My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 n.7 Madrid Jul. 2015
REVIEW
Submucosal chromoendoscopy. A technique that highlights epithelia and differentiates histological components, and renders colon polypectomy easier and safer
Cromoendoscopia submucosa. Una técnica que remarca los epitelios, diferencia los componentes histológicos, y facilita y ofrece seguridad a la polipectomía de colon
Carlos Dolz-Abadía and Angels Vilella-Martorell
Department of Digestive Diseases. Hospital Son Llatzer. Palma de Mallorca. Spain
ABSTRACT
Submucosal chromoendoscopy involves the injection of a solution containing a vital stain, usually indigo carmine, into the intestinal wall submucosal layer. This allows to: Better delimit and characterize the various epithelia present (colonic mucosa, adenoma, hyperplastic polyp, serrated polyp, small bowel mucosa); expose and delimit lesion implantation areas; cooperate in the lifting of resectable lesions; ensure section across the submucosal plane; identify intestinal wall structures; render complex polypectomy feasible; and facilitate the identification of perforations.
The present paper offers information on the endoscopic technique for submucosal injection, solution preparation and concentration, and on the potential benefits it may provide for polypectomy or endocopic mucosal resection whether en block or piecemeal. This endoscopic technique simultaneously combines a diagnostic and a therapeutic aspect, since lesion lifting in association with better delimited contours may improve not only accuracy but also endoscopic resection safety and feasibility.
Key words: Chromoendoscopy. Colonic polypectomy.
RESUMEN
La cromoendoscopia submucosa consiste en la inyección de una solución que contiene un colorante vital, por lo general índigo carmín, en la capa submucosa de la pared del intestino. Con ello se consigue: delimitar y caracterizar mejor los diferentes epitelios (mucosa de colon, adenoma, pólipo hiperplásico, pólipo serrado o la mucosa del intestino delgado), exponer y delimitar la base de implantación de las lesiones, colaborar en la sobreelevación de una lesión extirpable, asegurar la sección por el plano submucoso, identificar las estructuras constituyentes de la pared intestinal, hacer factible una polipectomía compleja o facilitar la detección de una perforación.
Este artículo ofrece información sobre la técnica endoscópica de la inyección submucosa, la composición de la solución, su concentración y las ventajas que puede ofrecer para realizar una polipectomía o una resección endoscópica mucosa en bloque o en fragmentos. Esta técnica endoscópica combina de forma simultánea una vertiente diagnóstica y otra terapéutica, pues la sobreelevación de la lesión, junto con la mejorar caracterización de los contornos de la misma, puede mejorar su definición y delimitación además de incrementar la seguridad y la viabilidad de la resección endoscópica.
Palabras clave: Cromoendoscopia. Polipectomía de colon.
Introduction
Chromoendoscopy or chromoscopy is defined as the topical application of dyes during endoscopy in order to highlight tissue characteristics (1). The dyes used for digestive chromoendoscopy are categorized according to their absorption. The first group includes absorbable dyes such as methylene blue, lugol, toluidine blue, and crystal violet. Dyes in the second group are not absorbed, and include indigo carmine. Finally, dyes in the third group modify their color according to pH, as is the case with congo red and phenol red (2).
Indigo carmine is the most widely used stain for colorectal endoscopy. It occurs naturally in the sap of the shrub Indigofera tinctoria, but is currently manufactured synthetically. It may be used as a food coloring in sweets (for instance, in violet-colored candy), drinks, and ice cream. It also serves as pH indicator.
The classical technique for topical chromoendoscopy involves the instillation of indigo carmine over the colonic epithelium and lesions. This requires an optimal or at least adequate level of cleanliness. Some authors previously administer a mucolytic agent (N-acetylcysteine) to cleanse as thoroughly as possible the target area. Atropine, butylhyoscine bromide or glucagon may be administered to obtain a hypokinetic bowel (3).
