Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.9 Madrid sep. 2015
The management of lactose intolerance among primary care physicians and its correlation with management by gastroenterologists: The SEPD-SEMG national survey
Manejo de la intolerancia a la lactosa entre los médicos de atención primaria y su correlación con la de los especialistas en digestivo: encuesta nacional SEPD-SEMG
Federico Argüelles-Arias1, Pilar Rodríguez-Ledo2, José María Tenías3, Mercedes Otero4, Francesc Casellas5, Guadalupe Blay-Cortés6, Alfredo Lucendo7, José Luis Domínguez-Jiménez8 and Fernando Carballo9
1Hospital Universitario Virgen Macarena. Sevilla, Spain.
2Gerencia de Gestión Integrada de Lugo, Cervo e Monforte. Lugo, Spain.
3Unidad Docente de Atención Familiar y Comunitaria. EVES, Valencia. Spain.
4Emergency Department. Clínica Marazuela. Talavera de la Reina, Toledo. Spain.
5Hospital Vall d'Hebron. Barcelona, Spain.
6Nutrition Unit. Policlínica Sagasta. Zaragoza, Spain.
7Hospital General de Tomelloso. Ciudad Real, Spain.
8Hospital Alto Guadalquivir de Andújar. Jaén, Spain.
9Hospital Clínico Universitario Virgen de la Arrixaca. IMIB. Murcia, Spain.
ABSTRACT
Introduction and aims: The understanding of lactose intolerance (LI) is limited in some professional settings. Sociedad Española de Patología Digestiva (SEPD) and Sociedad Española de Medicina General (SEMG) have developed a survey in order to: a) Analyze primary care physicians (PCPs) knowledge and clinical management; and b) to compare results with those of a previous survey of Spanish gastroenterologists (GEs).
Material and methods: An online questionnaire was sent to SEMG members with 27 items on various issues: Demographics, occupational characteristics, outlook on LI, diagnostic tests, treatment, and follow-up. Results were compared to those from a survey of GEs.
Results: A total of 456 PCPs responded, versus 477 GEs. PCPs had an older mean age and longer professional experience. Level of understanding of LI was similar, albeit a higher proportion of PCPs lacked epidemiological awareness (p < 0.01). GEs tended to consider LI a "minor" condition (71.3 vs. 40.1%; p > 0.001), and LI symptoms as overlapping those of irritable bowel syndrome (93.5 vs. 88.2%; p = 0.005), although symptoms perceived as suspicious of LI were similar in both groups. Dietary recommendations were recognized as the primary therapeutic approach.
Conclusion: This study reveals the outlook of PCPs on LI, and allows comparison with that of GEs, as a basis for the development of strategies aimed at improving LI understanding, approach and management in our setting.
Key words: Lactose intolerance. SEPD. Family doctors. Primary care physicians. Survey. Lactose intolerance management. Hypolactasia.
RESUMEN
Introducción y objetivos: el conocimiento sobre la intolerancia a la lactosa (IL) es limitado en algunos ámbitos profesionales. La Sociedad Española de Patología Digestiva (SEPD) y la Sociedad Española de Medicina General (SEMG) han elaborado una encuesta con los objetivos de: a) analizar el nivel de conocimiento y de manejo clínico de los médicos de atención primaria (MAP); y b) comparar sus resultados con los de la encuesta ya realizada entre los gastroenterólogos españoles (GE).
Material y métodos: se envió un cuestionario online a los socios de la SEMG, con 27 preguntas sobre distintas cuestiones: demografía y características laborales, actitud frente a la IL, métodos de diagnóstico, tratamiento y seguimiento. Los resultados fueron comparados con los de la encuesta a GE.
Resultados: se recopilaron 456 respuestas de MAP, que se compararon con las proporcionadas por 477 GE. Los MAP presentaron una edad media y experiencia profesional mayor. El nivel de conocimiento sobre IL fue parecido, si bien una mayor proporción de MAP desconocía la epidemiología del problema (p < 0,01). Los GE tendieron a considerar a la IL una patología "menor" (71,3 vs. 40,1%; p > 0,001), y a sus síntomas superponibles a los del síndrome del intestino irritable (93,5 vs. 88,2%; p = 0,005), si bien los síntomas reconocidos como sospechosos de IL fueron similares entre ambos grupos. Las recomendaciones dietéticas fueron reconocidas como la principal medida terapéutica.
