Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.8 Madrid ago. 2016
https://dx.doi.org/10.17235/reed.2016.4067/2016
Readmissions due to acute biliary edematous pancreatitis in patients without cholecystectomy
Reingresos por pancreatitis aguda biliar edematosa en pacientes sin colecistectomía
Eva Barreiro-Alonso, Alejo Mancebo-Mata, Pilar Varela-Trastoy, María Pipa-Muñiz, Eduardo López-Fernández, Rafael Tojo-González, Mónica García-Espiga, Rosa García-López, José Martín Pérez-Pariente and Francisco Javier Román-Llorente
Department of Digestive Diseases. Hospital de Cabueñes. Gijón, Asturias. Spain
ABSTRACT
Objectives: Analyzing the readmission of patients with acute biliary edematous pancreatitis (ABEP) without cholecystectomy despite a previous episode of mild acute gallstone pancreatitis or lithiasic cholecystitis. Calculating the health costs associated with the non-performance of cholecystectomy.
Materials and methods: Prospective observational study conducted at a tertiary hospital (Hospital de Cabueñes. Gijón, Asturias. Spain) from July to November 2014. The study has consecutively included inpatients suffering from ABEP who: a) had suffered a previous episode of mild acute gallstone pancreatitis or cholecystitis at least 2 weeks before readmission; and b) had not undergone cholecystectomy despite the lack of contraindications.
Results: During the research period, 9 patients (7 females and 2 males) with a mean age of 65.3 years (standard deviation [SD] 19.2) were readmitted. The median number of days between the previous episode of ABEP or cholecystitis and the readmission was 114 days (interquartile range [IQR] 111.0). Reported median overall length of hospital stay was 10 days (IQR = 2.0). Patients underwent a mean of 2.8 (SD = 1.2) ultrasound scans, 1.3 (SD = 0.9) abdominal and pelvic CT, 0.8 (SD = 1.0) MRCP and 0.2 (SD = 0.4) ERCP. The mean cost per patient for each readmission, including hospital stay (143.0 €/day), Emergency Service (332.31 €) and tests performed was 2,381.70 €/patient.
Conclusions: Not performing a cholecystectomy within two weeks after a first episode of mild ABEP or cholecystitis contributes to patient readmission due to recurrent pancreatitis, resulting in avoidable treatment costs.
Key words: Pancreatitis. Gallstone. Cholecystectomy. Costs. Length of stay.
RESUMEN
Objetivos: analizar los reingresos de pacientes con pancreatitis aguda biliar edematosa (PABE) sin colecistectomía a pesar de un episodio previo de pancreatitis aguda biliar leve o colecistitis litiásica. Calcular el coste sanitario asociado a la no realización de colecistectomía.
Material y métodos: estudio observacional prospectivo realizado en el Hospital de Cabueñes, entre julio y noviembre de 2014. Se incluyeron consecutivamente los pacientes ingresados en el Servicio de Digestivo con PABE que: a) habían presentado un episodio previo de pancreatitis aguda biliar leve o colecistitis al menos dos semanas antes del reingreso; y b) no se les había realizado colecistectomía pese a ausencia de contraindicaciones.
Resultados: durante el periodo de estudio reingresaron 9 pacientes, 7 mujeres y 2 varones, con una edad media de 65,3 años (desviación estándar [DE] = 19,2). La mediana de días transcurridos desde el episodio previo de PABE o colecistitis hasta su reingreso fue de 114 días (recorrido intercuartílico [RIC] = 111,0). La estancia global mediana de los pacientes fue de 10 días (RIC = 2,0). Los pacientes realizaron una media de 2,8 (DE = 1,2) ecografías, 1,3 (DE = 0,9) TC abdómino-pélvicos, 0,8 (DE = 1,0) RM y 0,2 (DE = 0,4) CPRE. El coste medio de cada reingreso por paciente, incluyendo la estancia hospitalaria (143,0 €/día), en el servicio de Urgencias (332,31 €) y las pruebas realizadas, fue de 2.381,70 €/paciente.
Conclusiones: la no realización de colecistectomía en las 2 semanas posteriores a un primer episodio de PABE leve o colecistitis contribuye a los reingresos por pancreatitis recurrentes con los consecuentes gastos evitables asociados.
Palabras clave: Pancreatitis. Cálculos biliares. Colecistectomía. Costes. Duración de la estancia.
