Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.5 Madrid may. 2016
Safety and risk factors for difficult endoscopist-directed ERCP sedation in daily practice: a hospital-based case-control study
Enrique Pérez-Cuadrado-Robles1, Abel González-Ramírez2, Ángel Lancho-Seco2, Eva Martí-Marqués2, Andrés Dacal-Rivas2, Elena Castro-Ortiz2, Roberto González-Soler2, Beatriz Álvarez-Suárez2, Dolores Tardáguila-García2, Alina López-Baz2, Alexia Fernández-López2 and Leopoldo López-Roses2
1 Department of Gastroenterology. Hospital Morales Meseguer. Murcia, Spain.
2 Department of Gastroenterology. Hospital Universitario Lucus Augusti. Lugo, Spain
ABSTRACT
Background: There are limited data concerning endoscopist-directed endoscopic retrograde cholangiopancreatography deep sedation. The aim of this study was to establish the safety and risk factors for difficult sedation in daily practice.
Patients and methods: Hospital-based, frequency matched case-control study. All patients were identified from a database of 1,008 patients between 2014 and 2015. The cases were those with difficult sedations. This concept was defined based on the combination of the receipt of high-doses of midazolam or propofol, poor tolerance, use of reversal agents or sedation-related adverse events. The presence of different factors was evaluated to determine whether they predicted difficult sedation.
Results: One-hundred and eighty-nine patients (63 cases, 126 controls) were included. Cases were classified in terms of high-dose requirements (n = 35, 55.56%), sedation-related adverse events (n = 14, 22.22%), the use of reversal agents (n = 13, 20.63%) and agitation/discomfort (n = 8, 12.7%). Concerning adverse events, the total rate was 1.39%, including clinically relevant hypoxemia (n = 11), severe hypotension (n = 2) and paradoxical reactions to midazolam (n = 1). The rate of hypoxemia was higher in patients under propofol combined with midazolam than in patients with propofol alone (2.56% vs. 0.8%, p < 0.001). Alcohol consumption (OR: 2.674 [CI 95%: 1.098-6.515], p = 0.030), opioid consumption (OR: 2.713 [CI 95%: 1.096-6.716], p = 0.031) and the consumption of other psychoactive drugs (OR: 2.015 [CI 95%: 1.017-3.991], p = 0.045) were confirmed to be independent risk factors for difficult sedation.
Conclusions: Endoscopist-directed deep sedation during endoscopic retrograde cholangiopancreatography is safe. The presence of certain factors should be assessed before the procedure to identify patients who are high-risk for difficult sedation.
Key words: Endoscopic retrograde cholangiopancreatography (ERCP). Sedation. Non-anesthesiologist administration of propofol (NAAP). Endoscopy.
Introduction
Many studies have demonstrated the safety of non-anesthesiologist administration of propofol (NAAP) in patients undergoing endoscopic procedures (1,2), primarily colonoscopy and upper-endoscopy (3,4). Propofol-based sedation has been demonstrated to be associated with rates of adverse events that are lower or similar to those of fentanyl/midazolam in standard (5) and advanced endoscopy procedures (6,7). Endoscopic retrograde cholangiopancreatography (ERCP) sedation is usually performed in elderly patients who may be at a greater risk of adverse events related to sedation. This procedure has been shown to be safe during NAAP sedation (8), and rates of deep duct cannulation similar to those of anesthesiologist-directed sedation have been achieved (9). The benefits of target-controlled infusion over patient-controlled sedation (10) and intermittent bolus application over continuous propofol infusion via an infusion pump during ERCP sedation have not yet been demonstrated (11).
Additionally, the tolerance and quality of the ERCP procedure under endoscopist-directed nurse-administered propofol-based sedation is unclear, especially for such high-risk patients. This approach may decrease the procedural and recovery times and provide high-quality examinations even in high-risk octogenarians (12). However, decreased satisfaction of patient and endoscopist during sedation in advanced gastrointestinal procedures compared with anesthesia providers has been described by other authors (13). Recent European guidelines (14) suggest the primary involvement of an anesthesiologist for American Society of Anesthesiologists (ASA) class ≥ III patients and in cases in which a long-lasting procedure is anticipated. However, according to the Spanish guidelines, the use of propofol by the endoscopy staff for ASA III patients is feasible and safe in experienced endoscopy units (15). Moreover, the response to propofol-based deep sedation can vary greatly between patients with similar risk factors, and it may be difficult to predict the procedural tolerance and ERCP length in daily practice.