Conclusión: este estudio permite conocer la actuación de los MAP ante la IL y compararla con la de los GE, como base para el desarrollo estrategias para mejorar el conocimiento, actitud y tratamiento de la IL en nuestro medio.
Palabras clave: Intolerancia a lactosa. SEPD. Médicos de familia. Médicos de atención primaria. Encuesta. Manejo de la intolerancia a lactosa. Hipolactasia.
Introduction
Lactase is a surface disaccharidase present at the apical brush border of enterocytes in small bowel microvilli. It is mainly found in the proximal jejunum. This enzyme's deficiency is known as hypolactasia, and may often entail lactose malabsorption and gastrointestinal symptoms, which is known as lactose intolerance (LI).
Lactase activity may be detected as early as on the 8th week of pregnancy at the intestinal mucosal surface, and increases through week 34, with peak expression being reached at birth. In mammals it declines after weaning as a result of dysregulated gene expression (1). The rate of lactase activity loss varies according to ethnicity, and Asians lose 80-90% of lactase activity within 3-4 years after weaning whereas North Europeans exhibit trough expression at 18-20 years. Data have been recently reported on its prevalence in South America (2). In our country no recent prevalence data are available as most studies date back to the 1970s (3). In the study performed in Galicia (4) a prevalence of 32.5% was found among the pediatric population. At the opposite age end the study by Varela-Moreiras et al. (5) found a prevalence of 36%, with 51% being found in the study by Casellas et al. (6).
Despite this high prevalence, the societal demand for more information and on the health impact of LI (for instance, its potential association with osteoporosis) has been long overlooked by gastroenterologists, who consider it a benign, "easily" managed condition. However, gastroenterologists are increasingly interested in its etiopathogenesis, management, impact and treatment. Similarly, primary care physicians (PCPs) demand information on this condition, and a recent study concludes that concepts and terms require clarification among PCPs (7). Indeed, while some guidelines exist on its diagnosis and management (8,9) many aspects remain unclear, and the condition's approach by specialists and PCPs is often inadequate.
From all the above, following a survey of gastroenterologists affiliated with Sociedad Española de Patología Digestiva (SEPD) (10), both SEPD and Sociedad Española de Medicina General (SEMG) set up a task force to develop a new survey based on the above now intended for family doctors. Changes to the previous survey were proposed by the authors based on PCP professional characteristics.
The goals of this study include:
- Discussing the understanding, diagnosis, attitudes, and management regarding this condition by primary care physicians.
- Comparing these results with those of the survey of Spanish gastroenterologists (GEs).
Material and methods
An online survey was administered to SEMG members. SEPD and SEMG members developed a 27-item survey based on the previous survey of SEPD members covering domains such as epidemiology, work post characteristics, attitude regarding the condition, diagnosis, treatment, and follow-up. Modifications were introduced according to the target specialty but keeping most items unchanged to allow comparison.
Statistical study
A descriptive analysis of responses was undertaken, followed by a comparative study using the chi-squared test (Fisher's exact test for values below 5 in the answers from both groups), considering statistical significance at 0.05. An analysis adjusted for age, sex, and professional experience was also carried out to establish differences in variables and their trends according to said subgroups between both surveyed groups. The IBM SPss Statistics 22.0 package was used for calculations.
Results
A total of 456 PCPs responded and were compared to 477 gastroenterologists (GEs). The proportion of female respondents was 41.5% among GEs and 59% among PCPs, with a median age of 52 (IQR 43 to 56 years) and 45 (IQR 35 to 57 years), respectively (Table I), with differences being statistically significant for both parameters (p < 0.001 in both cases). As regards work post, most GEs worked at third-level, mid-sized (200-500 beds), university hospitals, had MIR training in gastroenterology, and their cumulative experience within the specialty was at least 10 years. As for PCPs, 87.3% worked at an outpatient clinic, urban in 63.9% of cases, 75% had more than 1,200 individual health cards (IHCs) assigned, with a median of 1500 IHCs, and 21.5% were resident tutors. Professional experience amounted to 10 or less years for 41.9% of GEs, whereas 52.2% of PCPs had 21 or more years (Table I), this difference being statistically significant (p < 0.001).
