Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.5 Madrid may. 2017
https://dx.doi.org/10.17235/reed.2017.4738/2016
ORIGINAL PAPERS
The use of the modified Neff classification in the management of acute diverticulitis
Aplicación de la clasificación de Neff modificada en el manejo de la diverticulitis aguda
Laura Mora-López, Roser Flores-Clotet, Xavier Serra-Aracil, Noemí Montes-Ortega and Salvador Navarro-Soto
Department of General Surgery. Hospital Universitari Parc Tauli. Universitat Autònoma de Barcelona. Barcelona, Spain
ABSTRACT
Introduction: Acute diverticulitis (AD) is increasingly seen in Emergency services. The application of a reliable classification is vital for its safe and effective management.
Objective: To determine whether the combined use of the modified Neff radiological classification (mNeff) and clinical criteria (systemic inflammatory response syndrome [SIRS] and comorbidity) can ensure safe management of AD.
Material and methods: Prospective descriptive study in a population of patients diagnosed with AD by computerized tomography (CT). The protocol applied consisted in the application of the mNeff classification and clinical criteria of SIRS and comorbidity to guide the choice of outpatient treatment, admission, drainage or surgery.
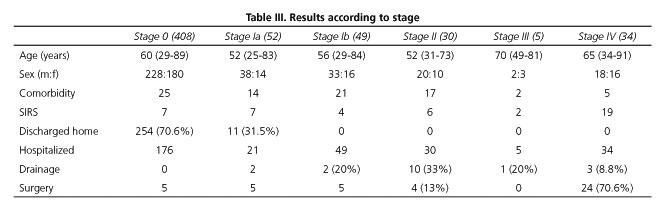
Results: The study was carried out from February 2010 to February 2016. A total of 590 episodes of AD were considered: 271 women and 319 men, with a median age of 60 years (range: 25-92 years). mNeff grades were as follows: grade 0 (408 patients 70.6%); 376/408 (92%) were considered for home treatment; of these 376 patients, 254 (67.5%) were discharged and controlled by the Home Hospitalization Unit; 33 returned to the Emergency Room for consultation and 22 were re-admitted; the success rate was 91%. Grade Ia (52, 8.9%): 31/52 (59.6%) were considered for outpatient treatment; of these 31 patients, 11 (35.5%) were discharged; eight patients returned to the Emergency Room for consultation and five were re-admitted. Grade Ib (49, 8.5%): five surgery and two drainage. Grade II (30, 5.2%): ten surgery and four drainage. Grade III (5, 0.9%): one surgery and one drainage. Grade IV (34, 5.9%): ten patients showed good evolution with conservative treatment. Of the 34 grade IV patients, 24 (70.6%) underwent surgery, and three (8.8%) received percutaneous drainage.
Conclusions: The mNeff classification is a safe, easy-to-apply classification based on CT findings. Together with clinical data and comorbidity data, it allows better management of AD.
Key words: Acute diverticulitis. Modified Neff classification. Outpatient treatment. Clinical practice.
RESUMEN
Introducción: la diverticulitis aguda (DA) es cada vez más frecuente en los servicios de Urgencias. Es necesario un manejo seguro y eficaz con criterios de clasificación que permitan un tratamiento dirigido.
Objetivo: verificar que la clasificación radiológica de Neff modificada (mNeff) asociada a criterios clínicos (síndrome de respuesta inflamatoria [SIRS] y comorbilidad) permite un manejo seguro de la DA.
Material y métodos: estudio descriptivo prospectivo en una población de pacientes diagnosticados de DA mediante tomografía computarizada (TC). El protocolo consiste en la aplicación de la clasificación de mNeff y criterios clínicos de SIRS y comorbilidad que permiten tratamiento ambulatorio, ingreso, drenaje o cirugía.