Then the dye is injected through a spray catheter at a concentration ranging from 0.1% to 0.8%. Once injected, the dye may be washed out with water or air through the same spray catheter should the stain be too dark (2). Mucosal irregularities and pit patterns are then carefully examined, usually with Kudo's pit pattern (4,5) (Fig. 1) and Sanos's capillary pattern (Fig. 2) classifications (6,7). In non-controlled studies aimed at identifying colonic preneoplastic lesions, indigo carmine increased detection rates for flat and smaller lesions overlooked by conventional colonoscopy (8-11). Randomized controlled studies comparing conventional white-light colonoscopy and chromoendoscopy have shown strong evidence that the latter enhances premalignant polyp detection in the colon and rectum (12-16). Moreover, the sensitivity of indigo carmine to predict polyp histology (adenomatous vs. hyperplastic) was 82% and 95%, with a specificity of 64% and 95%, respectively.
The injection of indigo carmine into the submucosal layer, or submucosal chromoendoscopy, is a variant of the above classical modality used to verify the submucosal location of the injected solution. The injection of any solution into the submucosal layer results in a bulging that will not develop during injection into the muscular layer. The addition of indigo carmine to the injected solution colors the resulting bulge and confirms its location within the submucosa. This averts perforation risk during polypectomy (17). Both the muscularis propria and the submucosal fibrotic tissue are weakly stained by indigo carmine. The muscularis propria layer is seen as concentric white fibers whereas fibrosis appears as a dense white-yellowish structure (3,18).
Most of the available information on the submucosal injection of indigo carmine involves the study of adenomas, colon cancer, and ulcerative colitis (12-16,19,20). In the last few years the submucosal injection of indigo carmine has been widely used for endoscopic submucosal dissection (21,22). However, overall, the injection of indigo carmine into the submucosa is a non-standard technique, and information available is scarce on the how, when and where of its use.
This manuscript is an attempt to offer information on the way submucosal chromoendoscopy may be carried out, and on the benefits it may provide.
Endoscopic technique
First, the target lesion is identified and cleansed, and secretions are aspirated. A hypokinetic agent is given for excessive intestinal peristaltism. We use glucagon rather than butylhyoscine bromide (Buscapine, Buscopan) as the latter more commonly increases heart rate.
Once the lesion's surface is attentively examined its attachment is delimited and established. Pedicled lesion resection usually entails no difficulties, but sessile or flat lesions may be challenging or even impossible to excise. In such cases delimiting the lesion's attachment extent and contour is crucial. It is here that submucosal chromoendoscopy may be of invaluable help, as it will lift and more clearly delineate the lesion's base by highlighting its contours. This is feasible even for lesions spanning two aspects of a haustrum or fold. In other words, it may render feasible a lesion initially deemed impossible to resect.
Injected solution composition
No recommendations are available regarding the components of solutions for submucosal chromoendoscopy and their concentrations. There is only some consensus in the endoscopic submucosal dissection setting, but modifications according to authors are many (23-28).
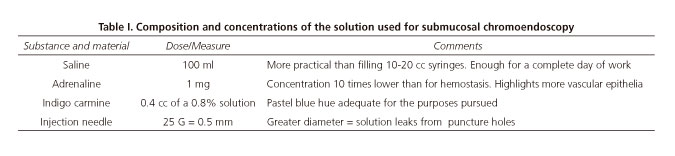
In this paper we shall not refer to the solution used for endoscopic submucosal dissection. Instead, we shall refer to the solution used for classical polypectomy, endoscopic mucosal resection or fragmented resection -anyway, a resection that will not in theory take longer than 15-20 minutes. The composition we recommend in table I is the result of a number of combinations tried in our practice, the one we finally deemed more appropriate.
