My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.7 Madrid Jul. 2016
https://dx.doi.org/10.17235/reed.2015.3828/2015
Appendicular bleeding: an excepcional cause of lower hemorrhage
Sangrado apendicular: una causa excepcional de hemorragia digestiva baja
Marta Magaz-Martínez1, Javier Martín-López2, Juan de-la-Revilla-Negro1, Irene González-Partida1, Tania de-las-Heras3, María Rosario Sánchez-Yuste2, Roberto Ríos-Garcés4, Clara Salas-Antón2 and Luis Abreu-García1
Departments of 1Digestive Diseases, 2Pathology, 3Radiology and 4Internal Medicine. Hospital Universitario Puerta de Hierro Majadahonda. Madrid, Spain
ABSTRACT
Chronic complications of acute appendicitis managed in a conservative manner are not frequent. We present a case of acute lower gastrointestinal hemorrhage in a young patient with a previous acute appendicitis without surgical intervention. The colonoscopy detected an appendicular bleeding which was surgically treated. The anatomopathological diagnosis was granulomatous appendicitis. The clinical evolution of the patient was favorable without bleeding recurrence. Appendicular hemorrhage can be an unusual complication -however potentially severe- of acute appendicitis not treated surgically.
Key words: Lower gastrointestinal hemorrhage. Granulomatous appendicitis.
RESUMEN
Las complicaciones crónicas de la apendicitis aguda manejada de forma conservadora son infrecuentes. Presentamos un caso de hemorragia digestiva baja aguda en paciente joven con antecendente de apendicitis aguda no intervenida. En la colonoscopia se detectó un sangrado apendicular que se trató quirúrgicamente. El diagnóstico anatomopatológico fue de apendicitis granulomatosa. La evolución clínica del paciente fue favorable sin recidiva hemorrágica. La hemorragia apendicular puede ser una complicación inusual potencialmente grave de la apendicitis aguda no intervenida.
Palabras clave: Hemorragia digestiva baja. Apendicitis granulomatosa.
Introduction
Severe lower gastrointestinal bleeding (LGIB) accounts for 15% of all cases of acute LGIB (1). The most frequent causes of rectorrhagia without hemodynamic repercussion are hemorrhoidal pathology and neoplasias. Acute lower gastrointestinal bleeding is usually related to bleeding of diverticular origin or with vascular ectasias. Patients aged < 30 that debut with an important LGIB episode usually present lesions due to vascular malformations (Dieulafoy's lesion) or intestinal malformation (Meckel's diverticulum), and their etiological diagnosis is rather difficult sometimes.
Surgical management of appendicitis has been a subject of debate. Many surgeons are in favor of an immediate appendectomy. However, the potential morbility, or even mortality, as a result of this technique lead other group of experts to defend a more conservative management (2,3).
Long term complications of this therapeutical non-aggressive attitude are not well known. Hereunder we describe a case of acute appendicitis that was not treated surgically and its long term unusual and potentially severe evolution (4).
Case report
We present the case of a Caucasian male aged 22 that comes to Emergency Service in our hospital with rectal bleeding. The only relevant personal background relates to appendicitis a year before, managed in a conservative manner with antibiotics. The patient shows a 3-4 day evolution consisting of bright red blood emanating from the rectum, not accompanied by defecation or other symptoms.
Several weeks before admission in the Emergency Service he had undergone an analytic control including a complete blood count (CBC) with normal levels of hemoglobin (13.3 g/dl).
Upon admission in Emergency the patient presented with hemodynamic stability, blood pressure 138/61 mmHg and a heart rate of 84 bpm. The physical exploration highlighted a pallor of the skin and the mucous membranes, perspiration and mucosal dryness, whereas the rest of the exploration was anodyne. The rectal examination showed plain rectal bleeding, but rectal masses could not be detected. The inspection around the annus showed no fissures or hemorrhoids.
During his stay in Emergency two peripheral lines were secured, blood tests were crossmatched and we started with the infusion of 500 cc of physiological saline at 0.9%. An urgent blood test highlighted a normocytic anemia (hemoglobin 7.3 g/dL and mean corpuscular volume MCV of 87.40 fL). The rest of the blood count, biochemistry and coagulation maintained values within the range of normality. Considering the hemodynamic stability of the patient we decided to schedule an elective colonoscopy prior colonic preparation with polyethylene glycol and transfusion of 4 etrytrocyte concentrates. The colonoscopy was carried out 24 hours after and it reached the terminal ileum. Blood remnants were only detected in the transverse and ascending colon. Ileoscopy was normal, showing bile remains. In the absence of conclusive findings, we carried out an oral panendoscopy, exploring the esophagus, the stomach and the duodenum until the second duodenal portion, but did not observe traces of blood or potentially bleeding injuries. We decided to complete the study by means of a capsule endoscopy. Nevertheless, 12 hours after the endoscopic examinations, the patient presented with a new episode of rectorrhagia with hemodynamic repercussion and new anemia to a 7.6 g/dl hemoglobin (in spite of the transfusion of six erytrocyte concentrates, what led us to carry out an urgent CT angiography. Thereby we found hyperdensity at the cecum level, findings that suggested active endoluminal bleeding. (Figs. 1 and 2). After the hemodynamic stabilization of the patient we repeated the colonoscopy. The colonoscope was introduced until the terminal ileon, that showed a normal mucosa without blood remnants. We examine the cecum where abundant traces of blood remnants and blood clots are detected, but no potentially bleeding mucosal lesions. At the base of the appendiceal orifice we observe an irregular structure with active bleeding at the base (Fig. 3), which suggests that it might correspond to a blood vessel.