Introduction
Cholelithiasis is the most common cause of acute pancreatitis in the Western world (1). Diagnosis is based on the existence of at least two of the following features: acute onset of persistent abdominal pain located in the epigastrium often radiating to the back; elevated levels of serum pancreatic enzymes (lipase or amylase), at least three times greater than the upper limit of normal levels; findings of acute pancreatitis on contrast-enhanced computerized tomography (CT), magnetic resonance imaging (MRI) or transabdominal ultrasound (US). Additionally, in the absence of any other compelling etiology, the existence of biliary tract stones has to be proven (1-3). The purpose of using imaging techniques in gallstone disease is to identify local complications and to assess the severity of pancreatitis. Severity stratification is essential to ensure that adequate care and interventions are provided (1,2). In most cases, acute gallstone pancreatitis (AGSP) is interstitial edematous pancreatitis (ABEP), a mild and self-limiting disease. However, in 20% of cases, pancreatitis can be necrotizing and severe with a mortality rate up to 30% (1,2).
Cholecystectomy is the treatment of choice for mild ABEP. When a cholecystectomy is not performed, this results in recurrence in up to 30-40% of patients within 2 weeks after the initial episode (4,5) and affects two thirds of patients within the three months following the index case (1). Recurrent pancreatitis can result in ABEP or can be more serious than the initial presentation, which happens in between 4% and 50% of cases depending on the series, with a mortality rate of 10% and morbidity of up to 40% (1).
Several studies have shown that in mild AGSP, early laparoscopic cholecystectomy within the first three days of hospitalization is safe, cost-effective (6), and does not increase local or systemic complications regarding its delayed performance (7). Guidelines from the American College of Gastroenterology, the British Society of Gastroenterology and the Recommendations of the Spanish Club for the Treatment of Acute Pancreatitis support performing laparoscopic surgery within 48 hours of admission (1,5,8,9). When this is not possible, cholecystectomy has to be performed after clinical recovery and normalization of pancreatic enzymes; it is recommended to carry out the intervention within 2 to 4 weeks after presentation of the pancreatitis (5).
At Hospital de Cabueñes, cholecystectomy is not performed during admission. The goal of this study is to review the readmission of patients with ABEP without cholecystectomy after an initial admission due to ABEP or lithiasic cholecystitis two weeks after medical discharge, and to calculate the health costs associated to these readmissions, as this point has not been considered in other published studies.
Material and methods
Study design and patients
Prospective observational study conducted from July to November 2014 (4 months) at a tertiary hospital. The study has consecutively included patients admitted in the Department of Digestive Diseases suffering from AGSP who met the following criteria: a) had suffered a previous episode of mild ABEP or lithiasic cholecystitis at least 2 weeks before readmission; and b) had not undergone cholecystectomy despite the lack of contraindications. Patients who in the previous AGSP admission had experienced any of the following symptoms were excluded: a) chronic pancreatitis or etiology other than biliary; b) severe clinical and analytical criteria, defined by RANSON score > 3 and/or APACHE II > 8 within the first three days of admission; and c) radiological evidence of pancreatic and/or peripancreatic necrosis according to the Atlanta classification (2). At our hospital, patients with pancreatitis are admitted to the department of Digestive Diseases even though they suffer from recurrent ABEP.
Variables
Several data were collected for this study: demographic variables such as gender, age or mortality; and quantitative information concerning clinic management (the number of readmissions after the first ABEP episode or lithiasic cholecystitis, days of hospitalization, period between initial admission for ABEP and subsequent readmissions). The following diagnostic tests performed in patients were also recorded: abdominal ultrasound (US), abdominopelvic CT, magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP). Chest and abdomen X-ray taken during admission have been included in the costs associated with the Emergency Service. Health costs, including diagnostic tests, administrative issues, emergency care and admission in the Digestive Diseases Department, together with the cost of the elective laparoscopic cholecystectomy (surgery and hospital stay), have been calculated based on the data provided by the Accounting Department.
Sample size and bias
Patients meeting inclusion and exclusion criteria constitute the study population. This approach avoids sources of potential bias in the estimation of sample size.
Data and statistical analysis
A descriptive analysis of the categorical variables was undertaken. Continuous variables with symmetric distribution are displayed with the mean and standard deviation (SD). Furthermore, the range of minimum and maximum value was included. Quantitative variables with asymmetric distribution are displayed with the median and the interquartile range (IQR) as a measure of data variability. Statistical analyses were performed with Microsoft Office EXCEL 2007 and IBM SPSS Statistics version 22.