The liquid base we shall use is a saline solution (0.9% sodium chloride) in a 100-cc container. Reloading from a 100-cc bag-container is more efficient and convenient as compared to filling 10-cc syringes. We add adrenaline, 1 mg per 100 cc of saline. This concentration is 10 times lower than usual when attempting to achieve hemostasis for active bleeding. We must underscore two reasons for the addition of adrenaline to a submucosal chromoendoscopy solution: First, to prevent potential bleeding; second, to obtain vasoconstriction in highly vascular epithelia, as is the case with some adenomas. We have seen that adenomas become paler following this sort of injection, and that such decoloration helps indigo carmine in delimiting the various epithelia present. We deem a higher adrenaline concentration unnecessary, but could be used to manage potential bleeding following resection.
Indigo carmine is available at several concentrations ranging from 0.1% to 0.8%. Its dosing at such concentrations, with no dilution, provides a deep blue color that precludes differentiating the various components of intestinal wall layers. When injecting a dye into the wall our goal is obtaining information on the various components we may come across in order to make better decisions. We must find a blue hue allowing differentiation between collagen fibrous tissue and muscle tissue, veins and arteries, fat from submucosa, etc. Having obtained a number of dilutions we believe that adding 0.4 cc of 0.8% indigo carmine to 100 cc of saline results in an appropriate blue hue for our purposes (Table I). Other compositions and combinations have also been used, as the one suggested by Bourke -succinate-polymerized gelatin plus indigo carmine 80 mg in 500 ml of solution plus adrenaline 1:10.000 (1 ml per 10 ml injected) (28).
Perilesional injection
The method and sequence of the injection procedure are very important. The final result of a consensus on the technique, with the different authors using differing methods. However, the recommendations issued by Bourke are highly useful (28) and may be considered a reference. A first option would consist of starting the injection at the lesion's posterior aspect so that the bulging obtained brings the lesion toward us, from back to front. Once the posterior aspect is lifted, the bulging should be induced on both sides, left and right, in a symmetrical, matching way. Finally, we must examine the lesion on its anterior aspect. Injection at this level may also be required, but always in smaller volumes as compared to the posterior and lateral procedures; failure to comply with this would mar the previously obtained visual plane. This is common in narrower colonic segments such as the sigmoid colon.
It should be noted the perilesional mucosal bulging detracts from endoscopic view, hence it is recommended that the needle be slowly withdrawn into the endoscope's working channel as the bulging develops (Fig. 3-6).



The needle recommended for injection should have a rather small bore to prevent the injected solution from leaking towards the intestinal lumen. A 25 G (0.5 mm) size seems appropriate to us.
The volume to be injected oscillates according to lesion dimensions. A sessile lesion about 25 mm in diameter may admit 5-20 cc of solution. More is better than less since the bulging slowly but steadily flattens over time; however, the injected volume is not to block the visual field thus precluding adequate lesion delimitation.
Some drops of injected solution usually leak from puncture orifices. This should entail no difficulties -rather, superficial epithelial staining helps define their characteristics and better delineate lesion borders.
Lesion resection
After submucosal injection completion we shall have a clearer view of the lesion's attachment base, which will allow an estimation of the lesion's histological nature and invasion depth by using the Kudo and Sano classifications (4,5,7). With this we are in a better position to decide whether the lesion should be excised and the best therapeutic modality to be used (Figs. 1 and 2). Be as it may, the final objective should be visual reassurance that a complete resection, that is, an R0 resection was obtained of the neoformed tissue. Factors in favor of submucosal injection (submucosal chromoendoscopy) include better lesion exposure from the lifting action exerted with a potential disappearance of the haustra effect, and complete exposure of difficult-to-identify neoplastic tissue as occurs with some serrated polyps. Some of these serrated polyps, the so-called SSA/P-D (sessile serrated adenomas/polyps) growths, have a non-dysplastic component that may be easily overlooked, thus resulting in incomplete endoscopic resection (29-33).
Better lesion exposure permits a safer, more accurate endoscopic resection. Similarly, lesion lifting averts perforation risk by increasing intestinal wall thickness, and may minimize bleeding risk as a result of the vasoconstriction provided by the diluted adrenaline associated with indigo carmine.