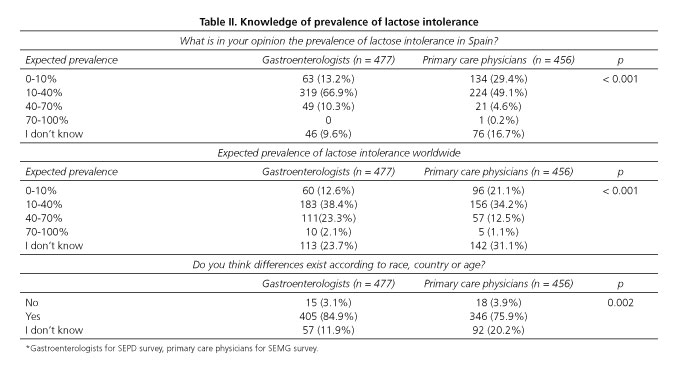
When analyzing knowledge of the prevalence of LI in Spain, results differed between these two groups, with statistically significant differences (p < 0.001) in the numbers of unaware respondents. A similar situation was found regarding LI prevalence worldwide, only with greater ignorance (p < 0.001). For differences according to race, age, and country, PCPs had a greater lack of awareness (p = 0.002) (Table II).
Regarding outlook on LI, GEs tend to consider it more commonly (71.3 vs. 40.1%) a minor condition in a statistically significant fashion (p < 0.001), with symptoms overlapping those of irritable bowel syndrome or functional dyspepsia (93.5 vs. 88.2%), also in a statistically significant manner (p = 0.005).
The assessment of symptoms indicative of LI is similar between GEs and PCPs except for discomfort after the ingestion of dairy products, considered highly suggestive by PCPs but not by GEs (Table III).
Beliefs on the tolerance of lactose or drugs in smaller amounts were more common among GEs (49.7 vs. 24.3% for lactose; 45.1 vs. 14.9% for drugs), this difference being statistically significant (Table IV).
As regards therapeutic approach dietary recommendations predominated in both groups albeit with a higher proportion among GEs (99.09 vs. 92.3%), as was also the case for the prescription of lactase tablets (57.2 vs. 25.6%), with statistical significance being reached in both instances (p < 0.001 for both). When used, lactase tablets were mostly prescribed on an occasional basis (90.4 vs. 86.5%, slightly higher for GEs). Calcium/vitamin D supplements were a minority recommendation (GEs 28.9%, PCPs 29.6%) with no significant differences between groups.
In both groups concerns regarding food intolerance are mostly based on the natural association between food and symptom onset (62.9% for GEs, 51.5% for PCPs), and most particularly on need for therapy in patients with functional impairment (73.6% for GEs, 73.0% for PCPs), as reflected in Table V. Both groups consider training on these conditions a useful measure (98.7 vs. 96.4%).
When responses were assessed according to age, there was a statistically significant greater trend among older PCPs to consider LI a non-minor condition, to be unaware of etiology, to consider laboratory tests more relevant for diagnosis, to advise against smaller amounts of lactose or lactose-containing drugs, and to prescribe more calcium/vitamin D supplementation. Among gastroenterologists older age was significantly associated with diagnostic testing (p = 0.027), fewer referrals to primary care (p = 0.004), prescription of calcium/vitamin D supplementation (p = 0.005), and advice against lactose-containing drugs (p < 0.001).
Discussion
The present paper discusses the comparative results of two surveys on LI among gastroenterologists and primary care physicians. We consider it a novel approach as no similar studies are found among the literature, and it sheds light on the beliefs and outlooks held by PCPs, allows comparison of specialized versus primary care management, and obtains highly interesting data that will empower both societies to develop joint strategies to promote improved awareness, diagnosis, outlook, and management regarding this intolerance.
Interestingly, these two groups of practitioners are heterogeneous, which represents a study limitation and a potential selection bias; as surveys were emailed to all members in both societies only practitioners interested in this condition may be represented among respondents. Differences were found between both groups that may influence the results obtained - over 50% of responding GEs were 30-50 year-olds and over 50% of PCPs were above 50 years of age. This results in differences in professional experience, longer among PCPs.
Interestingly, over 9% and 23% of GEs and over 16% and 31% of PCPs are unaware of the prevalence of LI in Spain and worldwide, respectively. This is obviously no reflection of the perceived relevance of the condition; however, we do believe that such results should prompt training committees in both societies to develop awareness programs on this subject.