Thus, there are still limited data concerning gastroenterologist-administered conscious sedation in ERCP. In this sense, it is important to assess sedation-related adverse events in addition to tolerance and discomfort during the procedure for the endoscopist and the patient. It is crucial to predict preoperative risk factors for difficult endoscopist-directed nurse-administered sedation during ERCP. All of these features may lead to inadequate examinations and aborted procedures. The aim of this study was to evaluate safety and risk factors for difficult endoscopist-administered sedations in ERCP procedures in daily practice.
Patients and Methods
Study population and study design
This was a hospital-based, frequency matched, case-control, retrospective study. All cases and controls were identified from a prospectively collected medical records database of 1,008 patients who underwent an ERCP at Hospital Universitario Lucus Augusti (Lugo, Spain) between January 2014 and December 2015. Cases were defined as patients with difficult endoscopist-directed sedations during ERCP. The eligibility criteria for controls included patients without difficult sedations during ERCP procedures from the same period of time and dataset. Controls were randomly selected by frequency matching according to age (± within 5 years) and sex. We designed the study with a 1:2 matching, i.e., two control subjects for each case. When a patient underwent several procedures, only the first was considered in the analysis. Patients who underwent anesthesiologist-administered sedation, those under 18 years of age and pregnant women were excluded. Subsequently, statistical analyses were performed to determine preoperative risk factors for difficult endoscopist-directed sedation.
Definitions and procedure
Three expert ERCP endoscopists (LLR, AGR, and ALS) performed all of the procedures with the patient in prone position or left lateral decubitus position when required. endoscopists were informed about basic and advanced life support and trained on propofol administration. No fellows in training performed the procedures, and carbon dioxide insufflation was used in all patients. The indication for the technique and the ASA score were considered. All patients provided informed consent both to undergo the ERCP procedure and to undergo moderate to deep sedation.
Patients received intravenous propofol as a single agent, fentanyl/midazolam or propofol combined with a small induction dose of midazolam as balanced propofol sedation (16) depending on the patient, the procedure characteristics and the endoscopist's preference. A trained nurse dedicated to NAAP administered the medications via intermittent bolus application or continuous propofol infusion via an infusion pump upon the instruction of the endoscopist. Patients received supplemental oxygen, they were monitored by continuous pulse oximetry and electrocardiography, and automated non-invasive blood pressure measurements were performed before the procedures. Capnographic monitoring was also used in some cases.
A difficult sedation/high sedation requirement was defined based on a definition similar to that previously described by Braunstein et al. [(17) as a combination of the receipt of a high dose (top 5%) of midazolam and/or propofol, the documentation of agitation or discomfort, the use of reversal agents or the occurrence of sedation-related adverse events. We clinically defined relevant hypoxemia as oxygen saturation < 90% that required an airway intervention such as bag-valve mask ventilation and/or an increase in the oxygen flow rate. Minor adverse events were also defined as requiring bag-mask ventilation with subsequent rapid recovery and no mechanical ventilation, cardiopulmonary resuscitation or death. Additionally, data regarding the interruption/incompletion of the ERCP procedure due to difficult sedation (and not due to procedure-related complications) were collected.
Statistical analysis
Categorical variables were compared using the chi_square test. Normally distributed continuous variables were analyzed with Student's t-tests, and non-normally distributed variables were analyzed with Mann-Whitney U-tests. Data were presented as mean (SD) or median (range). The following factors were evaluated with univariate analyses to determine whether they predicted difficult sedation: hypertension, diabetes, coronary heart disease, chronic respiratory disease, current or prior tobacco and alcohol consumption, psychiatric history, the use of benzodiazepines, opioids or other psychoactive drugs as home medications, inpatient/outpatient status, and body mass index. Multivariable logistic regression analysis was used to determine independent risk factors for difficult sedation using a backward selection method. The model was adjusted for age, sex and ASA score (ASA I-II and III-IV categories). 95% confidence intervals (CIs) were calculated for crude and adjusted odds ratios (ORs). All statistical tests were two-sided, and p-values < 0.05 were considered to be statistically significant. SPSS software version 23 (IBM; SPSS Inc., Chicago, IL, USA) was used.
