My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 n.12 Madrid Dec. 2015
CASE REPORT
Malignant degeneration of rectal endometriosis
Degeneración maligna de endometriosis de recto
José Andrés García-Marín, Enrique Manuel Pellicer-Franco, Victoriano Soria-Aledo, Mónica Mengual-Ballester, Graciela Valero-Navarro and José Luis Aguayo-Albasini
Services of General Surgery and Gastroenterology. Hospital Universitario Morales Meseguer. Murcia, Spain
ABSTRACT
Background: Endometriosis is a relatively common disease among women with child-bearing potential, and rare before puberty or following menopause. It consists of the presence of hormone-responsive endometrium outside the endometrial cavity.
Case report: We report the case of a patient with a rectal lesion, initially approached as a primary rectal malignancy, where histopathology eventually revealed an adenocarcinoma arising from endometrial tissue in the colonic wall.
Discussion: Endometriosis has an estimated rated of 10-20%. Sites may be split up into two larger categories - gonadal and extragonadal. The frequency of extragonadal endometriosis in the bowel is estimated to involve 3%-37% of women with pelvic endometriosis, and most lesions are found in the sigmoid colon and rectum. The malignant transformation of endometriotic lesions is estimated between 0.3% and 1% of cases. The gold standard in the diagnosis of intestinal endometriosis is exploratory laparotomy and the pathological study of specimens. Adjuvant radiotherapy and chemotherapy, although used for some patients, have not proven effective.
Key words: Degeneration. Endometriosis. Rectum.
RESUMEN
Introducción: la endometriosis es una patología relativamente frecuente en mujeres en edad fértil y poco prevalerte en mujeres prepúberes o postmenopáusicas.
Caso clínico: presentamos el caso clínico de una mujer de 57 años, con antecedentes de histerectomía y doble anexectomía por endometriosis ovárica, diagnosticada de neoplasia de recto T3N1. Se realizó neoadyuvancia preoperatoria y resección anterior baja, sin complicaciones. La anatomía patológica describía infiltración de la pared rectal por adenocarcinoma pobremente diferenciado de origen ginecológico.
Discusión: la endometriosis tiene una prevalencia estimada del 10-20% y su lugar de aparición puede ser variado, tanto gonadal como extragonadal. La frecuencia de endometriosis extragonadal de localización intestinal se estima en un 3-37% de mujeres con endometriosis pélvica, y de estas la mayoría se localizan en colon sigmoide y recto. La transformación maligna de un foco de endometriosis se estima entre el 0,3 y el 1%. El gold estándar para el diagnóstico es la resección y estudio histológico. La radioterapia y quimioterapia adyuvante todavía no ha demostrado su clara utilidad.
Palabras clave: Degeneración. Endometriosis. Recto.
Introducción
Endometriosis is a relatively common disease among women with child-bearing potential and rare before puberty or following menopause. It consists of the presence of hormone-responsive endometrium outside the endometrial cavity. Common sites include the ovaries, Fallopian tubes, pouch of Douglas, and cervix; extragonadal sites include the intestine, bladder, lungs, central nervous system, and even the skin (1). While malignant degeneration of an endometriotic site is a rare occurrence, it must be borne in mind particularly for lesions in the ovaries or bowel.
We report the case of a patient with a rectal lesion, initially approached as a primary rectal malignancy, where histopathology eventually revealed an adenocarcinoma arising from endometrial tissue in the colonic wall. Patient history included prior abdominal surgery for an endometriotic ovarian cyst.
Case report
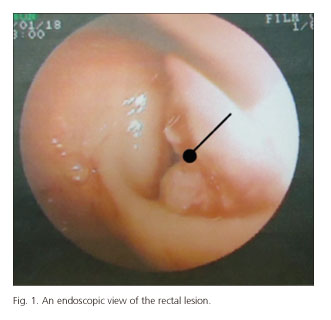
Back in 2003, this 57-year-old woman had undergone hysterectomy with double adnexectomy in a different hospital for pelvic endometriosis and uterine myomatosis; she also had a large 20-cm cyst in the right ovary (which ruptured during surgery), and a 5-cm cyst in the left ovary. In 2008, she visited her doctor because of rectorrhagia for about 8 months with no other associated symptoms. A colonoscopy was performed (Fig. 1), which revealed a stenosing superficially ulcerated neoplasm at 10 cm from the anal margin that blocked the passage of the endoscope. CT colonography confirmed a stenosing rectal neoplasm 4 cm in length with infiltration of perirectal fat and presence of adenopathies. Endoanal ultrasounds staged the lesion as T3N1. There was no evidence of metastatic disease. The pathology report documented a poorly differentiated adenocarcinoma. After consultation with the Oncology department in our hospital, neoadjuvant therapy was given with capecitabine 825 mg/m2/12 hours and pelvic radiation therapy in fractions of 180 cGy/d, 5 doses a week, up to 50.4 Gy. A reassessment reveals a partial response to radiation and a T2-3N0 lesion.
