My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.10 Madrid Oct. 2016
https://dx.doi.org/10.17235/reed.2016.3823/2015
CASE REPORTS
Endoscopic resection of rectal granular-cell tumor using elastic band ligation
Resección endoscópica mediante banda elástica de tumor rectal de células granulares
Sergio Sevilla-Ribota1, Javier Pérez-Bedmar-Delgado1, Juan José Domínguez-Cañete2, Ana María Dotor-de-Lama2 and Mariano Gómez-Rubio1
Departments of 1 Digestive Diseases and
2 Pathology. Hospital Universitario de Getafe. Getafe, Madrid. Spain
ABSTRACT
Granular cell tumor (GCT) is a rare neoplasm that develops in the gut's submucosal layer.
We report the case of a male with a history of surgically excised colon neoplasm where a rectal polyp was identified during a follow-up endoscopy. The lesion, eventually identified as a GCT, was endoscopically removed by band ligation-assisted mucosectomy.
This may be the second report of a colorectal GCT successfully managed using band ligation, and the first one on a rectal GCT excised with this technique.
Key words: Colonoscopy. Rectum. Granular cell tumor. Submucosal tumor of the colon. Endoscopic mucosal resection.
RESUMEN
El tumor de células granulares (TCG) es un tumor raro que se localiza en la capa submucosa del tubo digestivo.
Presentamos a continuación a un varón con antecedentes de neoplasia de colon extirpada mediante cirugía en el que durante una colonoscopia de control se identificó un pólipo en el recto que extirpamos endoscópicamente realizando una mucosectomia asistida con banda elástica, resultando ser un TCG.
Estamos ante lo que puede ser la segunda publicación de un TCG colorrectal tratado con éxito mediante banda elástica y el primer caso de TCG extirpado en el recto con esta técnica.
Palabras clave: Colonoscopia. Recto. Tumor de células granulares. Tumor submucoso del colon. Resección mucosa endoscópica.
Introduction
Granular cell tumor, also referred to as Abrikossoff's tumor, should be included in the diagnostic pool of submucosal lesions in the gut (1). This is an uncommon subepithelial tumor with low malignant potential that is usually located in other body areas, uncommon in the GI tract. It usually develops in the distal esophagus, but rectal cases are rare. It is usually asymptomatic and incidentally diagnosed during routine endoscopic procedures as in our patient (2). Its multifocal, synchronous and metachronous character must be borne in mind as well as its malignant potential, which will inform its subsequent management.
Case Report
A 59-year-old male, who smoked 15 cigarettes a day, drank a glass of wine during meals and had no remarkable personal or family history regarding tumors underwent laparoscopy and left hemicolectomy for colonic adenocarcinoma in 2009, followed by adjuvant chemotherapy, which resulted in complete remission as ascertained by yearly follow-up CT scans and colonoscopies. The last CT scan revealed no space-occupying lesions in other abdominal organs, and no mesenteric or retroperitoneal adenopathies. However, colonoscopy identified a normal surgical anastomosis at 15 cm from the anal margin, and an immobile sessile rectal polyp at 10 cm from the anal margin; the latter was 8 mm in diameter and soft, and had a regular surface and contour consistent with a submucosal lesion (Fig. 1). Given its morphological and structural characteristics, resection by band ligation-assisted mucosectomy was decided on during the ongoing procedure (Fig. 2). The technique was successful and a fine-looking post-polypectomy scar was obtained (Fig. 3), with no complications arising either during the procedure or afterwards.
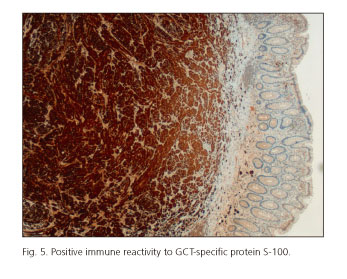
Under the microscope a nodular submucosal lesion was seen comprised of fusiform and polygonal cells with ovoid nuclei without atypia or mitotic activity, and extended cytoplasms containing PAS+ granules, all of which was consistent with a histological diagnosis of GCT without malignancy criteria (3-5). Resection margins were reported as complete (Fig. 4), and immune reactivity to protein S-100 enhanced diagnostic specificity (Fig. 5).
