Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.12 Madrid dic. 2016
PICTURES IN DIGESTIVE PATHOLOGY
A diffusely enlarged pancreas: the (un)usual suspect
Pedro Magalhães-Costa1, Maria José Brito2 and Pedro Pinto-Marques3
1Department of Gastroenterology. Hospital Egas Moniz. Lisbon, Portugal.
2Department of Pathology. Hospital Garcia de Orta. Lisbon, Portugal.
3Department of Gastroenterology. Hospital Garcia de Orta. Lisbon, Portugal
Case report
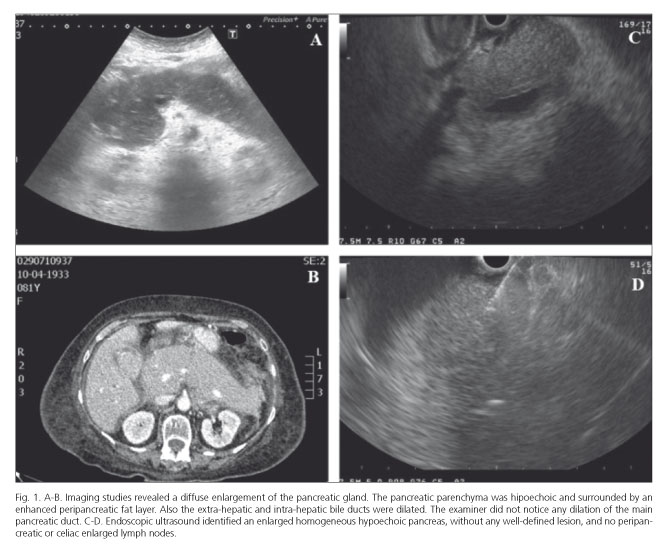
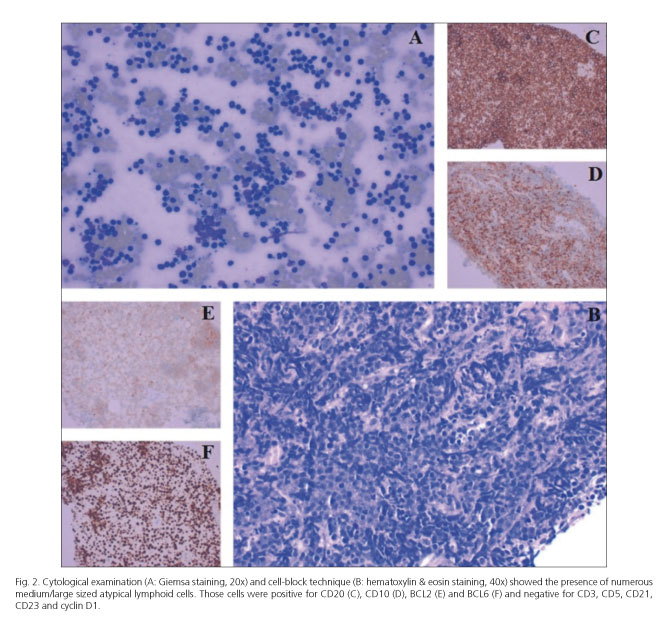
An 81-year-old female presented with obstructive jaundice and a non-specific clinical picture of nausea and appetite loss. Labs demonstrated a conjugated hyperbilirubinemia (7.7 mg/dL), increased aspartate aminotransferase and alanine aminotransferase (10x ULN and 8x ULN, respectively), increased lactate dehydrogenase (10x ULN) and serum lipase (3x ULN). CA 19.9 was 342 U/mL (ref. value < 37 U/mL). There was no evidence of peripheral lymphadenopathy or hepatosplenomegaly. Imaging (Fig. 1 A and B) revealed a marked homogeneous enlargement of the pancreas (without any well-defined mass), dilation of the extra and intra-hepatic bile ducts and ascites. Endoscopic ultrasound (Fig. 1 C and D) identified an enlarged homogeneous hypoechoic pancreas, without any well-defined lesion, no dilation of the main pancreatic duct, and no peripancreatic or celiac enlarged lymph nodes. A fine-needle biopsy was performed yielding, on cytological examination and cell-block technique (Fig. 2 A and B), numerous medium/large sized atypical lymphoid cells that displayed a B-cell lineage immunophenotype (Fig. 2 A-F). Even though further characterization (by flow cytometric immunophenotyping) could not be obtained, a final diagnosis of primary pancreatic lymphoma (PPL) was assumed.
Discussion
Primary pancreatic lymphoma is a remarkably rare tumor of the pancreas, representing approximately 0.5% of all pancreatic neoplasms and < 2% of all lymphomas (1,2). A correct diagnosis is crucial because therapeutic management differs from other pancreatic malignancies (pancreatic ductal adenocarcinoma, neuroendocrine tumor and metastases) (2,3). Two morphologic patterns of PPL are recognized: a focal form (occurring in the pancreatic head in 80% of cases) and a rarer diffuse/infiltrative pattern, as depicted herein, emulating an acute/autoimmune pancreatitis (1).
References
1. Battula N, Srinivasan P, Prachalias A, et al. Primary pancreatic lymphoma: Diagnostic and therapeutic dilemma. Pancreas 2006;33:192-4. DOI: 10.1097/01.mpa.0000227910.63579.15. [ Links ]
2. Du X, Zhao Y, Zhang T, et al. Primary pancreatic lymphoma: A clinical quandary of diagnosis and treatment. Pancreas 2011;40:30-6. DOI: 10.1097/MPA.0b013e3181e6e3e5. [ Links ]
3. Iglesias García J, Lariño Noia J, Domingues Muñoz JE. Endoscopic ultrasound in the diagnosis and staging of pancreatic cancer. Rev Esp Enferm Dig 2009;101:631-8. DOI: 10.4321/S1130-01082009000900006. [ Links ]