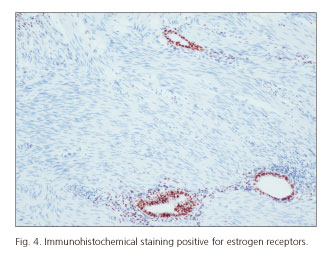
A surgical laparotomy was decided upon, which found a neoplasm in the upper third of the rectum with multiple adhesions and inferior mesenteric adenopathy. A low anterior resection with Quirke grade 2 mesorectal excision was carried out. The postoperative period was complicated by prolonged paralytic ileus and urinary fistula involving the left ureter, which required double J stenting and had a favorable outcome. The specimen pathology report informed rectal wall infiltration by poorly differentiated adenocarcinoma with sclerosis and abundant psammoma bodies (Fig. 2) of extradigestive, likely gynecologic origin. The immunohistochemical profile showed CK20 negativity and CK7 positivity (Fig. 3), as well as mildly positive estrogen receptors (Fig. 4). The patient received adjuvant chemotherapy with taxol-adriamycin-CDDP for 6 cycles. As of today, no clinical or radiographic evidence of recurrence has been found during follow-up.
Discussion
Endometriosis is a condition that usually involves women with child-bearing potential (with an estimated rate of 10% to 20%) (1,2) but data vary because of a high number of either asymptomatic or paucisymptomatic cases. Sites may be split up into two larger categories - gonadal and extragonadal. The former include, in decreasing order of frequency, the ovaries, Fallopian tubes, uterosacral ligaments, pouch of Douglas, rectovaginal septum, cervix, and vagina. Most common extragenital sites include the intestine (particularly the rectum-sigmoid), lungs, bladder, skin, and central nervous system.
The etiology of endometriosis remains obscure and several theories are posited - embryonic theory, Sampson's implantation theory, Halban's vascular or lymphatic dissemination theory, and Meyer's metaplastic theory. The influence of immune factors supporting or favoring some of these theories is currently underscored. Little is known on the extragonadal development of endometrial tissue foci, and both the vascular dissemination and implantation theory might seemingly explain such ectopic implants (3). The frequency of extragonadal endometriosis in the bowel is estimated to involve 3%-37% of women with pelvic endometriosis, and most lesions are found in the sigmoid colon and rectum (4).
Clinically, patients with extragonadal endometriosis have signs and symptoms according to lesion location; if it is the colon that is involved, they may present with rectorrhagia, intestinal obstruction, colicky pain, bowel habit changes, and constitutional syndrome (1,5). The malignant transformation of endometriotic lesions is well covered by the literature (1,6,7). Prevalence is estimated between 0.3% and 1% of cases. Of these, malignancies arising from ovarian endometriosis are most common (up to 75% of cases), followed by those arising from foci in the pelvic peritoneum and the colorectal tract, as in the present case report. Regarding diagnosis, no specific data are known to initially suggest colonic endometriosis. Suspicion may be prompted by a history of genital endometriosis, when present.
Colonoscopy is usually the initial test because of its usefulness to demonstrate extrinsic compression on the colonic mucosa, as well as ulcerations in the instance of advanced disease with mucosal involvement. Biopsy taking is recommended even though no definitive diagnosis is provided for most cases. This is based on Sampson's criteria (8), who in 1925 described the first 7 patients with malignant degeneration of endometriosis, both gonadal and extragonadal, as well as three basic criteria for its diagnosis: a) Presence of both benign and malignant endometrial tissue in the specimen; b) no evidence of other malignancies; and c) malignant endometrial tissue among normal intestinal glands. In our case, the endoscopic view was identical to that of a primary rectal lesion as the mucosa was ulcerated. Furthermore, the tumor's poorly differentiated nature contributed to biopsy results not suggesting a gynecologic origin. In other reported cases (9) endoscopic biopsy taking is cost-ineffective for this type of lesion, as was the case with our patient. The limited amount of tissue that can be obtained may include no endometrial tissue, and both reactive inflammatory changes and the possibility of endometriosis sparing the mucosa may result in false negative findings.