Likewise, most respondents suspect a patient may have LI in the presence of diarrhea and bloating, albeit PCPs pay more attention to the association between dairy product ingestion and symptom onset. While such correlation has been questioned by some studies (11,12), eliciting this aspect during history taking may be helpful for diagnosis both in the primary care and the outpatient gastroenterology setting.
The fact that GEs more commonly tend to consider LI a minor condition in a statistically significant manner is outstanding, and again highlights the traditional low relevance of this disease among GEs, not so among PCPs. The scarce specificity of LI symptoms has been demonstrated in multiple studies (13-16), and the fact that symptoms overlap those of irritable bowel syndrome (17) or functional dyspepsia (93.5 vs. 88.2%) is well known by both groups of practitioners, especially by GEs.
A common question posed by patients with LI is how much lactose they may take and whether their usual drugs may contain lactose and induce symptoms. The results of our survey reveal societal demand that a greater proportion of GEs versus PCPs consider that small amounts of lactose, including lactose-containing drugs, may be tolerated bymost patients. This has been presumably demonstratedby some studies (18) but evidence is inadequate, as some variables should be considered - e.g., the number of lactose-containing drugs actually taken. From our viewpoint this is aspect deserves careful assessment as information is sparse on the drugs that contain this sugar, and many of those prescribed by GEs actually have lactose among excipients (19).
The last part of the survey focuses on treatment and dietary recommendations for intolerant patients. Differences are seen between both groups on this aspect, with a greater proportion of GEs recommending lactase supplementation and dietary measures. Notably, the number of practitioners who prescribe calcium and vitamin D supplements is low in both groups, but such recommendation may be obviated given the availability of lactose-free milk containing calcium and vitamin D. However, studies have been reported that associate LI with low vitamin D levels (9,20), albeit with no direct impact on child growth (21).
Also outstanding is the fact that older GEs and PCPs consider LI to be more "severe" when compared to younger physicians. Thus, they advise against low lactose ingestion, including in drugs, and consider diagnostic testing mandatory; as for GEs, most won't refer patients to primary care.
Finally, respondents clearly request more information on this topic and on food intolerance, as patients increasingly demand such information. SEPD and SEMG training committees should take notice thereof and develop joint training programs or specific protocols to improve awareness and patient management. Many aspects remain obscure but improved management will no doubt improve quality of life.
Acknowledgments
We are grateful to all SEMG and SEPD members who responded. Their participation and cooperation is necessary for these studies. Similarly, we are also grateful to SEMG for their active collaboration in the survey, and to SEPD, most particularly to Ángel Martínez, Henar Ortega, Beatriz Sánchez, and Ricardo Burón, for their invaluable help.
References
1. Kretchmer N. Lactose and lactase - a historical perspective. Gastroenterology 1971;61:805-13. [ Links ]
2. Latorre G, Besa P, Parodi CG, et al. Prevalence of lactose intolerance in Chile: A double-blind placebo study. Digestion 2014;90:18-26. DOI: 10.1159/000363229. [ Links ]
3. Guix García J, Rodrigo Gómez JM, Aparisi Quereda L, et al. Lactose intolerance in the Spanish population. Rev Esp Enferm Dig 1974;42:367-82. [ Links ]
4. Leis R, Tojo R, Pavón P, et al. Prevalence of lactose malabsorption in Galicia. J Pediatr Gastroenterol Nutr 1997;25:296-300. DOI: 10.1097/00005176-199709000-00009. [ Links ]
5. Varela-Moreiras G, Antoine JM, Ruiz-Roso B, et al. Effects of yogurt and fermented-then-pasteurized milk on lactose absorption in an institutionalized elderly group. J Am Coll Nutr 1992;11:168-71. [ Links ]