Results
Patients
Of the 1,008 patients who underwent ERCP, 626 were under moderate to deep sedation by propofol alone (62.1%), 304 were under fentanyl/midazolam sedation (30.16%), and 78 received combined propofol and fentanyl/midazolam (n = 78, 7.74%). One hundred and eighty-nine patients (63 cases and 126 controls) were included in the analysis. According to the American Society of Anesthesiologists, patients were classified as ASA I (n = 3, 1.59%), ASA II (n = 69, 36.51%), ASA III (n = 109, 57.67%) or ASA IV (n = 8, 4.23%). The median propofol dose administered across all patients (n = 189) was 173 mg (range: 30-843). The median administered doses of propofol in case and control patients for whom it was used as single agent were 367.5 mg (range: 75-873) and 157 mg (range: 30-241), respectively.
Sixty-three cases (mean age: 68.86 ± 16.63 years old, 71.43% male) underwent ERCP due to gallstone disease (n = 36, 57.14%), benign biliary stenosis (n = 9, 14.3%), malignant biliary stenosis (n = 15, 23.81%) and other indications (n = 3, 4.8%). Sedation was administered via propofol alone (n = 37, 58.73%), fentanyl/midazolam (n = 14, 22.22%) or a mix of both (n = 12, 19.05%). The patients were mainly classified as requiring difficult sedations due to high-dose requirements (n = 35, 55.56%), sedation-related adverse events (n = 14, 22.22%), the use of reversal agents (n = 13, 20.63%) and agitation/discomfort (n = 8, 12.7%). Six patients were classified in several categories. However, procedures were aborted or not completed only in 14 cases (22.22%) due to adverse events (78.57%) and agitation/discomfort (21.43%). Two cases that presented with moderate hypoxemia requiring endoscope withdrawal were not considered as aborted because procedures were completed quickly with bag-valve masks after the patients recovered.
Thus, the total rate of sedation-related adverse events was 1.39% (Table I), and these events included hypoxemia (Sat02 < 90%; n = 11, with associated severe bronchospasms in three cases), severe hypotension with bradycardia after propofol administration (n = 2) and paradoxical reactions to midazolam (n = 1). No hypoxemia cases had high-dose sedation requirements, and the majority of the instances of hypoxemia occurred at the beginning of the procedure under propofol alone (n = 5, 45.45%), whereas fewer cases occurred under fentanyl or midazolam (n = 4, 36.36%) or a combination of the two (n = 2, 18.18%). The rate of hypoxemia under propofol alone was lower than those under propofol combined with midazolam (0.8% vs. 2.56%, p < 0.001) and midazolam alone (0.8% vs. 1.32%, p < 0.001). Six cases (54.54%) required airway interventions, including three with Guedel airways, and rapid recoveries were observed in all of these cases. The median propofol and midazolam doses among patients with high-dose requirements were 376 mg (range: 330-873) and 12.5 mg (range: 0), respectively. The majority of the patients who consumed alcohol required high-doses (n = 11, 84.62%). The body mass indices did not differ between patients with and without high-dose requirements (28.32 ± 4.56 vs. 25.61 ± 5.21 kg/m2, respectively, p = 0.072). There were no sedation-related deaths or major complications requiring mechanical ventilation via endotracheal intubation.
Among the 945 remaining patients in the database, 126 fulfilled all of the selection criteria and formed the control group after frequency matching. There were no differences between case and control groups in terms of ERCP indications (p = 0.295) or ASA scores (p = 0.204).