Results
During the research period, 9 patients (7 females [78%] and 2 males [22%]) with a mean age of 65.3 years (SD = 19.2) (range 30-84) were admitted. The median number of days between the previous episode of ABEP or lithiasic cholecystitis and the readmission was 114 days (interquartile range 111.0). The range of readmission per patient during the study was from 1-3, with a mean of 1.4 (SD = 0.7) readmissions per patient. Readmissions had a median length of 8.3 days (IQR = 4.0). Reported median overall length of hospital stay was 10 days (IQR = 2.0) per patient taking into account readmissions during the period of study. Patients underwent a mean of 2.8 (SD = 1.2) US, 1.3 (SD = 0.9) abdominopelvic CT, 0.8 (SD = 1.0) MRCP and 0.2 (SD = 0.4) ERCP. The median of days from the initial admission due to ABEP or lithiasic cholecystitis and subsequent readmission for recurrent ABEP was 114 days (IQR = 111), and the median of days until surgery was 207 days (IQR = 114). One patient with recurrent ABEP had not been operated on at the end of the study. Neither severe recurrent ABEP nor deaths have been reported among inpatients (Table I). During the period of study, 27 patients with AGSP were admitted, two of them in a serious condition.
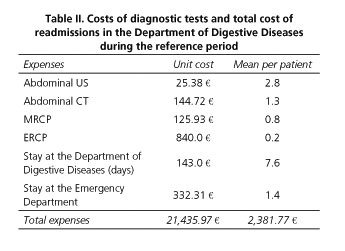
During the study, a total of 25 US, 12 CT, 7 MRCP and 2 ERCP were ordered, with a mean per patient of: 2.8 (SD = 1.2) US; 1.3 (SD = 0.9) CT; 0.8 (SD = 1) MRCP and 0.2 (SD = 0.4) ERCP. Health costs of these diagnostic tests, using the prices applied in 2014 at the Hospital de Cabueñes as a reference, were 25.38 € per US, 144.72 € per CT, 125.93 € per MRCP and 840.0 € per ERCP.
Mean total cost per patient during the reference period including hospital stay in the Digestive Diseases Department was 143.0 €/day, the Emergency Service was 332.31 €, and the abovementioned tests amounted to 2,381.77 €. Total cost amounted to 21,435.97 € (Table II).
At the Hospital de Cabueñes, the cost of laparoscopic cholecystectomy performed by the General and Digestive Surgery Department, with a mean stay of 5.1 days, amounted to 3,012.50 € per patient.
Discussion
The goal of our study was to analyze the readmission of patients with acute edematous pancreatitis (ABEP) without cholecystectomy after an initial admission due to ABEP or lithiasic cholecystitis at least two weeks before. During the study period of 4 months, 9 patients suffered from recurrent ABEP due to the fact that an early cholecystectomy was not performed during initial admission or due to a late cholecystectomy in the following 2-4 weeks. At the Hospital de Cabueñes, recurrent ABEP represents around 25% of gallstone pancreatitis which requires hospital admission; during the referred period, 9 patients with recurrent ABEP and 27 cases of AGSP were admitted.
The median number of days from the previous ABEP episode or lithiasic cholecystitis to readmission for recurrent ABEP was 114 days (IQR = 111.0), and 207 days (IQR = 114.0) for cholecystectomy.
Cholecystectomy is the definitive treatment for AGSP, preventing its recurrence (10). Laparoscopic surgery is the preferred method for cholecystectomy. The time until performing laparoscopic cholecystectomy after a mild ABEP episode has changed in the last years (11). Historically, it was recommended to delay cholecystectomy at least 6-8 weeks after an attack of acute pancreatitis to help to reduce inflammation in the peripancreatic area (12). In the current clinical practice, many surgeons postpone cholecystectomy at least 6 weeks due to a perceived more difficult and risky intervention during the first weeks after an acute pancreatitis episode as well as for logistic reasons (13). This is the procedure followed at our hospital, where all patients with AGSP and/or recurrent ABEP are discharged without performing an early cholecystectomy during hospitalization.