6. Casellas F, Aparici A, Casaus M, et al. Self-perceived lactose intolerance and lactose breath test in elderly. Eur Geriatr Med 2013;4:372-5. DOI: 10.1016/j.eurger.2013.07.004. [ Links ]
7. Jellema P, Schellevis FG, van der Windt DA, et al. Lactose malabsorption and intolerance: A systematic review on the diagnostic value of gastrointestinal symptoms and self-reported milk intolerance. QJM 2010;103:555-72. DOI: 10.1093/qjmed/hcq082. [ Links ]
8. Gasbarrini A, Corazza GR, Gasbarrini G, et al.; 1st Rome H2-Breath Testing Consensus Conference Working Group. Methodology and indications of H2-breath testing in gastrointestinal diseases: the Rome Consensus Conference. Aliment Pharmacol Ther 2009;29(Supl. 1):1-49. [ Links ]
9. Suchy FJ, Brannon PM, Carpenter TO, et al. NIH consensus development conference statement: Lactose intolerance and health. NIH Consens State Sci Statements 2010;27:1-27. [ Links ]
10. Argüelles-Arias F, Tenías JM, Casellas-Jordá F, et al. Results of a nation-wide survey on hypolactasia - How is this condition diagnosed and managed in our setting? Rev Esp Enferm Dig 2015;107:55-6. [ Links ]
11. Gelincik A, Buyukozturk S, Gul H, et al. Confirmed prevalence of food allergy and non-allergic food hypersensitivity in a Mediterranean population. Clin Exp Allergy 2008;38:1333-41. DOI: 10.1111/j.1365-2222.2008.03019.x. [ Links ]
12. Casellas F, Aparici A, Casaus M, et al. Subjective perception of lactose intolerance does not always indicate lactose malabsorption. Clin Gastroenterol Hepatol 2010;8:581-6. DOI: 10.1016/j.cgh.2010.03.027. [ Links ]
13. Dainese R, Casellas F, Mariné-Barjoan E, et al. Perception of lactose intolerance in irritable bowel syndrome patients. Eur J Gastroenterol Hepatol 2014;26:1167-75. DOI: 10.1097/MEG.0000000000000089. [ Links ]
14. Shaw AD, Davies GJ. Lactose intolerance: Problems in diagnosis and treatment. J Clin Gastroenterol 1999;28:208-16. DOI: 10.1097 /00004836-199904000-00005. [ Links ]
15. Fernández-Bañares F. Reliability of symptom analysis during carbohydrate hydrogen-breath tests. Curr Opin Clin Nutr Metab Care 2012;15:494-8 DOI: 10.1097/MCO.0b013e328356689a. [ Links ]
16. Yang J, Fox M, Cong Y, et al. Lactose intolerance in irritable bowel syndrome patients with diarrhoea: The roles ofanxiety, activation of the innate mucosal immune system and visceral sensitivity. Aliment Pharmacol Ther 2014;39:302-11. DOI: 10.1111/apt.12582. [ Links ]
17. Vernia P, Di Camillo M, Marinaro V. Lactose malabsorption, irritable bowel syndrome and self-reported milk intolerance. Dig Liver Dis 2001;33:234-9. DOI: 10.1016/S1590-8658(01)80713-1. [ Links ]
18. Montalto M, Gallo A, Santoro L, et al. Low-dose lactose in drugs neitherincreases breath hydrogen excretion nor causes gastrointestinal symptoms. Aliment Pharmacol Ther 2008;28:1003-12. DOI: 10.1111/j.1365-2036.2008.03815.x. [ Links ]
19. Eadala P, Waud JP, Matthews SB, et al. Quantifying the 'hidden' lactose in drugs used for the treatment ofgastrointestinal conditions. Aliment Pharmacol Ther 2009;29:677-87. DOI: 10.1111/j.1365-2036.2008.03889.x. [ Links ]
20. Tereszkowski CM, Simpson JA, Whiting SJ, et al. Body mass, vitamin D and alcohol intake, lactose intolerance, and television watching influence bonemineral density of young, healthy Canadian women. J Am Coll Nutr 2012;31:24-31. DOI: 10.1080/07315724. 2012.10720005. [ Links ]
21. Lehtimäki T, Hemminki J, Rontu R, et al. The effects of adult-type hypolactasia on body height growth and dietary calcium intake from childhood into young adulthood: A 21-year follow-up study - the Cardiovascular Risk in Young Finns Study. Pediatrics 2006;118:1553-9. DOI: 10.1542/peds.2006-0542. [ Links ]
![]() Correspondence:
Correspondence:
Federico Argüelles-Arias.
Hospital Universitario Virgen Macarena.
Avda. Doctor Fedriani, 3.
41071 Sevilla, Spain
e-mail: farguelles@telefonica.net
Received: 15-03-2015
Accepted: 30-05-2015











 texto en
texto en