Often, a lesion initially considered non-resectable becomes endoscopically resectable in just one fragment, which allows the pathology study of a single block and ensures a precise histological characterization. A second option is fragmented (piecemeal) resection following submucosal injection. Piecemeal resection entails uncertain pathological diagnosis and uncertain cure, hence must be considered a valid though not preferable option. With good visual access, a resection en block should have margins < 25-30 mm in the distal colon and rectum, and < 20-25 mm in the right colon (28).
Once resection is completed, the bluish tinge of the submucosa grants that it took place along that plane, and lower perforation risks. The sight of linear, parallel, whitish structures will suggest the muscle layer was reached, and depth was excessive. Small ectopic fat collections may be identified in the submucosa, particularly in the proximal colon, which should not be mistaken for peritoneal fat; the latter would suggest perforation. Red areas may also be identified that represent submucosal bleeding and should not be mistaken for muscle fibers, which are a whitish pale color (18). Prior staining with India ink, as in a tattoo, may confer a typical blackish hue to the submucosal layer, and result in wall fibrosis and loss of elasticity, which translates into higher perforation risk after endoscopic resection; from all the above, endoscopic resection should be avoided on previously tattooed segments if possible (34,35). The use of prophylactic endoscopic procedures to avoid digestive bleeding after the endoscopic resection of large colonic lesions (including the use of clips to bring together the borders of the mucosal defect left after the excision) is now open to debate (36). Closing the resection base may reduce bleeding risk (37). Thus, the prophylactic use of clips may reduce the risk for complications following polypectomy for lesions greater than 2 cm in size, although controlled, randomized studies are needed to demonstrate this in a prospective manner. Reinjecting the indigo carmine solution is also useful when in doubt regarding potential microperforations. Reinjection may confirm an appropriate resection plane, thus reducing the risk for delayed perforation (17).
In summary, submucosal chromoendoscopy may attain several goals:
- Better delimitation and characterization of the different epithelia present, thus telling the normal colonic mucosa from that of lesions.
- Exposure and definition of a lesion's attachment base and its morphology (this may render feasible the resection of a lesion previously considered non-resectable).
- Confirmation that resection took place along the submucosal layer.
- Improved perforation detection.
References
1. Devuni D, Vaziri H, Anderson JC. Chromocolonoscopy. Gastroenterol Clin North Am 2013;42:521-45. DOI: 10.1016/j.gtc.2013.05.002. [ Links ]
2. Wong KeeSong LM, Adler DG, Chand B, et al. Chromoendoscopy. ASGE Technology Committee. Gastrointest Endosc 2007;66:639-49. [ Links ]
3. Mönkemüller K, Wilcox CM. Interventional chromoendoscopy. Gastrointest Endosc 2013;78:346-50. DOI: 10.1016/j.gie.2013.04.181. [ Links ]
4. Kudo S, Hirota S, Nakajima T, et al. Colorectal tumours and pit pattern. J Clin Pathol 1994;47:880-5. DOI: 10.1136/jcp.47.10.880. [ Links ]
5. Kudo S, Tamura S, Nakajima T, et al. Diagnosis of colorrectal tumourous lesions by magnifying endoscopy. Gastrointest Enodsc 1996;44:8-14. DOI: 10.1016/S0016-5107(96)70222-5. [ Links ]