There is no universally accepted definition of the time interval over which laparoscopic cholecystectomy can be considered to be early. In the case of mild AGSP, UK guidelines for the management of acute pancreatitis (14), systematic reviews (1,11) and controlled randomized clinical tests such as the one conducted in Los Angeles by Aboulian et al. (10) recommend the performance of laparoscopic cholecystectomy during the first three days after the onset of symptoms (11,14) or even within the first 48 hours of hospital admission (1,10). A 3-day period will allow the clinician to differentiate mild pancreatitis from severe pancreatitis as in most cases clinical deterioration happens during the first 48 hours (15). Furthermore, taking into account that up to 20% of patients could have choledocholithiasis, this period of time would enable them to perform MRCP to exclude choledocholithiasis when there are reasonable doubts.
There is no consensus on the best approach for patients with choledocholithiasis in laparoscopic cholecystectomies. In a randomized study that compares early cholecystectomy during admission and late cholecystectomy after hospital discharge, Aboulian et al. performed an intraoperative cholangiography in patients with suspected choledocholithiasis, extracting lithiasis after surgery by ERCP with sphincterotomy (10).
Several studies show that early cholecystectomy is safe when compared to late cholecystectomy that is performed after three days of hospitalization but usually before 2-4 weeks (1,10,11,14). Early laparoscopic cholecystectomy may shorten hospital stays, and no differences were observed regarding switching from laparoscopy to an open procedure or perioperative complications (10,11).
Taylor et al. compared two groups of patients with mild gallstone pancreatitis: in one group cholecystectomy was performed when abdominal exploration had improved and pancreatic enzymes had decreased; in the other group cholecystectomy was not performed until a complete normalization of enzymes and abdominal exploration. The study showed that it is safe to perform cholecystectomy in the first group, with no difference in the surgery complication rate of both groups (16). The study of Aboulian et al. has reached similar conclusions, proving that early laparoscopic cholecystectomy in patients with mild ABEP, regardless of pain or pancreatic enzymes elevation, shortens hospital stays and has no apparent impact on the technical difficulty of the procedure or the increase of perioperative complications (10).
The results of a randomized controlled trial have been recently published. The PONCHO trial (pancreatitis of biliary origin, optimal timing of cholecystectomy) was designed to study whether early laparoscopic cholecystectomy reduces mortality and readmissions due to biliary complications when compared to delayed cholecystectomy (13). In this multicenter trial, 266 inpatients with AGSP were randomly assigned to same-admission cholecystectomy within 3 days of randomization, or to discharge and the performance of cholecystectomy after 25-30 days of randomization. AGSP patients aged 18 to 75 with an ASA I-III physical status were assessed for eligibility. They were randomized when hospital discharge was expected within the next 48 hours, that is, when they could tolerate a normal oral diet, there was no need for analgesics, and C-reactive protein concentration was < 100 mg/L. Readmission due to gallstone-related complications occurred in 17% of patients in the group without same-admission surgery and in 5% of patients in the group with same-admission surgery (p = 0.002). There were no differences between both groups in terms of surgery difficulty, switch to open cholecystectomy, surgery time or average hospital stay after the intervention. There was also no difference between the groups in terms of the complication rate during cholecystectomy. Safety endpoints occurred in four patients: one case of bile duct leakage and one case of postoperative bleeding in each group. The PONCHO study shows that same-admission cholecystectomy reduces recurrent biliary complications in mild AGSP and does not increase surgery complications (17).
In the case of mild ABEP, UK guidelines for the management of acute pancreatitis recommend surgery within two weeks after admission (14). A delay of more than 4 weeks in the laparoscopic cholecystectomy after the first episode of ABEP is associated with readmission due to biliary complications as pancreatitis, cholecystitis or biliary colic. In our series, cholecystectomy had not been performed on patients although a median of 114 days (IQR = 111.0) had passed since the initial admission.
In the case of severe or necrotizing acute pancreatitis, a greater emphasis has to be placed on the management of systemic and local complications. Surgery in these patients should be more conservative. There is no evidence that early cholecystectomy in these patients is useful. In fact, several initial studies showing high morbidity of early cholecystectomy in patients with pancreatitis derive from the significant proportion of peripancreatic or hemorrhagic necrosis in this series (18,19).
A second episode of recurrent acute pancreatitis is not exempt from the risks for the patient, and successive episodes of recurrent pancreatitis increase by up to 10% the risk of chronic pancreatitis (20). In our study, there were no reports of evolution from ABEP to severe pancreatitis. There were no deaths during hospitalization.