The patient was later studied with upper GI endoscopy. Esophagogastroduodenoscopy revealed no polypoid lesions. Mild erosive bulbitis and chronic antral gastritis were identified. Biopsy samples were obtained from the antrum, which confirmed chronic gastritis, and urease testing for H. pylori was positive. Regarding the oral cavity, the patient had no oral or tongue lesions, and dermatological examination identified no changes or nodules.
Discussion
GCT is a rare uncommon growth that may develop in many tissues. It is mainly located in the oral cavity (particularly the tongue), the skin (predominating in the head and neck), the musculoskeletal system, and the breasts. Although less frequently (8% of all GCTs), it may develop anywhere along the GI tract, and cases have been reported from the upper esophageal sphincter to the anal canal (6). The distal esophagus is the most common site in up to one third of patients. Then follows the colorectal segment, particularly the cecum and ascending colon, with the rectum being a rare location (2). As far as we know, only one case is reported in the literature of resection with our endoscopic method of a sigmoid lesion (3). Rare cases have been reported in the stomach and bile tree, exceptionally in the duodenum and pancreas (7,8).
This tumor is predominant among females, in the fourth or fifth decade of life, and in the black population. In contrast to its classical myogenic etiology, the latest etiopathogenic theories posit an origin peripheral nerve cells (Schwann cells) given the presence of protein S-100 and other neuron-specific proteins when using immunohistochemical staining techniques such as the myeloprotein or neuron-specific enolase tests (2,4).
Due to the increased number of GI studies that our specialty has experienced in the last decade, the diagnosis of this condition has increased. It is usually a symptom-free condition unveiled by routine endoscopic procedures. The sparse manifestations reported include nonspecific abdominal pain and exceptionally GI bleeding (3).
Standard endoscopy shows submucosal polypoid lesions, usually smaller than 2 cm and yellowish-white in color. Endoscopic endosonography may assess the layer involved and tumor extension. It usually behaves in a hardly invasive manner not extending outside the gut wall's muscular layer. In 95% of cases the tumor is seen as a solid lesion with regular margins originating in the second (hypoechoic) or third (hyperechoic) layer (9). In our patient we decided not to extend the endoscopic exam using ultrasounds since the lesion's anatomical and morphological characteristics led us to suspect a rectal carcinoid tumor. Echoendoscopy is not mandatory for rectal carcinoid tumors smaller than 1 cm in diameter since a high percentage never invade the muscularis propria (10). Furthermore, we also relied on previous tests, which showed no local invasion, nodal involvement or distant spread findings. However, the best method to characterize gastrointestinal subepithelial lesions is endoscopic ultrasonography, which should be used whenever possible (1).
Given its ubiquitous nature, we must bear in mind that between 10% and 20% of GCT cases exhibit a multifocal origin along the gut, which should prompt a thorough endoscopic examination of the whole GI tract (8,11). While abdominal ultrasounds seem a reasonable addition, they were not used for our patient since previous CT scans revealed no biliary or pancreatic changes. Most recent literature reports tend to highlight the synchronous nature of this tumor with respect to other extradigestive involvement signs (12). We underscore the relevance of proper history taking and physical examination most particularly regarding the ENT, dermatological and gynecological areas, which were not involved in our patient.
Despite its scarcely malignant nature (1-2%), an extension study and clinical as well as endoscopic follow-up are always advisable as GCT displays a metachronous behavior with 5% to 10% recurrences following resection. Lateral and deep margins should be assessed in order to prevent recurrence (11). Malignancy criteria to be considered include size greater than 4 cm, rapid tumor growth, and presence of local or distant spread (13). Closer clinical follow-up is recommended for patients with positive malignancy criteria (11).