Resultados: el estudio comprende el periodo de febrero de 2010 a febrero de 2016, con un total de 590 episodios de DA en 271 mujeres y 319 hombres, con una edad mediana de 60 años (rango: 25-92 años). Grados de mNeff: grado 0 (408 pacientes, 70,6%): 376/408 (92%) tributarios a tratamiento domiciliario; alta 254/376 (67,5%); reconsultaron 33 pacientes y 22 reingresaron; éxito: 91%. Grado Ia (52, 8,9%): 31/52 (59,6%) tributarios a tratamiento ambulatorio; alta 11/31 (35,5%); reconsultaron ocho e ingresaron cinco. Grado Ib (49, 8,5%): cinco cirugías y dos drenajes. Grado II (30, 5,2%): diez cirugías y cuatro drenajes. Grado III (5, 0,9%): una cirugía y un drenaje. Grado IV (34, 5,9%): diez pacientes con buena evolución con tratamiento conservador; 24/34 (70,6%) fueron intervenidos; colocamos 3/34 (8,8%) drenajes percutáneos.
Conclusión: la clasificación de mNeff es una clasificación segura y aplicable basada en los hallazgos radiológicos de la TC. Junto con datos clínicos y de comorbilidad, permite un mejor manejo del cuadro de DA.
Palabras clave: Diverticulitis aguda. Clasificación de Neff modificada. Tratamiento ambulatorio. Práctica clínica.
Introduction
Diverticulosis has a prevalence of between 20% and 60% in the general population. The most frequent complication is acute diverticulitis (AD), which appears in 20-25% of cases. Its prevalence has risen in recent years due to the increase in the age of the general population and also due to dietary changes (1,2). As a result, Emergency Room (ER) consultations for this condition are becoming more frequent.
The presumptive diagnosis of AD can be made on the basis of a clinical history and physical examination. Abdominopelvic computed tomography (CT) is the diagnostic technique of choice because of its high sensitivity (97%) and specificity (98%) (3-6). CT is useful for diagnosis, but above all is most useful to evaluate the degree of inflammation, for differential diagnosis (vs ischemic colitis, inflammatory disease, tumor, and so on), to assist treatment (i.e., drainage of collections) and to predict the failure of conservative treatment and the risk of complications.
The ability to assess the severity of AD is important for therapeutic decision making. Several classifications for AD are currently available. The Hinchey system is a surgical classification and as such it is not particularly useful, since nowadays very few ADs require surgery (7-9). Multiple variations on the Hinchey system have been described based on radiological criteria: among others, the modified Hinchey, Kaiser, Kohler, Sher, Wasvary and Ambrosetti classifications (3,4,10).
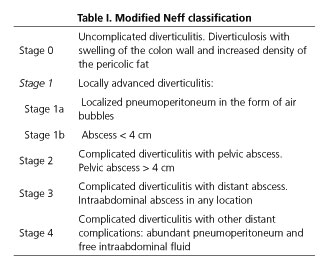
The modified Neff classification (mNeff) is based on the radiological findings of the CT scan (Table I). This classification allows a correct diagnosis of AD and stages it according to severity, from stage 0 (localized pericolic abscess) to stage IV (pneumoperitoneum and diffuse peritonitis) (11). This modified version includes the sub-stage Ia, which can now be differentiated due to recent technological advances. The degrees of radiological classification, together with clinical data, allow for a better management of this clinical entity (12-15).
Over time, management of AD has become more conservative both in the acute setting and in subsequent controls. Currently, the tendency is to manage uncomplicated AD at home. Treatment for complicated AD varies from antibiotic use only to resective surgery of the inflamed area in case of peritonitis or pneumoperitoneum (16-29).
To be able to decide on the correct treatment, criteria are needed to create an action protocol for all AD cases once diagnosed. Here we propose a protocol that can be implemented at any hospital with a radiology service and by any physician encountering this condition.
In this study we describe our experience with the application of a management protocol for AD which uses the mNeff radiological classification in combination with clinical criteria of comorbidity and SIRS, in order to be able to apply the most appropriate treatment in each case.
Material and methods
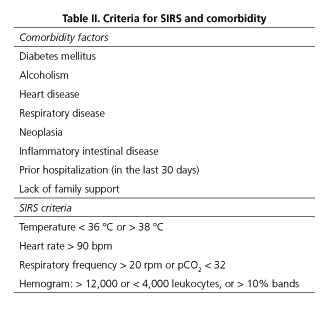
Prospective, observational study using a database including all consecutive patients attending our hospital's ER who were diagnosed with AD after their visit. Demographic data (age, sex), presence or absence of comorbidities (Table I), and presence of sepsis (SIRS) (Table II) were recorded, as well as the type of AD according to the radiological classification and its management in view of the clinical and radiological findings (discharge, hospitalization, drainage, surgery, re-admission or re-examination). Other factors unrelated to the application of the protocol were not considered.