With the clinical suspicion that it may be a severe acute LGIB of appendicular origin we decided to carry out an urgent surgical intervention, performing an appendectomy with associated removal of the cecum. The postoperative course was uneventful and the patient is discharged from hospital 72 hours after surgery. The clinical follow-up three and six months after discharge shows that the patient presents no further symptoms. He has not suffered new episodes of macroscopic bleeding and the recovery from anemia is confirmed as well.
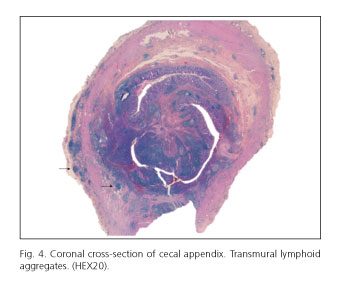
Upon examination of the pieces removed the only significant thing was a cecal appendix with diffuse enlargement. Under the microscope we could observe non-necrotizing epitheliod granulomas, scattered along the wall, ulcers, fissures and cryptal abscesses in the mucosa. The diagnosis thereof was chronic granulomatous appendicitis (Figs. 4 and 5).
Discussion
Granulomatous appendicitis is a rare clinicopathological finding histologically characterized by the presence of appendicular granulomas. Granulomas are chronic inflammatory lesions consisting of clusters of epithelioid histiocytes, occasionally accompanied by multinucleated giant cells and lymphocytes as well as plasmatic cells (5). This entity accounts for less that 2% of all appendicitis. It was thought at first that it was a manifestation of Crohn's disease. However, only 5-10% of all granulomatous appendicitis develops this disease. Other etiologies are varied, highlighting the sarcoidosis, the reaction of foreign-body granuloma and intestinal infectious diseases such as tuberculosis, parasitic disease and more frequently the Yersinina species. Recently subacute appendicitis has been described as the most common cause of this entity. This condition produces a granulomatous reaction in relation to a secondary inflammatory response to acute appendicitis managed conservatively, with a postponed appendectomy (4). Unlike our case, the common clinical presentation is the abdominal pain (6), whereas rectal bleeding is a truly rare event. We are therefore faced with an exceptional case. The diagnosis is usually made by imaging, while the definitive diagnosis based on histology. Since in our case the presentation was rectal bleeding, the differential diagnosis should be made with other causes of severe gastrointestinal bleeding in young patients. The definitive management of granulomatous appendicitis is based on the appendectomy (7) and as a whole the cases reviewed in the literature have a good long term prognosis (8). To date, less than 30 cases of appendiceal bleeding have been reported. Those cases of bleeding of appendicular origin included inflammatory bowel disease, tuberculosis, cases of intussusception or angiodysplasias among other etiologies. It is really difficult to make a diagnosis with endoscopic visualization. And in most cases it is still necessary to conduct a removal of the cecum (or sometimes an associated hemicolectomy) to control the bleeding (9).
To conclude, granulomatous appendicitis in the context of a subacute appendicitis may appear clinically as severe lower gastrointestinal bleeding due to appendicular bleeding with important clinical and analytical repercussion. The combination of dynamic radiological tests and endoscopy during the acute bleeding process increases the diagnostic yield, but in most cases it requires a surgical management for the final resolution of the case (10).
References
1. García Sánchez N, González Galilea A, López Vallejos P, et al. Role of early colonoscopy in severe acute lower gastrointestinal bleeding. Gastroenterol Hepatol 2001;24:327-32. [ Links ]
2. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: Meta-analysis of randomised controlled trials. BMJ 2012;344:e2156. DOI: 10.1136/bmj.e2156. [ Links ]
3. Wilms IM, de Hoog DE, de Visser DC, et al. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst Rev 2011;(11):CD008359. DOI: 10.1002/14651858.CD008359.pub2. [ Links ]
4. Bronner MP. Granulomatous appendicitis and the appendix in idiopathic inflammatory bowel disease. Semin Diagn Pathol 2004;21(2):98-107. DOI: 10.1053/j.semdp.2004.12.001. [ Links ]
5. Yilmaz M, Akbulut S, Kutluturk K, et al. Unusual histopathological findings in appendectomy specimens from patients with suspected acute appendicitis. World J Gastroenterol 2013;19:4015-22. DOI: 10.3748/wjg.v19.i25.4015. [ Links ]
6. Bianchi A, Hidalgo LA, Fantova MJ, et al. Granulomatous disease of the cecal appendix. Clinical significanc. Med Clin (Barc) 2004;122:798. DOI: 10.1157/13062677. [ Links ]
7. Alhambra Rodríguez de Guzmán C, Morales Marín VJ, Salvelio Picazo Yeste J, et al. Granulomatous appendicitis: An uncommon cause of acute abdomen. Cir Esp 2014. pii: S0009-739X(13)00381-3. DOI: 10.1016/j.ciresp.2013.09.019. [ Links ]
8. Tucker ON, Healy V, Jeffers M, et al. Granulomatous appendicitis. Surgeon 2003;1:286-9. DOI: 10.1016/S1479-666X(03)80047-1. [ Links ]
9. Konno Y, Fujiya M, Tanaka K, et al. A therapeutic barium enema is a practical option to control bleeding from the appendix. BMC Gastroenterol 2013;13:152. DOI: 10.1186/1471-230X-13-152. [ Links ]
10. Gu J, Allan C. Idiopathic granulomatous appendicitis: a report of three consecutive cases. ANZ J Surg 2010;80:201. DOI: 10.1111/j.1445-2197.2010.05237.x. [ Links ]
![]() Correspondence:
Correspondence:
Marta Magaz Martínez.
Department of Digestive Diseases.
Hospital Universitario Puerta de Hierro Majadahonda.
C/ Manuel de Falla, 1.
28222 Majadahonda, Madrid. Spain
e-mail: martamagazm@gmail.com
Received: 28/04/2015
Accepted: 06/05/2015











 text in
text in