EMD in 35-100% (10) and 90% (11) cases, respectively. In the case of epiphrenic diverticula it was considered the protrusion of the mucosa and submucosa was caused by the increase in the esophageal pressure secondary to a motor disorder (8).
In our series of patients with ED a motor disorder in the esophageal body or in the EGJ was detected in all of them. Esophageal manometry is the gold standard for the diagnosis of the EMD (3). For many years, the conventional water-perfused manometry was the tool available to diagnose such disorders. However, in approximately 25% of the cases the EMD could pass unnoticed with this diagnostic technique. Today, the implementation of the HRM with the topographic plots obtained allows a higher accuracy in evaluation of the EGJ (12) and detection of segmental peristaltic defects, often unnoticed in the conventional study, though it obtains topographic plots of all of the esophagus by using a large number of sensors (4,13). In this respect, in our series of cases, we found pressure alterations in the anatomic area of the diverticulum, and we also identified the subjacent EMD, mainly spastic or hypercontractile, as well as alterations in the relaxation of the EGJ.
In conclusion, HRM clarifies the pathophysiology of the formation of the ED and can support the need to perform a myotomy added to the reconstructive surgical technique and its extension according to the EMD type and the affected esophageal segments as in the case of the 5th patient, in which surgical diverticulectomy and myotomy were performed.
References
1. Watanabe S, Matsuda K, Arima K, et al. Detection of subclinical disorders of the hypopharynx and larynx by gastrointestinal endoscopy. Endoscopy 1996;28:295-8. [ Links ]
2. Herbella F, Patty MG. Modern pathophysiology and treatment of esophageal diverticula. Arch Surg 2012;397:29-35. [ Links ]
3. Costantini M, Zaninotto G, Rizzetto, et al. Oesophageal diverticula. Best Pract Res Clin Gastroenterol 2004;18:3-17. [ Links ]
4. Vicentine F, Herbella F, Silva L, et al. High resolution manometry findings in patients with esophageal epiphrenic diverticula. Am Surg 2011;77:1661-4. [ Links ]
5. Schima W, Schober E, Stacher G, et al. Association of midoesophageal diverticula with oesophageal motor disorders. Acta Radiol 1997;38:108-14. [ Links ]
6. Khan N, Ismail F, van der Werke I. Oesophageal pouches and diverticula: A pictorial review. S Afr J Surg 2012;50:71-5. [ Links ]
7. Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24(Supl. 1):57-65. [ Links ]
8. Benacci JC, Deschamps C, Trastek VF, et al. Epiphrenic diverticulum: Results of surgical treatment. Ann Thorac Surg 1993;55:1109-14. [ Links ]
9. Palotas A, Lazar G, Paszt A, et al. Alkali ingestion predisposes to developing giant mid-esophageal pulsion diverticulum - A report of a medical rarity. Med Hypotheses 2004;62:931-4. [ Links ]
10. Herbella F, Dubecz A, Patti MG. Esophageal diverticula and cancer. Dis Esophagus 2012;25:153-8. [ Links ]
11. Cassivi S, Deschamps C, Nichols FC 3rd, et al. Diverticula of the esophagus. Surg Clin North Am 2005;85:495-503. [ Links ]
12. Ciriza de los Ríos C, Canga F, Castel de Lucas I, et al. How useful is esophageal high resolution manometry in diagnosing gastroesophageal junction disruption: Causes affecting this disruption and its relationship with manometric alterations and gastroesophageal reflux. Rev Esp Enferm Dig 2014;106:22-9. [ Links ]
13. Ciriza de los Ríos C, Canga F. Manometría de alta resolución e impedancia/manometría-pH: Nuevas técnicas para el avance en el conocimiento de la función esofágica y su aplicación clínica. Rev Esp Enferm Dig 2009;101:861-9. [ Links ]
![]() Correspondence:
Correspondence:
Constanza Ciriza-de-los-Ríos.
Department of Gastroenterology.
Hospital Universitario 12 de Octubre.
Avenida de Córdoba, s/n.
28041 Madrid, Spain
e-mail:
constanzacarpa@gmail.com
Received: 03-09-2014
Accepted: 29-09-2014











 text in
text in