Other tests to be performed in the setting of a neoplastic-looking lesion in the colonic wall include CT scans, CT colonography (when the endoscope cannot pass through), and MRI, as well as endoanal ultrasounds for rectal examination. All are useful to characterize the mass and its extension, but none will provide a definitive diagnosis. The gold standard in the diagnosis of intestinal endometriosis is exploratory laparotomy (1,3) and the pathological study of specimens.
The key test for surgical specimens is immunohistochemical staining for cytokeratin-7 and cytokeratin-20, and for estrogen receptors (1,10-12). Tumor tissue arising from the intestinal mucosa exhibits the following immunoreactivity profile: negative CK7, positive CK20, and negative estrogen receptors. In contrast, endometrial tissue displays, as in our patient: positive CK7, negative CK20, and positive estrogen receptors.
As regards add-on therapy, adjuvant radiotherapy and chemotherapy, although used for some patients, have not proven effective. In our case, after neoadjuvant chemotherapy, a partial response was radiographically demonstrated, with the lesion regressing from a T3N1 stage to T2-3N0, hence it may be claimed to have proven effective for our patient as has been the case in other reports.
Colorectal cancer is a most common malignancy. While most malignant-looking lesions in the colon are primary colonic adenocarcinomas, a different origin may be suspected from the patient history on some occasions. This may at times result in a change of therapy or surgical approach.
References
1. Kobayashi S, Sasaki M, Goto T, et al. Endometrioid adenocarcinoma arising from endometriosis of the rectosigmoid. Dig Endos 2010;22:59-63. [ Links ]
2. Dimoulios P, Koutroubakis IE, Tzardi M, et al. A case of sigmoid endometriosis difficult to differentiate from colon cancer. BMC Gastroenterol 2003;3:18. [ Links ]
3. Kim JS, Hur H, Min BS, et al. Intestinal endometriosis mimicking carcinoma of rectum and sigmoid colon: a report of five cases. Yonsei Med J 2009;50:732-5. [ Links ]
4. Samet JD, Horton KM, Fishman EK, et al. Colonic endometriosis mimicking colon cancer on a virtual colonoscopy study: A potential pitfall in diagnosis. Case Rep Med 2009;2009:379578. [ Links ]
5. Petersen VC, Underwood JCE, Wells M, et al. Primary endometrioid adenocarcinoma of the large intestine arising in colorectal endometriosis. Histopathology 2002;40:171-6. [ Links ]
6. Marchena-Gomez J, Conde-Martel A, Hemmersbach-Miller M, et al. Metachronic malignant transformation of small bowel and rectal endometriosis in the same patient. World J Surg Oncol 2006;4:93. [ Links ]
7. Debus G, Schuhmacher I. Endometrial adenocarcinoma arising during estrogenic treatment 17 years after total abdominal hysterectomy and bilateral salpingooophorectomy: A case report. Acta Obstet Gynecol Scand 2001;80:589-90. [ Links ]
8. Sampson JA. Endometrial carcinoma of the ovary, arising in endometrial tissue in that organ. Arch Surg 1925;10:1-72. [ Links ]
9. Hoang CD, Boettcher AK, Jessurun J, et al. An unusual rectosigmoid mass: Endometrioid adenocarcinoma arising in colonic endometriosis. Am Surg 2005;71:694-7. [ Links ]
10. Amano S, Yamada N. Endometrioid carcinoma arising from endometriosis of the sigmoid colon. Hum Pathol 1981;12:845-8. [ Links ]
11. Chen KTK. Endometrioid adenocarcinoma arising from colonic endometriosis mimicking primary carcinoma. Int J Gynecol Pathol 2002;21:285-8. [ Links ]
12. Slavin RE, Krun R, Dinh TV. Endometriosis-associated intestinal tumors: A clinical and pathological study of 6 cases with review of the literature. Hum Pathol 2000;31:456-63. [ Links ]
![]() Correspondence:
Correspondence:
José Andrés García Marín.
Services of General Surgery and Gastroenterology.
Hospital Universitario Morales Meseguer.
C/ Marqués de los Vélez, s/n. 3007 Murcia, Spain
e-mail: joseandresgarciamarin@gmail.com
Received: 12-12-2014
Accepted: 12-02-2015











 text in
text in