Endoscopic resection is the modality of choice for lesions smaller than 2 cm not invading the muscularis propria layer; lesions larger than 4 cm and multifocal tumors should be managed surgically (2). The endoscopic technique we used, assisted by elastic band ligation, is user friendly and provides a number of benefits. On the one hand, margin resection is clear as the plastic cap allows improved polyp edge delimitation and favors complete resection. On the other hand, the technique has been shown to induce an exceptional rate of serious complications, including perforation (3,14).
References
1. http://www.elsevier.es/es-revista-endoscopia-335-articulo-papel-del-ultrasonido-endoscopico-el-90192517. [ Links ]
2. Brambilla E, Antonio M, Rasia H, et al. Granular cell tumor of colon: A case report. J Coloproctol 2012;32:193-5. DOI: 10.1590/S2237-93632012000200017. [ Links ]
3. Endo S, Hirasaki S, Doi T, et al. Granular cell tumor occurring in the sigmoid colon treated by endoscopic mucosal resection using a transparent cap (EMR-C). J Gastroenterol 2003;38:385-9. DOI: 10.1007/s005350300068. [ Links ]
4. http://www.wjgnet.com/1007-9327/10/2452.pdf. [ Links ]
5. http://imsear.li.mahidol.ac.th/bitstream/123456789/143163/1/tg2011v32n3p242.pdf. [ Links ]
6. Santoni B, Pinto F, Machado L, et al. Tumor de células granulares no canal anal: relato de caso e revisão de literatura. Rev Bras Coloproct 2006;26:454-8. DOI: 10.1590/S0101-98802006000400014. [ Links ]
7. Franco C, Rodrigo P, Freddy C, et al. Ictericia obstructiva secundaria a tumor de células granulares de la vía biliar extrahepática. Rev Chilena de Cirugía 2011;63:627-30. DOI: 10.4067/S0718-40262011000600014. [ Links ]
8. Vicente Cantero M, Martín Díaz L, Martínez Barba E, et al. Tumor de células granulares multicéntrico del aparato digestivo. Cir Esp 2004;76:331-2. DOI: 10.1016/S0009-739X(04)72386-6. [ Links ]
9. http://www.scielo.org.co/pdf/rcg/v20n2/v20n2a09.pdf. [ Links ]
10. Scherübl H, Jensen R, Cadiot G, et al. Management of early gastrointestinal neuroendocrine neoplasms. World J Gastrointest Endosc 2011;3:133-9. DOI: 10.4253/wjge.v3.i7.133. [ Links ]
11. Znati K, Harmouch T, Benlemlih A, et al. Solitary granular cell tumor of cecum: A case report. ISRN Gastroenterol 2011;2011:943804. DOI: 10.5402/2011/943804. [ Links ]
12. Kocatas A, Dural A, Sever N, et al. Minimal invasive endoscopic management of synchronous granular cell tumours in the colon and posterior mediastinum. J Min Access Surg 2014;10:34-6. DOI: 10.4103/0972-9941.124469. [ Links ]
13. Choi S, Hong S, Kang S, et al. A case of malignant granular cell tumor in the sigmoid colon. Clin Endosc 2014;47:197-200. DOI: 10.5946/ce.2014.47.2.197. [ Links ]
14. Ono A, Fujii T, Saito Y, et al. Endoscopic submucosal resection of rectal carcinoid tumors with a ligation device. Gastrointest Endosc 2003;57:583-7. DOI: 10.1067/mge.2003.142. [ Links ]
![]() Correspondence:
Correspondence:
Sergio Sevilla-Ribota.
Departmet of Digestive Diseases.
Hospital Universitario de Getafe.
Ctra. de Toledo, km. 12.5.
28905 Getafe, Madrid. Spain.
e-mail: s.sevilla.ribota@gmail.com
Received: 28-04-2015
Accepted: 20-08-2015











 text in
text in