Risk factors for difficult ERCP sedation
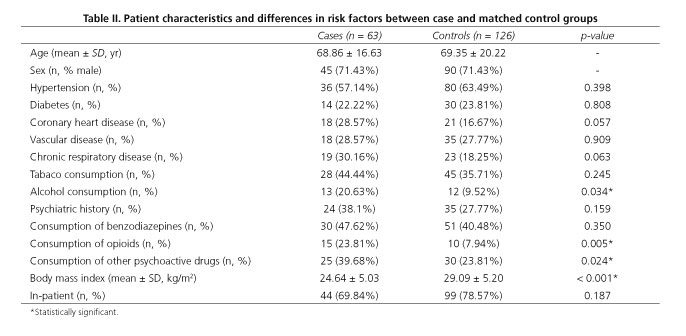
Patient characteristics and unadjusted differences between cases and age- and sex-matched controls are displayed in table II. Alcohol consumption (20.63% vs. 9.52%, p = 0.034), opioid consumption (23.81% vs. 7.94%, p = 0.005), other psychoactive drug consumption (39.68% vs. 23.81%, p = 0.024) and body mass index (24.64 ± 5.03 vs. 29.09 ± 5.20, p < 0.001) differed significantly between case and control groups. There were differences between the groups in coronary heart disease and chronic respiratory disease, but these differences did not achieve significance. Concerning alcohol consumption, 4 and 6 case patients had malignant neoplasms and chronic pancreatitis, respectively, whereas only 1 and 3 controls presented with these diseases. Current consumption did not significantly differ between the cohorts (61.53% vs. 33.33%, p = 0.081). The consumption of opioids was related to chronic pancreatitis (n = 7), malignant neoplasms (n = 12) and other conditions (n = 6). Fifty per cent of the controls and 40% of the cases who consumed opioids had malignant pancreaticobiliary neoplasms. Multivariable analysis (Table III) revealed that the consumptions of alcohol, opioids and psychoactive drugs were independent risk factors for difficult endoscopist-directed nurse-administered sedation based on the crude ORs. The ORs did not vary significantly according to age, sex or ASA score in the adjusted analysis.
Discussion
In the present matched case-control study, we reported 63 cases with difficult ERCP sedations and 126 controls from an ERCP referral hospital database of 1,008 procedures. Endoscopist-directed nurse-administered sedation has been demonstrated to be safe with a global rate of sedation-related adverse events of 1.39%. Additionally, the consumptions of alcohol, opioids and other psychoactive drugs were demonstrated to be independent risk factors for difficult sedations based on an analysis that was adjusted for age, sex and ASA score.
ERCP has previously been reported to be safe under NAAP sedation with a low rate of adverse events (18,19) and ERCP has also been reported to be feasible without intubation for the majority of healthier patients (20). However, it is important to consider all patients with difficult sedations from a global perspective, including cases with poor tolerance, the use of reversal agents and high-dose requirements rather than considering only those who experience adverse events. In this sense, the present study sought to analyze the rate of and risk factors for difficult NAAP sedation during daily practice while considering all potential patients in whom sedation may alter the expected ERCP results. This fact may be of great importance, because the majority of these cases are fragile old patients with multiple illnesses and repeated ERCPs or long procedures that lead to extra risks.
In a comparative meta-analysis of pooled results, Goudra et al. (13) reported a hypoxemia rate of 0.133 (95% CI: 0.117-0.152) among NAAP advanced gastrointestinal endoscopic procedures. Although hypoxemia did not affect the endoscopic procedures and was corrected with oxygen supplementation, fentanyl/midazolam associated with propofol in NAAP sedation during ERCP procedures has been reported to result in a higher rate of hypoxemia than propofol alone (21). In our study, we did not consider transient and self-limited hypoxemia, which did not affect the ERCP procedures or patient management. We observed differences in clinically relevant hypoxemia rates between patients who received propofol alone or propofol combined with midazolam (0.8% vs. 2.56%, p < 0.001). Globally, 78.57% of hypoxemia cases required an interruption of the procedure, but all patients achieved rapid recoveries, and 42.86% required airway interventions.
Interestingly, hypoxemia was not related to propofol dose. Therefore, patients who were classified as "difficult sedations" due to high-dose requirements were probably so classified due to long procedures, alcohol consumption (31.43%) or individual variability. The lack of procedure time data limits the interpretation of this result, but there were no ERCPs aborted due to this reason. Additionally, it would have been interesting to examine the induction propofol doses and not simply the total amounts because the latter may have been more strongly related to difficult sedations than long or technically challenging procedures. Regarding tolerance and endoscopist/patient satisfaction with the procedure, it was difficult to assess these features and their influences on the ERCPs. The state of anxiety prior to an endoscopic procedure has been described as a risk factor for a poor tolerance even in patients without psychiatric histories or psychoactive drug or benzodiazepine use. In our retrospective study, poor tolerance was only reported as clinically significant in terms of endoscopist satisfaction in 8 cases. However, recovery times, state of anxiety and patient satisfaction were not noted in our series.