At our service, after radiological diagnosis, the type of AD is graded using the mNeff classification (Table I). Clinical data are then assessed in order to define the appropriate management on a case-by-case basis. Among the clinical data, the SIRS criteria represent an important prognostic factor within the management of AD (12). The clinical assessment is completed with baseline data on comorbidities which allow an overall assessment of the patient and his/her ability to respond to the aggression that AD may represent (12-14) (Table II).
In accordance with the algorithm used at our center (Fig. 1), all patients arriving in the Emergency Room with suspected AD are given a CT scan to confirm the diagnosis and to classify the condition according to the mNeff system (Table I). Patients who present grade 0, do not present SIRS or any of the comorbidity factors present in table II, tolerate diet and have good pain control are discharged from the ER with antibiotic treatment and a residue-free diet, under a home health care scheme and seen at the outpatient service after two weeks. If they present SIRS or any of the comorbidity factors mentioned above, they are admitted for control observation and treatment.
Patients with type Ia AD receive antibiotic treatment and are kept under observation for 48 hours. Patients without comorbidities or SIRS who tolerate oral feeding and have no pain are discharged under a home health care scheme and seen at the outpatient service after two weeks.
From grade Ib upward, AD is considered to be complicated; patients are administered antibiotic treatment and are hospitalized. The grading determines the most suitable management. Grade Ib patients receive medical treatment. In grades II and III, drainage may be needed depending on the size (e.g., from 4 cm in diameter upward) and the accessibility of the abscess. Grade IV patients require surgical treatment in most cases, but always depending on their hemodynamic and clinical status.
In this study, the program SPSS 21.0 was used for the statistical analysis. Quantitative variables were described using means and standard deviations or medians and ranges when the distribution was not normal. Categorical variables are described in absolute numbers and percentages.
Results
Between February 2010 and February 2016, 590 cases of AD were diagnosed at our center (271 women and 319 men). The median age was 60 years (range 25-92 years). Twelve cases were removed from the AD management algorithm, either because the CT initially indicated some degree of AD but the differential diagnosis could not rule out a different condition such as neoplasia or colitis (5/12, 42%), or because of an unusual location such as the transverse colon (7/12, 58%). All of them required hospitalization. Therefore, 578 episodes were treated according to the management protocol (Table III).
Using the modified Neff classification, 408/578 (70.6%) were diagnosed with AD grade 0, 52 (8.9%) with grade Ia, 49 (8.6%) with grade Ib, 30 (5.2%) with grade II, five (0.9%) with grade III and 34 (5.9%) with grade IV. The management of these patients is displayed in the flow chart (Fig. 2).
Of the 408 AD stage 0, 376 (92.1%) met radiological and clinical criteria for home treatment. Of these, 254 (67.5%) were discharged with antibiotic treatment and control by the home hospitalization unit. The other 122 patients (32.5%) required hospital admission, due in most cases to poor pain control, food intolerance and, on rare occasions, refusal to follow the outpatient treatment protocol. During the follow-up, 33/254 (12.9%) returned to the ER for consultation, although only 22 (8.7%) required admission, with good evolution. The main reason for consultation or admission was pain and oral intolerance at home. In all, 232 out of 254 patients successfully completed home treatment, representing a success rate of 91%. Of the 376 patients initially considered for home hospitalization, 122 required admission, due in most cases to difficult pain control and, to a lesser extent, to food intolerance while in the ER. Of the 408 grade A patients, 176 patients required admission as a result of comorbidity or SIRS (32), oral intolerance or pain (122) or after re-consultation at the ER (22). Of the 176 patients admitted, five (2.8%) required surgery due to poor evolution.