Acute pancreatitis involves health costs and indirect social costs as a result of sick leave of patients during hospitalization and recovery. Most of the expenses are due to hospitalization but the cost of the loss of work days adds an unnecessary economic burden that should be taken into account (21).
There are few analyses of the costs associated with pancreatitis; most of them were undertaken in Sweden. In 2010, the group Andersson et al. published several long-term prospective studies focused on the evolution of endocrine and exocrine pancreatic function, quality of life and health costs associated with acute pancreatitis. Patients with severe pancreatitis incurred higher health costs due to a longer hospital stay, follow-up after hospital discharge and late complications (22). In Japan, Murata et al. highlighted that the factors that increase admission costs of patients with acute pancreatitis are complex treatments such as necrosectomy or intensive care in case of severe pancreatitis (23). At present, due to the scarce number of studies about associated costs (21) there are few data concerning expenses arising from early or delayed cholecystectomy, and there are no studies that include the loss of work days in the costs (11). A retrospective study done in one center showed that cholecystectomy performed within the first two weeks does not increase costs as compared to late cholecystectomy (24).
In our study, all patients admitted with recurrent ABEP were eligible for cholecystectomy. The mean age of patients in our study was 65.3 years (SD = 19.2) (range 30-84) and none of them had been dismissed for surgery. Health costs linked to readmissions due to not performing early or late cholecystectomy was 2,381.77 € per patient during the period of study.
In conclusion, if after a first episode of ABEP or lithiasic cholecystitis cholecystectomy is not performed in an early or late interval according to the timing recommended by the guidelines, avoidable readmissions due to gallstone-related complications such as recurrent pancreatitis occur. These readmissions pose a risk of comorbidity and increase the risk of developing chronic pancreatitis. Avoidable costs associated with the illness such as emergency department costs, hospital stay and tests, during a four-month period, amounted to 21,435.97 €. If we extrapolate these costs to a one-year period, it would amount to 64,307.90 € of avoidable costs. Thus, the right moment to perform cholecystectomy in these patients needs to be reconsidered.
Our study presents some limitations. Although none of the patients had been readmitted due to biliary colic or cholecystitis, costs associated with the Emergency Department consultation without admission or Primary Care doctor visit are not taken into account. In addition, this study analyzes patients of only one center and it is not possible to compare it to other centers. Ultimately, stronger evidence of costs-overrun linked to the non-performance of cholecystectomy within 2-4 weeks after initial admission for mild AGSP would require a randomized controlled trial. The ability to extrapolate from these results is limited, and consequently the external validity of the study is also limited as protocols and routine clinical practice regarding costs associated to the non-performance of cholecystectomy vary in the different hospitals.
Acknowledgements
To all medical staff, nursing staff and assistants who work in the Department of Digestive Diseases at the Hospital de Cabueñes (Gijón, Spain), for their help and support.
References
1. Cucher D, Kulvatunyou N, Green DJ, et al. Gallstone pancreatitis: a review. Surg Clin North Am 2014;94(2):257-80. DOI: 10.1016/j.suc.2014.01.006. [ Links ]
2. Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis - 2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62(1):102-11. DOI: 10.1136/gutjnl-2012-302779. [ Links ]
3. Lankisch PG, Apte M, Banks PA. Acute pancreatitis. Lancet 2015;386(9988):85-96. DOI: 10.1016/S0140-6736(14)60649-8. [ Links ]
4. Randial Perez LJ, Fernando Parra J, Aldana Dimas G. The safety of early laparoscopic cholecystectomy (48 hours) for patients with mild gallstone pancreatitis: a systematic review of the literature and meta-analysis. Cir Esp 2014;92(2):107-13. [ Links ]