6. Fu KL, Sano Y, Kato S, et al. Chromoendoscopy using indigo carmine dye sparring with magnifying observation is the most reliable method for differential diagnosis between non-neoplastic and neoplastic colorrectal lesions: A prospective study. Endoscopy 2004;36:1089-93. DOI: 10.1055/s-2004-826039. [ Links ]
7. Uraoka T, Saito Y, Ikematsu H, et al. Sano's capillary pattern classification for narrow-band imaging of early colorectal lesions. Dig Endosc 2011;23(Supl. 1):112-5. DOI: 10.1111/j.1443-1661.2011.01118.x. [ Links ]
8. Hurlstone DP, Sanders DS, Cross SS, et al. Colonoscopic resection of lateral spreading tumours: A prospective analysis of endoscopic mucosal resect. Gut 2004;53:1334-9. DOI: 10.1136/gut.2003.036913. [ Links ]
9. Rembacken BJ, Fujii T, Cairns A, et al. Flat and depressed colonic neoplasms: A prospective study of 1000 colonoscopies in the UK. Lancet 2000;355:1211-4. DOI: 10.1016/S0140-6736(00)02086-9. [ Links ]
10. Lee JH, Kim JW, Cho YK, et al. Detection of colorectal adenomas by routine chromoendoscopy with indigo carmine. Am J Gastroenterol 2003;98:1284-8. DOI: 10.1111/j.1572-0241.2003.07473.x. [ Links ]
11. Brown SR. Baraza W. Chromoscopy versus convetional endoscopy for the detection of polyps in the colon and rectum. Cochrane Database Syst Rev 2010;(10):CD006439. [ Links ]
12. Brooker JC, Saunders BP, Shah SG, et al. Total colonic dye-spray increases the detection of diminutive adenomas during routine colonoscopy: A randomized controlled trial. Gastrointest Endosc 2002;56:333-8. DOI: 10.1016/S0016-5107(02)70034-5. [ Links ]
13. Hurlstone DP, Cross SS, Slater R, et al. Detecting diminutive colorectal lesions at colonoscopy: A randomised controlled trial of pan-colonic versus targeted chromoscopy. Gut 2004;53:376-80. DOI: 10.1136/gut.2003.029868. [ Links ]
14. Lapalus MG, Helbert T, Napoleon B, et al. Does chromoendoscopy with structure enhance the colonoscopic adenoma detection rate? Endoscopy 2006;38:444-8. [ Links ]
15. Le Rhun M, Coron E, Parlier D, et al. High resolution colonoscopy with chromoscopy versus standard colonoscopy for the detection of colonic neoplasia: A randomized study. Clin Gastroenterol Hepatol 2006;4:349-54. DOI: 10.1016/j.cgh.2005.12.009. [ Links ]
16. Stoffel EM, Turgeon DK, Stockwell DH, et al. Great Lakes New England Clinical Epidemiology and Validation Center of the Early Detection Research Network. Chromoendoscopy detects more adenomas than colonoscopy using intensive inspection without dye spraying. Cancer Prev Res (Phila) 2008;7:507-13. DOI: 10.1158/1940-6207.CAPR-08-0096. [ Links ]
17. Holt BA, Jayasekeran V, Sonson R, et al. Topical submucosal chromoendoscopy defines the level of resection in colonic EMR and may improve procedural safety (with video). Gastrointest Endosc 2013;77:949-53. DOI: 10.1016/j.gie.2013.01.021. [ Links ]
18. Tutticci N, Bourke MJ. Interventional chromoendoscopy: Specific aspects for the colon. Gastrointest Endosc 2014;79:536-8. DOI: 10.1016/j.gie.2013.09.002. [ Links ]
19. Matsumoto T, Iwao Y, Igarashi M, et al. Endoscopic and chromoendoscopic atlas featuring dysplastic lesions in surveillance colonoscopy for patients with long-standing ulcerative colitis. Inflamm Bowel Dis 2008;14:259-64. DOI: 10.1002/ibd.20267. [ Links ]
20. Kiesslich R, Neurath MF. Chromoendoscopy in inflammatory bowel disease. Gastroenterol Clin North Am 2012;41:291-302. DOI: 10.1016/j.gtc.2012.01.016. [ Links ]
21. Herreros de Tejada A. ESD training: A challenging path to excellence. World J Gastrointest Endosc 2014;6:112-20. DOI: 10.4253/wjge.v6.i4.112. [ Links ]
22. Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video). Gastrointest Endosc 2010;72:1217-25. DOI: 10.1016/j.gie.2010.08.004. [ Links ]
23. Conio M, Rajan E, Sorbi D, et al. Comparative performance in the porcine esophagus of different solutions used for submucosal injection. Gastrointest Endosc 2002;56:513-6. DOI: 10.1016/S0016-5107(02)70435-5. [ Links ]
24. Hyun JJ, Chun HR, Chun HJ, et al. Comparison of the characteristics of submucosal injection solutions used in endoscopic mucosal resection. Scand J Gastroenterol 2006;41:488-92. DOI: 10.1080/00365520500325994. [ Links ]
25. Kantsevoy SV, Adler DG, Conway JD, et al. Endoscopic mucosal resection and endoscopic submucosal dissection. ASGE Technology Committee. Gastrointest Endosc 2008;68:11-8 DOI: 10.1016/j.gie.2008.01.037. [ Links ]
26. Matsui Y, Inomata M, Izumi K, et al. Hyaluronic acid stimulates tumor-cell proliferation at wound sites. Gastrointest Endosc 2004;60:539-43. DOI: 10.1016/S0016-5107(04)01890-5. [ Links ]
27. Bures J, Kopácová M, Kvetina J, et al. Different solutions used for submucosal injection influence lyhealing of gastric endoscopic mucosal resection in a preclinical study in experimental pigs. SurgEndosc 2009;23:2094-101. [ Links ]
28. Bourke MJ. Endoscopic mucosal resection in the colon: A practical guide. Tech Gastroientest Endosc 2011;13:35-49. DOI: 10.1016/j.tgie.2011.01.002. [ Links ]
29. Pohl H, Srivastava A, Bensen SP, et al. Incomplete polyp resection during colonoscopy-results of the complete adenoma resection (CARE) study. Gastroenterology 2013;144:74-80 DOI: 10.1053/j.gastro.2012.09.043. [ Links ]
30. Gancayco J, Siddiqui UD, Jain D, et al. Narrow band imaging features and pathological correlations of sessile serrated polyps. Am J Gastroenterol 2011;106:1559-60 DOI: 10.1038/ajg.2011.122. [ Links ]
31. Tadepalli US, Feihel D, Miller KM, et al. A morphologic analysis of sessile serrated polyps observed during routine colonoscopy. Gastrointest Endosc 2011;74:1360-8. DOI: 10.1016/j.gie.2011.08.008. [ Links ]
32. Hazewinkel Y, López-Cerón M, East JE, et al. Endoscopic features of sessile serrated adenomas: Validation by international experts using high-resolution white-light endoscopy and narrow-band imaging. Gastrointest Endosc 2013;77:916-24. DOI: 10.1016/j.gie.2012.12.018. [ Links ]
33. Burgess NG, Tutticci NJ, Pellise M, et al. Sessile serrated adenomas/polyps with cytologic dysplasia: A triple threat for interval cancer. Gastrointest Endosc 2014;80:307-10. DOI: 10.1016/j.gie.2014.03.050. [ Links ]
34. Trakarnsanga A, Akaraviputh T. Endoscopic tattooing of colorectal lesions: Is it a risk-free procedure? World J Gastrointest Endosc 2011;3:256-60. [ Links ]
35. Moss A, Bourke MJ, Pathmanathan N. Safety of colonic tattoo with sterile carbon particle suspension: A proposed guideline with illustrative cases. Gastrointest Endosc 2011;74:214-8. DOI: 10.1016/j.gie.2011.01.056. [ Links ]
36. Bourke MJ. Bleeding following wide-field endoscopic resection in the colon. Gastroenterol Hepatol 2011;7:814-7. [ Links ]
37. Liaquat H, Rohn E, Rex DK. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: Experience in 277 clip large sessile or flat colorectal lesions and 247 control lesions. Gastrointest Endosc 2013;77:401-7. DOI: 10.1016/j.gie.2012.10.024. [ Links ]
![]() Correspondence:
Correspondence:
Carlos Dolz Abadía.
Department of Digestive Diseases.
Hospital Son Llatzer.
Ctra. Manacor, km. 4.
07198 Palma de Mallorca
e-mail: cdolzaba@gmail.com
Received: 25-09-2014
Accepted: 07-01-2015











 text in
text in