Of the 52 AD stage Ia patients (8.9%), 31 (59.6%) met the criteria for outpatient treatment and eleven (35.5%) of these were discharged with antibiotic treatment and control by the home hospitalization unit. The remaining 20 required admission for pain or oral intolerance. During the follow-up, eight of the eleven on home treatment (72.7%) returned to the ER for consultation, of whom four (41.6%) required admission. Seven of the eleven patients completed home treatment, representing a success rate of 63.7%. Of all AD stage Ia patients, 45 were hospitalized. Of the 21 stage Ia patients (40.4%) who were admitted for SIRS or comorbidity factors, five (23%) required surgery, and in two (9.5%) cases the AD worsened and required drainage. The remaining patients evolved satisfactorily with antibiotic treatment.
Complicated AD (grades Ib, II, III and IV) were not considered for discharge and outpatient treatment, and were hospitalized. Of the 49 stage Ib patients (8.6% of all diagnosed cases), five required surgery and two required drainage. Of the 30 stage II patients (5.2%), ten required surgery and four, drainage. Of the five stage III patients (0.9%), one required surgery and another needed percutaneous drainage. Of the 34 stage IV patients (5.9%), ten (29.4%) had no comorbidity factors or SIRS criteria, and so conservative treatment was chosen, with satisfactory evolution. Drains were placed in three of the patients treated with antibiotics, with a good response. The remaining 24/34 (70.6%) underwent surgery.
The decision to insert an abdominal drain was taken in light of the radiological criteria of the size and accessibility of the abscess. None of the drains were associated with adverse effects. The success rate of drainage in our center was 100% since no cases of AD requiring drainage required surgery, and there were no complications associated with the placement of the drain.
Discussion
AD is an increasingly common entity whose management has evolved over time. Its treatment requires accurate diagnosis and clear staging criteria. This staging is the basis for the choice of a safe, effective and economical treatment in each particular case (30).
The diagnosis of AD requires the performance of a radiological test, in this case CT. CT has a high sensitivity (97%) and specificity (98%) for AD diagnosis. In addition, it is able to assess the degree of inflammation produced, allows differential diagnosis, and may also predict the failure of conservative treatment or the need for drainage (3-6). Once the diagnosis of AD has been made, and with all the data obtained with CT, we believe that it is important to be able to classify the condition in different degrees (3-6).
After reviewing classifications such as the Ambrosetti and the modified Hinchey systems (3,7,8), we decided to use the mNeff classification (11,15) (Table I), a radiology-based classification that distinguishes between six grades of AD and predicts its severity. The mNeff emphasizes the staging of patients with low radiological involvement: that is, it classifies stages 0 and Ia very well and, combined with clinical criteria, can define patients who can be assigned to home treatment and those requiring hospitalization and monitoring. In our study, 408 of 578 AD patients (70.6%) were diagnosed as grade 0, a proportion similar to that found by other groups. Of these, 254 out of 376 (67.5%) were assigned to home hospitalization, which was successful in 232 cases (91%). Our results are comparable to those reported by other groups in Spain and abroad, such as Alonso et al., Martín Gil et al., Ridgway et al. and Al-Sahaf et al., who demonstrated the safety of outpatient treatment for uncomplicated AD with treatment compliance rates of around 90% in all cases (23,34,37). In the recent prospective randomized study by Biondo et al. (the DIVER trial) (36), after a CT scan confirming the diagnosis of uncomplicated AD, the authors compared 66 patients per arm in which one group received outpatient treatment and the other was hospitalized. The study concluded that outpatient treatment is safe and effective. Although it used a different classification, like the mNeff system it also differentiated the uncomplicated AD group (AD G0).
The mNeff classification classifies patients requiring drainage within stages Ib and II. Not all patients with mNeff grade Ib, II or III will need drainage, but the mNeff classification helps to assess whether it is required. This coincides with the results presented by Ambrosetti's group, where 58% of patients with complicated AD were drained, and by Singh's group, which drained 47% of patients with Hinchey AD grade III (34).
