My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.8 Madrid Aug. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Gastric necrosis secondary to strangulated giant paraesophagic hiatal hernia
Necrosis gástrica secundaria a hernia hiatal gigante paraesofágica estrangulada
José Ángel Díez-Ares, Nuria Peris-Tomás, Nuria Estellés-Vidagany and Dolores Periáñez-Gómez
Department of General and Digestive Surgery. Hospital Doctor Peset. Valencia, Spain
Introduction
Asymptomatic giant hiatal hernia comprises a relatively common disease, mostly presented in women at the age of 50 and older. The therapeutic approach remains controversial in recent years.
Case report
A 67-year-old woman with a medical history of morbid obesity, type 2 diabetes mellitus, arterial hypertension, dyslipemia, and an asymptomatic hiatal hernia is admitted to our hospital owing to thoracic and abdominal pain, which has been related to food intake for 6 months. The patient presents a clear worsening in the last 48 hours, with no other associated symptomatology. With the suspected diagnosis of acute pancreatitis, the patient is admitted to the Digestive Service.
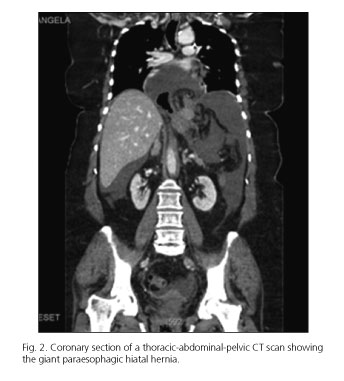
Twenty four hours after admission, the patient presents an overall worsening, with hypotension, tachycardia and profuse sweating. The CT scan shows a hiatal hernia with a mesentero-axial stomach volvulus inside. Gas and abundant periesophageal liquid are also observed. These findings are compatible with the diagnosis of an incarcerated and ischemic paraesophagic hiatal hernia with a stomach perforation (Fig. 1).
CT scan also shows moderate amount of perihepatic, perisplenic liquid (Fig. 2). Suspecting an incarcerated hiatal hernia with stomach perforation, the patient is taken to the operating room for a laparotomy during the early hours.
An atypical gastrectomy of the greater curvature with a gastropexy is performed along with fixation to the anterior abdominal wall. Surgery is completed with a feeding jejunostomy.
During the postoperative period, the patient has a mediastinal collection, which is treated conservatively with antibiotics. The patient is discharged after 12 days.
Discussion
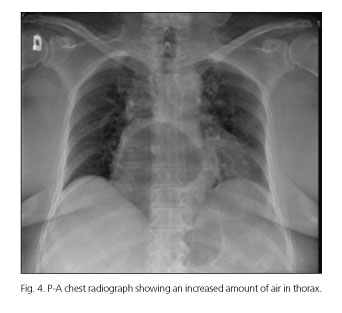
Gas-filled viscus in the lower chest or upper abdomen on chest radiograph is diagnostic of a paraesophagic hernia. In our case, we also objectified a progressive air increase inside the herniated stomach (Figs. 3 and 4). These findings support the suspected incarceration.
At present, upper endoscopy is the most sensitive and specific technique for this kind of disease.
CT findings make the diagnosis clear and can be very important in establishing the diagnosis when a clinician is aware of the severity of the presentation.
Hiatal hernia emergency surgery technique is actually not still clearly established.
References
1. Skinner DB, Belsey RH. Surgical management of esophageal reflux and hiatus hernia. Long-term results with 1,030 patients. J Thorac Cardiovasc Surg 1967;53:33-54. [ Links ]
2. Granderath FA, Schweiger UM, Kamolz T, et al. Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: Preliminary results of a prospective randomized functional and clinical study. Arch Surg 2005;140:40-8. DOI: 10.1001/archsurg.140.1.40. [ Links ]
3. Oelschlager BK, Pellegrini CA, Hunter J, et al. Biologic prosthesis reduces recurrence after laparoscopic paraesophageal hernia repair: A multicenter, prospective, randomized trial. Ann Surg 2006;244:481-90. DOI: 10.1097/01.sla.0000237759.42831.03. [ Links ]
4. Kohn GP, Price RR, DeMeester SR, et al. Guidelines for the management of hiatal hernia. Surg Endosc 2013;27:4409-28. DOI: 10.1007/s00464-013-3173-3. [ Links ]
5. Hill LD. Incarcerated paraesophageal hernia. A surgical emergency. Am J Surg 1973;126:286-91. DOI: 10.1016/S0002-9610(73)80165-5. [ Links ]











 text in
text in