My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 n.12 Madrid Dec. 2016
https://dx.doi.org/10.17235/reed.2016.4121/2015
Hybrid treatment of dysphagia lusoria: right carotid to subclavian bypass and endovascular insertion of an Amplatzer II Vascular Plug
Ernesto Cobos-González1, José Arturo Aragón-López2, Ricardo García-Buen-Abad3, José A. Rojas4 and Abraham Gutiérrez5
1Division of Vascular Surgery. Centro Especializado en Diabetes.
2Division of General Surgery, 3Department of Radiology and Molecular Imaging, 4Division of Internal Medicine, and 5Division of Anesthesiology. The American British Cowdray Medical Center. Mexico City, Mexico
ABSTRACT
Compression of the esophagus by a retroesophageal aberrant right subclavian artery (ARSA) is a rare cause of dysphagia. We present the case of a 47-year-old female with symptoms of progressive dysphagia diagnosed with dysphagia lusoria using barium swallow and contrast computed tomography and successfully treated with a hybrid procedure: right carotid to subclavian bypass and endovascular insertion of an Amplatzer II Vascular Plug through the right superficial femoral artery. We consider this approach safer, less invasive and more complete to avoid recurrent dysphagia.
Key words: Dysphagia. Lusoria. Aberrant. Subclavian. Endovascular. Hybrid.
Introducción
Difficulty swallowing caused by compression of the esophagus by a retroesophageal aberrant right subclavian artery (ARSA) is termed dysphagia lusoria and constitutes a rare cause of dysphagia. Originally named by Bayford in 1795 in reference to "lusus naturae" (freaks of nature) (1) and first treated surgically by Gross in 1964 (2), the condition is of elusive diagnosis and controversial management. Patients often have seen several physicians before diagnosis and treatment are achieved. Recent endovascular advances have allowed for safer, less invasive management (3,4).
Case report
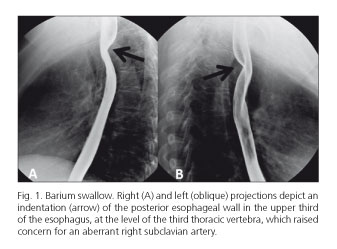
A 47-year-old female with history of diabetes and hypertension was sent to the Vascular Surgery Office from the Gastroenterology Service, where she had been seen for progressive dysphagia for approximately nine months. Initial symptoms related only to solid food progressed to dysphagia to liquids and accumulation of secretions in upper digestive tract and choke sensation during nights that interfered with her sleep and caused growing anxiety. The patient also mentioned weight loss of approximately 5 kg in this period of time. Physical examination did not reveal significant findings. Endoscopy of the esophagus, stomach and duodenum and esophageal manometry only found moderate esophagitis. A six-week course of proton pump inhibitors and pro-kinetic drugs did not modify her symptoms. A barium swallow was then performed (Fig. 1). The finding of an indentation at the level of the third thoracic vertebra gave the first clue to her diagnosis. Her imaging was completed with a contrast computed tomography (CT) of the neck and chest (Fig. 2). The presence of a bicarotid trunk and a retroesophageal ARSA compressing the postero-lateral aspect of the esophagus confirmed the diagnosis of dysphagia lusoria. On arrival to our office, we offered a hybrid procedure to treat her condition. The patient accepted the procedure and underwent double clipping, division and oversewing of the ARSA (Figs. 3 A and B) and transposition to the right common carotid with an end-to-side anastomosis through a transverse right supraclavicular incision followed by angiogram and endovascular insertion of a 14 mm Amplatzer II Vascular Plug in the stump of the aberrant subclavian artery through right femoral artery puncture with a 9 F introducer (Fig. 3C). No complications occurred during the procedure. A chest X-ray in the recovery area showed elevation of the right hemidiaphragm that resulted from right phrenic nerve manipulation (Fig. 3D). This finding quickly improved with respiratory therapy during her hospital stay. The patient was discharged home on the sixth postoperative day with complete resolution of her dysphagia. One year after surgery, the patient is symptom free and has a normal right hemidiaphragm.
Discussion
Despite the fact that the aberrant artery causing dysphagia lusoria is of congenital origin, this condition frequently gives symptoms until the fourth or fifth decades in life. The reason for this late presentation is that vessels are soft and compliant in children and young adults, while later in life, especially in those with chronic conditions like diabetes and hypertension (as seen in our patient), arteries become rigid and even aneurysmal and may cause compression of a structure like the esophagus more easily (5). In the absence of an aneurysm of the aberrant artery, the combination of a bicarotid trunk anteriorly and a retroesophageal ARSA entrapping the esophagus (as seen in the present case) are believed to be associated to symptoms of dysphagia more frequently (5).