The management of stage IV AD also allows assessment of the need for surgery. Our protocol favors individualizing the indication of surgery. Costi et al. (33) described a group of 39 patients with perforated AD who did not require surgery but were treated with antibiotics alone; drainage was required in only seven cases, all of whom presented satisfactory posterior evolution. Sallinen et al. (34) presented a study in which 189 patients with perforated AD responded well to conservative treatment, and the authors tried to find prognostic criteria for the need for surgery. In our study, ten out of 34 patients with stage IV AD responded well to conservative treatment. We believe that the use of clinical criteria increases the chances of a good response to conservative treatment. Perhaps when a larger number of patients have been assessed it will be possible to improve the mNeff classification and to define which groups of perforated or stage IV AD can be assigned to conservative treatment (always assuming that the clinical criteria permit).
At all radiological stages, it is important to include clinical criteria in the assessment. Data on comorbidity and SIRS can help to determine the degree of systemic involvement and the patient's likely response capacity (12,13).
The experience we have accumulated with this protocol over a 6-year period at our center suggests that AD can be managed safely. The protocol is similar to others presented by other groups in our country and elsewhere in Europe for the treatment of uncomplicated AD and its management at home (15,19,36,37), and it also defines the management of complicated AD. This last point means that at our center, AD can be treated by any practitioner with the required training, either at the ER or at the General Surgery Service. The protocol thus helps to standardize criteria and raises the safety levels for the treatment of patients with AD.
As our understanding of the pathophysiology of AD increases, we will be able to propose new advances in its management, such as conservative treatment of stage IV, or we might go even further and modify the management of uncomplicated AD, treating it with anti-inflammatory drugs alone (18,19,39-41).
Our protocol has weak points, such as the management of stage 0 ADs which cannot be treated on an outpatient basis despite meeting clinical criteria, and the need for a better definition of stage IV ADs in which the need for surgery in each particular case cannot be radiologically defined. Furthermore, we are unable to compare our group with a control group in which the protocol was not applied.
In spite of these limitations, we conclude that the mNeff classification, together with clinical data on SIRS and comorbidity, can help to define an effective and safe management protocol for any patient diagnosed with AD. Further studies are needed to determine which factors of comorbidity are most important within the management of the condition, which prognostic factor may be most helpful in uncomplicated cases, and how the management of complicated AD might be improved.
Acknowledgements
We thank the staff of the General Surgery Service who made it possible to apply the AD management protocol at our center, the staff at the Radiology Service for their help in implementing the mNeff classification, and the Home Hospitalization team.
References
1. Biondo S, López Borao J, Millan M, et al. Current status of acute colonic diverticulitis: A systematic review. Colorectal Dis 2011;14:e1-11. DOI: 10.1111/j.1463-1318.2011.02766.x. [ Links ]
2. Stollman N, Raskin JB. Diverticular disease of the colon. Lancet 2004;363:631-9. DOI: 10.1016/S0140-6736(04)15597-9. [ Links ]
3. Ambrosetti P, Grossholz C, Becker C, et al. Computed tomography in acute left colonic diverticulitis. Br J Surg 1997;84:532-4. DOI: 10.1046/j.1365-2168.1997.02576.x. [ Links ]