Regarding factors that are potentially related to difficult sedation, the majority of the studies to date have performed qualitative analyses that considered general diseases and histories of drug consumption. It must be noted that patients who consume different numbers and quantities of drugs may have different risk factors and require different propofol/midazolam for deep sedation. These facts can be especially relevant among patients consuming benzodiazepines or psychoactive drugs. Older patients are increasingly likely to be on low doses of psychotropic medication, and such low doses are probably as important in terms of required sedation doses as the use of high-doses or multiple psychotropics. This supposition may explain why benzodiazepine intake was not a statistically significant risk factor in the present study. In agreement with other reports (17), alcohol consumption (OR: 2.674 [CI 95%: 1.098-6.515], p = 0.030), opioid consumption (OR: 2.713 [CI 95%: 1.096-6.716], p = 0.031) and the consumption of other psychoactive drugs (OR: 2.015 [CI 95%: 1.017-3.991], p = 0.045) were confirmed to be independent risk factors for endoscopist-directed difficult moderate-deep sedation in the multivariable analysis in our series. Body mass indices differed significantly between case and control groups (24.64 ± 5.03 vs. 29.09 ± 5.20, respectively, p < 0.001). However, this difference was related to the higher proportion of cases with chronic pancreatitis and/or alcohol consumption and, therefore, worse nutritional statuses.
The main strength of the present study is the inclusion of a heterogeneous group of patients with different ASA risks, ERCP indications and types of sedation, which enabled the assessment of ERCP deep sedation in endoscopists' daily practice. In addition to those previously mentioned, the limitations of the present study included the low number of procedures and the retrospective design.
In conclusion, our results suggest that endoscopist-directed nurse-administered deep sedation during ERCP procedures is safe even for high-ASA risk patients based on the low rate of sedation-related adverse events. Additionally, the presence of certain factors should be systematically assessed prior to the procedure to identify patients who are at a high risk for difficult sedation.
References
1. Sieg A; bng-Study-Group, Beck S, et al. Safety analysis of endoscopist-directed propofol sedation: A prospective, national multicenter study of 24,441 patients in German outpatient practices. J Gastroenterol Hepatol 2014; 29:517-23. DOI: 10.1111/jgh.12458. [ Links ]
2. De Paulo GA, Martins FP, Macedo EP, et al. Sedation in gastrointestinal endoscopy: A prospective study comparing nonanesthesiologist-administered propofol and monitored anesthesia care. Endosc Int Open 2015;3:E7-E13. DOI: 10.1055/s-0034-1377835. [ Links ]
3. Poincloux L, Laquière A, Bazin JE, et al. A randomized controlled trial of endoscopist vs. anaesthetist-administered sedation for colonoscopy. Dig Liver Dis 2011;43:553-8. DOI: 10.1016/j.dld.2011.02.007. [ Links ]
4. Molina-Infante J, Dueñas-Sadornil C, Mateos-Rodríguez JM, et al. Nonanesthesiologist-administered propofol versus midazolam and propofol, titrated to moderate sedation, for colonoscopy: A randomized controlled trial. Dig Dis Sci 2012;57:2385-93. DOI: 10.1007/s10620-012-2222-4. [ Links ]
5. Rex DK, Deenadayalu VP, Eid E, et al. Endoscopist-directed administration of propofol: A worldwide safety experience. Gastroenterology 2009;137:1229-37;quiz 1518-9. DOI: 10.1053/j.gastro.2009.06.042. [ Links ]
6. Sethi S, Wadhwa V, Thaker A, et al. Propofol versus traditional sedative agents for advanced endoscopic procedures: A meta-analysis. Dig Endosc 2014;26:515-24. DOI: 10.1111/den.12219. [ Links ]