Concerns for ischemic complications prompted Hallman and Cooley to recommend arteriograms prior to aortic vascular ring repair in adults and flow re-establishment to the upper extremity after ligation of an aberrant subclavian artery (6). Cooley was first to anastomose the distal subclavian artery to the right common carotid artery (7). A number of authors have reported successfully treating cases of dysphagia lusoria only with division of the aberrant artery through a right supraclavicular incision and transposition of the subclavian artery to the carotid, with no intervention on the ARSA stump (8). We consider this an incomplete approach to this condition. The possibility of a patent stump causing persistent compression on the esophagus or the stump or distal aortic arch becoming aneurysmal with time and causing relapsing compression on the esophagus are risks that can be avoided with endovascular obliteration of the stump (3). In our opinion, removing systemic blood pressure from the stump of the ARSA (as with an Amplatzer occluder) is indispensable to avoid persistent or relapsing esophageal compression. The endovascular procedure to treat the stump is safe and minimally invasive. However, there is a risk for these rigid devices inside a vessel to erode their wall and cause esophageal fistula. Multiple reports have documented erosive complications with septal Amplatzer occluders in the heart, even years after their placement, with dire consequences (9). Only long term follow-up can determine the safety of these devices.
As in the case reported by Morris et al. (4), we also followed the recommendation of 50% oversizing of the Amplatzer II Vascular Plug to avoid migration, and also found it impossible to deploy the plug proximal to a retroesophageal position. Our patient reported immediate postoperative remission of her dysphagia and remains asymptomatic after one-year follow-up.
A recent report from New York described a brilliant technique of ligation of the ARSA at its origin in the distal aortic arch using a mediastinoscope through a right transverse supraclavicular incision prior to restoring arterial continuity by transposition of the ARSA to the ipsilateral common carotid artery (10). Although attractive, we consider the femoral endovascular approach to be safer than the insertion of a mediastinoscope over the aberrant vessel in the chest for the management of the stump.
Conclusions
The diagnosis of dysphagia lusoria may be elusive to the unwary eye. Barium swallow will suggest the diagnosis and contrast computed tomography or arteriogram will confirm the condition. Only mild cases will respond to medical treatment. Severe symptoms will only respond to surgical management. Ideal surgical treatment includes proximal ligation or endovascular exclusion of the aberrant vessel and re-establishment of arterial continuity to the right upper extremity. Only long term follow-up can rule-out complications or recurrence of symptoms associated to endovascular devices for proximal exclusion of the aberrant vessel.
References
1. Bayford D. An account of a singular case of obstructed deglutition. Memoirs Med Soc London 1794;2:275-86. [ Links ]
2. Gross RE. Surgical treatment of dysphagia lusoria. Ann Surg 1964;124:532-5. DOI: 10.1097/00000658-194609000-00008. [ Links ]
3. Shennib H, Diethrich EB. Novel approaches for the treatment of the aberrant right subclavian artery and its aneurysms. JVS 2008; 47:1066-70. [ Links ]
4. Morris ME, Benjamin M, Gardner GP, et al. The use of the Amplatzer Plug to treat dysphagia lusoria caused by an aberrant right subclavian artery. Ann Vasc Surg 2010;24:416e5-8. [ Links ]
5. Myers PO, Fasel JHD, Kalangos A, et al. Arteria lusoria: Developmental anatomy, clinical, radiological and surgical aspects. Ann Cardiol Angeiol (Paris) 2010;59:147-54. DOI: 10.1016/j.ancard.2009.07.008. [ Links ]
6. Hallman GL, Cooley DA. Congenital aortic vascular ring: Surgical considerations. Arch Surg 1964;88:666-75. DOI: 10.1001/archsurg.1964.01310220156024. [ Links ]
7. Cooley DA. Surgical treatment of aortic aneurysms. Philadelphia: WB Saunders; 1986. p. 175-84. [ Links ]
8. Carrizo G, Marjani M. Dysphagia lusoria caused by an aberrant right subclavian artery. Tex Heart Inst J 2004;31:168-71. [ Links ]
9. Crawford GB, Brindis RG, Krucoff MW, et al. Percutaneous atrial septal occluder devices and cardiac erosion: A review of the literature. Catheter Cardiovasc Interv 2012;80:157-67. DOI: 10.1002/ccd.24347. [ Links ]
10. Fukuhara S, Patton B, Yun J, et al. A novel method for the treatment of dysphagia lusoria due to aberrant right subclavian artery. Interact Cardiovasc Thorac Surg 2013;16:408-10. DOI: 10.1093/icvts/ivs517. [ Links ]
![]() Correspondence:
Correspondence:
Ernesto Cobos-González.
Division of Vascular Surgery.
Centro Especializado en Diabetes.
Prolongación Paseo de la Reforma 115-807,
Col. Paseo de las Lomas.
Delegación Álvaro Obregón.
01330 México D.F., México
e-mail: ecobos799@hotmail.com
Received: 28-11-2015
Accepted: 07-12-2015