4. Kaiser AM, Jiang JK, Lake JP, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol 2005;100(4):910-7. DOI: 10.1111/j.1572-0241.2005.41154.x. [ Links ]
5. Liljegren G, Chabok A, Wickbom M, et al. Acute colonic diverticulitis: A systematic review of diagnostic accuracy. Colorectal Dis 2007;9:480-8. DOI: 10.1111/j.1463-1318.2007.01238.x. [ Links ]
6. Ambrosetti P, Jenny A, Becker C, et al. Acute left colonic diverticulitis - Compared performance of computed tomography and water-soluble contrast enema: Prospective evaluation of 420 patients. Dis Colon Rectum 2000;43:1363-7. DOI: 10.1007/BF02236631. [ Links ]
7. Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg 1978;12:85-109. [ Links ]
8. Wasvary H, Turfah F, Kadro O, et al. Same hospitalization resection for acute diverticulitis. Am Surg 1999;65(7):632-5. [ Links ]
9. Naraynsingh V, Maharaj R, Hassranah D, et al. Perforated left-sided diverticulitis with faecal peritonitis: Is the Hinchey classification the best guide for surgical decision making? Tech Coloproctol 2011;15(2):199-203. DOI: 10.1007/s10151-011-0675-7. [ Links ]
10. Dharmarajan S, Hunt SR, Birnbaum EH, et al. The efficacy of non-operative management of acute complicated diverticulitis. Dis Colon Rectum 2011;54:663-71. DOI: 10.1007/DCR.0b013e31820ef759. [ Links ]
11. Mora L, Serra S, Serra-AracilX, et al. Application of a modified Neff classification to patients with uncomplicated diverticulitis. Colorectal Dis 2013;15(11):1442-7. [ Links ]
12. Van de Wall BMJ, Draaisma WA, Van der Kaaij RT, et al. The value of inflammation markers and body temperature in acute diverticulitis. Colorectal Dis 2013;15:621-6. DOI: 10.1111/codi.12072. [ Links ]
13. Lorimer JW, Doumit G. Comorbility is a major determinant of severity in acute diverticulitis. Am J Surg 2007;193:681-5. DOI: 10.1016/j.amjsurg.2006.10.019. [ Links ]
14. Chapman J, Davies M, Wolff B, et al. Complicated diverticulitis: Is it time to rethink the rules? Ann Surg 2005;242(4):576-83. [ Links ]
15. Neff CC, Van Sonnenberg E. CT of diverticulitis: diagnosis and treatment. Radiol Clin North Am 1989;27:743-52. [ Links ]
16. Ribas Y, Bombardó J, Aguilar F, et al. Prospective randomized clinical trial assessing the efficacy of a short course of intravenously administered amoxicillin plus clavulanic acid followed by oral antibiotic in patients with uncomplicated acute diverticulitis. Int J Colorectal Dis 2010;25(11):1363-7. DOI: 10.1007/s00384-010-0967-9. [ Links ]
17. Vennix S, Morton DG, Hahnloser D. Systematic review of evidence and consensus on diverticulitis: An analysis of national and international guidelines. Colorectal Dis 2014;16(11):866-78. DOI: 10.1111/codi.12659. [ Links ]
18. Andeweg CS, Mulder IM, Felt-Bersma RJ. Guidelines of diagnostics and treatment of acute left-sided colonic diverticulitis. Dig Surg 2013;30(4-6):278-92. DOI: 10.1159/000354035. [ Links ]
19. Chabok A, Pthman L, Hjern F, et al; AVOD Study Group. Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 2012;99(4):532-9. DOI: 10.1002/bjs.8688. [ Links ]
20. Unlü C, De Korte N, Daniels L, et al. Dutch Diverticular Disease (3D) Collaborative Study Group. A multicenter randomized clinical trial investigating the cost-effectiveness of treatment strategies with or without antibiotics for uncomplicated acute diverticulitis (DIABOLO trial). BMC Surg 2010;10:23. DOI: 10.1186/1471-2482-10-23. [ Links ]
21. Wieghard N, Geltzeiler C, Tsikitis V. Trends in the surgical management of diverticulitis. Ann Gastroenterol 2015;28(1):25-30. [ Links ]
22. Peláez N, Pera M, Courtier R, et al. Applicability, safety and efficacy of an ambulatory treatment protocol in patients with uncomplicated acute diverticulitis. Cir Esp 2006;80:369-72. DOI: 10.1016/S0009-739X(06)70989-7. [ Links ]
23. Martín J, Serralta D, García A, et al. Safety and efficiency of ambulatory treatment of acute diverticulitis. Gastroenterol Hepatol 2009;32:83-7. [ Links ]