5. Wilson CT, de Moya MA. Cholecystectomy for acute gallstone pancreatitis: early vs delayed approach. Scand J Surg 2010;99(2):81-5. [ Links ]
6. Morris S, Gurusamy KS, Patel N, et al. Cost-effectiveness of early laparoscopic cholecystectomy for mild acute gallstone pancreatitis. Br J Surg 2014;101(7):828-35. DOI: 10.1002/bjs.9501. [ Links ]
7. Nebiker CA, Frey DM, Hamel CT, et al. Early versus delayed cholecystectomy in patients with biliary acute pancreatitis. Surgery 2009;145(3):260-4. DOI: 10.1016/j.surg.2008.10.012. [ Links ]
8. Tenner S, Baillie J, DeWitt J, et al. American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 2013;108(9):1400-15; 16. DOI: 10.1038/ajg.2013.218. [ Links ]
9. Navarro S, Amador J, Arguello L, et al. Recommendations of the Spanish Biliopancreatic Club for the Treatment of Acute Pancreatitis. Consensus development conference. Gastroenterol Hepatol 2008;31(6):366-87. [ Links ]
10. Aboulian A, Chan T, Yaghoubian A, et al. Early cholecystectomy safely decreases hospital stay in patients with mild gallstone pancreatitis: a randomized prospective study. Ann Surg 2010;251(4):615-9. DOI: 10.1097/SLA.0b013e3181c38f1f. [ Links ]
11. Gurusamy KS, Nagendran M, Davidson BR. Early versus delayed laparoscopic cholecystectomy for acute gallstone pancreatitis. Cochrane Database Syst Rev 2013;9:CD010326. [ Links ]
12. Pellegrini CA. Surgery for gallstone pancreatitis. Am J Surg 1993;165(4):515-8. DOI: 10.1016/S0002-9610(05)80952-3. [ Links ]
13. Bouwense SA, Besselink MG, van Brunschot S, et al. Pancreatitis of biliary origin, optimal timing of cholecystectomy (PONCHO trial): study protocol for a randomized controlled trial. Trials 2012;13:225. DOI: 10.1186/1745-6215-13-225. [ Links ]
14. UK guidelines for the management of acute pancreatitis. Gut 2005;54(Supl. 3):iii1-9. [ Links ]
15. Ranson JH, Pasternack BS. Statistical methods for quantifying the severity of clinical acute pancreatitis. J Surg Res 1977;22(2):79-91. DOI: 10.1016/0022-4804(77)90045-2. [ Links ]
16. Taylor E, Wong C. The optimal timing of laparoscopic cholecystectomy in mild gallstone pancreatitis. Am Surg 2004;70(11):971-5. [ Links ]
17. da Costa DW, Bouwense SA, Schepers NJ, et al. Same-admission versus interval cholecystectomy for mild gallstone pancreatitis (PONCHO): a multicentre randomised controlled trial. Lancet 2015;386(10000):1261-8. DOI: 10.1016/S0140-6736(15)00274-3. [ Links ]
18. Delorio AV Jr, Vitale GC, Reynolds M, et al. Acute biliary pancreatitis. The roles of laparoscopic cholecystectomy and endoscopic retrograde cholangiopancreatography. Surg Endosc 1995;9(4):392-6. [ Links ]
19. Kelly TR, Wagner DS. Gallstone pancreatitis: a prospective randomized trial of the timing of surgery. Surgery 1988;104(4):600-5. [ Links ]
20. Lankisch PG, Bruns A, Doobe C, et al. The second attack of acute pancreatitis is not harmless. Pancreas 2008;36(2):207-8. DOI: 10.1097/MPA.0b013e318157b11d. [ Links ]
21. Andersson B, Appelgren B, Sjodin V, et al. Acute pancreatitis--costs for healthcare and loss of production. Scand J Gastroenterol 2013;48(12):1459-65. DOI: 10.3109/00365521.2013.843201. [ Links ]
22. Andersson B, Pendse ML, Andersson R. Pancreatic function, quality of life and costs at long-term follow-up after acute pancreatitis. World J Gastroenterol 2010;16(39):4944-51. DOI: 10.3748/wjg.v16.i39.4944. [ Links ]
23. Murata A, Matsuda S, Mayumi T, et al. Multivariate analysis of factors influencing medical costs of acute pancreatitis hospitalizations based on a national administrative database. Dig Liver Dis 2012;44(2):143-8. DOI: 10.1016/j.dld.2011.08.011. [ Links ]
24. Monkhouse SJ, Court EL, Dash I, et al. Two-week target for laparoscopic cholecystectomy following gallstone pancreatitis is achievable and cost neutral. Br J Surg 2009;96(7):751-5. DOI: 10.1002/bjs.6644. [ Links ]
![]() Correspondence:
Correspondence:
Eva Barreiro Alonso.
Department of Digestive Diseases.
Hospital de Cabueñes.
C/ de los Prados, 395. 33394 Gijón, Asturias
e-mail: evabarreiroalonso@yahoo.es
Received: 28-10-2015
Accepted: 02-05-2016











 texto en
texto en