My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.11 Madrid Nov. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Endoscopic management of late complication of blunt traumatic total pancreatic transection
João Santos-Antunes, Pedro Moutinho-Ribeiro and Guilherme Macedo
Department of Gastroenterology. Faculty of Medicine. Centro Hospitalar S. João. Porto, Portugal
Case Report
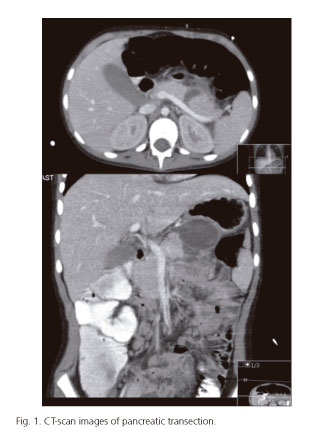
An 11-year-old girl was admitted elsewhere due to severe abdominal pain after a fall with abdominal blunt trauma. CT-scan showed total pancreatic transection of the distal body with suspected injury of main pancreatic duct (Fig. 1). Conservative approach with antibiotics and total parenteral nutrition was decided due to her clinical stability. On day 12, she deteriorated clinically; ultrasound showed an 8 cm pseudocyst that was percutaneously drained. Initially she improved, but on day 37 she developed alimentary intolerance, and on day 55 she was referred to us with septic shock, to perform endoscopic drainage, under piperacillin/tazobactam.
During endoscopic ultrasound, a 5 cm anechoic lesion (Fig. 2) was found in the distal pancreatic body. Transgastric puncture was performed and, over a guide-wire, the fistula was created with a cystotome, followed by balloon dilation (Fig. 3). Two 7 Fr double pigtail stents were placed (Fig. 4). Fluid and blood cultures were positive for Pseudomonas aeruginosa, and amikacin was added.
She had a favourable evolution, starting oral feeding 5 days later, and was discharged asymptomatic after two weeks. Six months later, MRI showed no signs of pancreatic lesion.
Discussion
Immediate management of blunt traumatic pancreatic transection is controversial, since the literature is based on case reports or series. Previous reports showed good outcomes with endoscopic, surgical treatment and even with conservative management in clinically stable patients (1,2).
Management of late complications are even rarely described (3). Clinical deterioration with septic shock demanded undoubtedly an aggressive treatment, with cystogastrostomy, percutaneous drainage or laparotomy. In our case, a minimally invasive approach was decided, with an excellent outcome.
References
1. Iqbal CW, St Peter SD, Tsao K, et al. Operative vs nonoperative management for blunt pancreatic transection in children: Multi-institutional outcomes. J Am Coll Surg 2014;218:157-62. DOI: 10.1016/j.jamcollsurg.2013.10.012. [ Links ]
2. Hamidian Jahromi A, D'Agostino HR, Zibari GB, et al. Surgical versus nonsurgical management of traumatic major pancreatic duct transection: Institutional experience and review of the literature. Pancreas 2013;42:76-87. DOI: 10.1097/MPA.0b013e3182575cf9. [ Links ]
3. Wales PW, Shuckett B, Kim PC. Long-term outcome after nonoperative management of complete traumatic pancreatic transection in children. J Pediatr Surg 2001;36:823-7. DOI: 10.1053/jpsu.2001.22970. [ Links ]