24. Rodríguez-Cerrillo M, Poza-Montoro A, Fernández-Díaz E, et al. Patients with uncomplicated diverticulitis and comorbidity can be treated at home. Eur J Intern Med 2010;21:553-4. DOI: 10.1016/j.ejim.2010.09.002. [ Links ]
25. Rodríguez-Cerrillo M, Poza-Montoro A, Fernández-Díaz E, et al. Treatment of elderly patients with uncomplicated diverticulitis, even with comorbidity, at home. Eur J Intern Med 2013;24:430-2. DOI: 10.1016/j.ejim.2013.03.016. [ Links ]
26. Etzioni DA, Chiu VY, Cannom RR, et al. Outpatient treatment of acute diverticulitis: Rates and predictors of failure. Dis Colon Rectum 2010;53:861-5. DOI: 10.1007/DCR.0b013e3181cdb243. [ Links ]
27. Ünlü C, Gunadi PM, Gerhards MF, et al. Outpatient treatment for acute uncomplicated diverticulitis. Eur J Gastroenterol Hepatol 2013;25:1038-43. DOI: 10.1097/MEG.0b013e328361dd5b. [ Links ]
28. Sánchez-Velázquez P, Grande L, Pera M. Outpatient treatment of uncomplicated diverticulitis: A systematic review. Eur J Gastroenterol Hepatol 2016;28:622-7. DOI: 10.1097/MEG.0000000000000610. [ Links ]
29. Jaung R, Robertson J, Vather R, et al. Changes in the approach to acute diverticulitis ANZ J Surg 2015;85:715-9. [ Links ]
30. McDermott FD, Collins D, Heeney A, et al. Minimally invasive and surgical management strategies tailored to the severity of acute diverticulitis. Br J Surg 2014;101:e90-9. DOI: 10.1002/bjs.9359. [ Links ]
31. Lorente L, Cots F, Alonso S, et al. Outpatient treatment of uncomplicated acute diverticulitis: Impact on healthcare costs. Cir Esp 2013;91:504:9. DOI: 10.1016/j.cireng.2013.01.007. [ Links ]
32. Sallinen VJ, Mentula PJ, Leppäniemi AK. Non-operative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Dis Colon Rectum 2014;57(7):875-81. DOI: 10.1097/DCR.0000000000000083. [ Links ]
33. Costi R, Cauchy F, Le Bian A, et al. Challenging a classic myth: Pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery in hemodynamically stable patients. A 10-year experience with non-operative treatment. Surg Endoscopy 2012;26:2061-71. DOI: 10.1007/s00464-012-2157-z. [ Links ]
34. Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum 2014;57:284-94. DOI: 10.1097/DCR.0000000000000075. [ Links ]
35. Luca Stocchi. Current indications and role of surgery in the management of sigmoid diverticulitis. World J Gastroenterol 2010;16(7):804-17. [ Links ]
36. Biondo S, Golda T, Kreisler E, et al. Outpatient versus hospitalization management for uncomplicated diverticulitis: A prospective, multicenter randomized clinical trial (DIVER Trial). Ann Surg 2014;259(1):38-44. DOI: 10.1097/SLA.0b013e3182965a11. [ Links ]
37. Alonso S, Pera M, Parés D, et al. Outpatient treatment of patients with uncomplicated acute diverticulitis. Colorectal Dis 2010;12(10):e278-82. DOI: 10.1111/j.1463-1318.2009.02122.x. [ Links ]
38. Ambrosetti P, Morel P. Acute left colonic diverticulitis. Indications for operation and predictive parameters of early and late medical treatment failure: A prospective non-randomised study of 423 patients. Dig Surg 1996;13:349-52. DOI: 10.1159/000172461. [ Links ]
39. Hjern F, Josephson T, Altman D, et al. Conservative treatment of acute colonic diverticulitis: Are antibiotics always mandatory? Scand J Gastroenterol 2007;42:41-7. DOI: 10.1080/00365520600780650. [ Links ]
40. Isacson D, Andreasson K, Nikberg M, et al. No antibiotics in acute uncomplicated diverticulitis: Does it work? Scand J Gastroenterol 2014;49:1441-6. [ Links ]
41. Shabanzadeh DM, Wille-Jorgensen P. Antibiotics for uncomplicated diverticulitis. Cochrane Database Syst Rev 2012;11(92):CD009092. [ Links ]
![]() Correspondence:
Correspondence:
Laura Mora López.
Department of General Surgery.
Hospital Universitari Parc Tauli.
Universitat Autònoma de Barcelona.
Parc Tauli, s/n.
08208 Sabadell, Barcelona. Spain
e-mail: Lmora@tauli.cat
Received: 25-11-2016
Accepted: 03-01-2017











 texto en
texto en