7. Vargo JJ, Zuccaro G Jr, Dumot JA, et al. Gastroenterologist-administered propofol versus meperidine and midazolam for advanced upper endoscopy: A prospective, randomized trial. Gastroenterology 2002;123:8-16. DOI: 10.1053/gast.2002.34232. [ Links ]
8. Khan HA, Umar M, Tul-Bushra H, et al. Safety of non-anesthesiologist-administered propofol sedation in ERCP. Arab J Gastroenterol 2014;15:32-5. DOI: 10.1016/j.ajg.2014.01.011. [ Links ]
9. Mehta PP, Vargo JJ, Dumot JA, et al. Does anesthesiologist-directed sedation for ERCP improve deep cannulation and complication rates? Dig Dis Sci 2011;56:2185-90. DOI: 10.1007/s10620-011-1568-3. [ Links ]
10. Mazanikov M, Udd M, Kylänpää L, et al. A randomized comparison of target-controlled propofol infusion and patient-controlled sedation during ERCP. Endoscopy 2013;45:915-9. DOI: 10.1055/s-0033-1344712. [ Links ]
11. Riphaus A, Geist C, Schrader K, et al. Intermittent manually controlled versus continuous infusion of propofol for deep sedation during interventional endoscopy: A prospective randomized trial. Scand J Gastroenterol 2012;4:1078-85. DOI: 10.3109/00365521.2012.685758. [ Links ]
12. Riphaus A, Stergiou N, Wehrmann T. Sedation with propofol for routine ERCP in high-risk octogenarians: A randomized, controlled study. Am J Gastroenterol 2005;10:1957-63. DOI: 10.1111/j.1572-0241.2005.41672.x. [ Links ]
13. Goudra BG, Singh PM, Gouda G, et al. Safety of non-anesthesia provider-administered propofol (NAAP) sedation in advanced gastrointestinal endoscopic procedures: comparative meta-analysis of pooled results. Dig Dis Sci 2015;60:2612-27. DOI: 10.1007/s10620-015-3608-x. [ Links ]
14. Dumonceau JM, Riphaus A, Schreiber F, et al. Non-anesthesiologist administration of propofol for gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy, European Society of Gastroenterology and Endoscopy Nurses and Associates Guideline - Updated June 2015. Endoscopy 2015;47:1175-89. DOI: 10.1055/s-0034-1393414. [ Links ]
15. Igea F, Casellas JA, González-Huix F, et al. Clinical practice guidelines of the Sociedad Española de Endoscopia Digestiva. Rev Esp Enferm Dig 2014;106:195-211. [ Links ]
16. Vargo JJ, Cohen LB, Rex DK, et al. Position statement: Nonanesthesiologist administration of propofol for GI endoscopy. Gastroenterology 2009;137:2161-7. DOI: 10.1053/j.gastro.2009.09.050. [ Links ]
17. Braunstein ED, Rosenberg R, Gress F, et al. Development and validation of a clinical prediction score (the SCOPE score) to predict sedation outcomes in patients undergoing endoscopic procedures. Aliment Pharmacol Ther 2014;40:72-82. DOI: 10.1111/apt.12786. [ Links ]
18. Ikeuchi N, Itoi T, Gotoda T, et al. Feasibility of non-anesthesiologist-administered propofol sedation for emergency endoscopic retrograde cholangiopancreatography. Gastroenterol Res Pract 2015;2015:685476. DOI: 10.1155/2015/685476. [ Links ]
19. Kongkam P, Rerknimitr R, Punyathavorn S, et al. Propofol infusion versus intermittent meperidine and midazolam injection for conscious sedation in ERCP. J Gastrointestin Liver Dis 2008;17:291-7. [ Links ]
20. Barnett SR, Berzin T, Sanaka S, et al. Deep sedation without intubation for ERCP is appropriate in healthier, non-obese patients. Dig Dis Sci 2013;58:3287-92. DOI: 10.1007/s10620-013-2783-x. [ Links ]
21. Angsuwatcharakon P, Rerknimitr R, Ridtitid W, et al. Cocktail sedation containing propofol versus conventional sedation for ERCP: A prospective, randomized controlled study. BMC Anesthesiol 2012;12:20. DOI: 10.1186/1471-2253-12-20. [ Links ]
![]() Correspondence:
Correspondence:
Enrique Pérez-Cuadrado-Robles.
Department of Gastroenterology.
Hospital Morales Meseguer.
Av. Marqués de los Vélez, s/n.
30008 Murcia, Spain
e-mail: kikemurcia@gmail.com
Received: 26-01-2016
Accepted: 14-02-2016