Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.6 Madrid jun. 2017
https://dx.doi.org/10.17235/reed.2017.4237/2016
CASE REPORT
Hepatic hematoma after ERCP: two new case reports
Hematoma hepático tras CPRE: presentación de dos nuevos casos
María-del-Moral-Martínez, Ana Delgado-Maroto, María Eloísa Cervilla-Sáez-de-Tejada, Francisco Javier Casado-Caballero and Francisco Javier Salmerón-Escobar
Clinical Management Unit of Digestive Diseases. Hospital Universitario San Cecilio. Granada, Spain
ABSTRACT
ERCP is an endoscopic procedure with a complication risk ranging from 2.5 to 8%. The most frequent complications are pancreatitis, cholangitis, hemorrhage or perforation. Hepatic hematoma after ERCP is a potentially serious, rare complication. Not many cases are reported in the literature. We present here two new cases of hepatic hematoma following ERCP along with a review of the literature and possible therapeutic options.
Key words: Hepatic hematoma. ERCP. Complication.
RESUMEN
La colangiopancreatografía retrógrada endoscópica (CPRE) es una técnica endoscópica con un riesgo de complicaciones secundarias que oscila del 2,5-8%. Las complicaciones que con más frecuencia se presentan son la pancreatitis, procesos infecciosos, hemorragia o perforación. El hematoma hepático secundario a CPRE es una rara y potencialmente grave complicación con pocos casos descritos en la literatura. A continuación presentamos dos casos de hematomas hepáticos secundarios a la realización de CPRE, realizando una revisión de la bibliografía y de las posibles opciones terapéuticas.
Palabras clave: Hematoma hepático. CPRE. Complicación.
Introduction
The endoscopic retrograde cholangiopancreatography ERCP is an endoscopic procedure with a complication risk ranging from 2.5 to 8%. The most frequent complications are pancreatitis, cholangitis, hemorrhage or perforation. Hepatic hematoma after ERCP is a potentially serious, rare complication. Not many cases are reported in the literature. We present here two new cases of hepatic hematoma following ERCP along with a review of the literature and possible therapeutic options.
Case report 1
A 37-year-old woman was admitted to hospital, as programmed, to perform an ERCP due to a diagnosis of a common-bile-duct stone the previous week via a magnetic resonance (MR) cholangiography. On admission, she was asymptomatic. The patient had no significant past medical and family history. During the examination, a marked cutaneous-mucous jaundice was observed. Laboratory tests showed: total bilirubin 7.91 mg/dl, direct bilirubin 7.13 mg/dl, aspartate aminotransferase (AST) 366 U/l, alanine aminotransferase (ALT) 407 U/l, GGT 812 U/l, and alkaline phosphatase (ALP) 332 U/l; the rest of the parameters showed no alteration.
An ERCP was performed, revealing a small papilla difficult to cannulate, and gaining access into the pancreatic duct on two occasions. By performing a precut, access was gained into the common bile duct, which was dilated, and an impacted calculus about 2 cm in diameter was found. A wide papillotomy was performed, the calculus was removed with the help of the Fogarty balloon and an outflow of retained bile and pus remains was observed.
Six hours after the ERCP was performed, the patient began to complain of intense diffuse abdominal pain associated with diffuse discomfort. She did not present with fever or hyperthermia. An urgent laboratory test showed amylase at 1,702 U/l and no other alterations. The patient was diagnosed with acute pancreatitis post-ERCP and she was prescribed serum therapy, nil per os (NPO), analgesic perfusion and vital signs monitoring. A few hours later, the patient had a presyncopal episode and her diffuse discomfort and intense abdominal pain persisted, observing a blood pressure (BP) of 85/45 mmHg, heart rate (HR) of 120 bpm and SatO2 of 97% with no O2 supply, so a new laboratory test was requested in order to evaluate possible complications.
A new laboratory test revealed a marked drop in hemoglobin from 12 to 7.6 g/dl, along with the already known hyperamylasemia; there was no rise in acute phase reactants and no other alterations. The patient presented neither tarry stools nor hematemesis, and no blood exteriorization was observed. In view of this findings, an abdominopelvic computed tomography (CT) scan was requested in order to preclude possible complications. The CT scan revealed two large subcapsular/intraparenchymal hypodense collections, one of them (measuring 70 x 107 x 120 mm) in the left hepatic lobe and the other one affecting the entire right hepatic lobe, compatible with hematomas. A small amount of subphrenic intraparenchymal air in contact with the right hepatic lobe collection was observed. Hepatic artery and portal vein permeability was noticed, with no contrast extravasation (Fig. 1).
A red blood cell transfusion and intravenous antibiotic therapy were initiated, and the patient was transferred to the Intensive Care Unit for stabilization and monitoring. An urgent arteriography revealed no contrast extravasation. Since the patient was successfully stabilized, afebrile and in good condition, with a stable hemoglobin level, she was managed by close observation. Two weeks later she remained afebrile and there was no evidence of additional bleeding, so she was discharged from the hospital. The patient attended monthly follow-up visits in the clinic, which included laboratory tests and ultrasound monitoring. No clinical or analytical repercussion was observed and the imaging tests showed a progressive reduction in the size of the injuries. Six months after being discharged, a follow-up abdominal CT scan was performed, which revealed that the two hypodense collections in the subphrenic space remained over the right and the left hepatic lobes, though they had decreased significantly, measuring about 11 x 8.5 x 10.5 cm and 2.8 x 2.6 x 2.3 cm (anteroposterior x lateral x transverse diameters, respectively).
Case report 2
A 60-year-old woman with no significant past medical history was admitted from the Emergency Department with clinical symptoms suggestive of cholangitis. During her stay, an MR cholangiography was performed, which revealed a retained 7.7 mm calculus in the common bile duct, about 4.4 cm from the papilla, with intra- and extrahepatic bile duct dilatation. In view of this finding, we decided to perform an ERCP, but the papilla of Vater could not be cannulated. Two days later, as the jaundice persisted, a new ERCP was performed. A fresh clot covering the papilla was detected. After removing it, access was gained into the bile duct, observing the calculus described during the MR cholangiography, which was removed after performing a biliary sphincterotomy. Finally, diluted epinephrine was injected into the papilla, still with signs of recent bleeding.
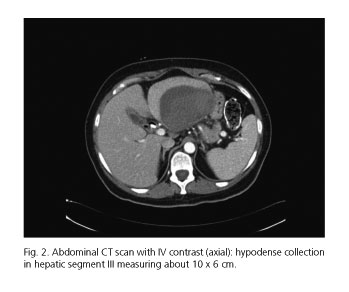
Seven days after being discharged from the hospital, the patient presented to the Emergency Department with fever, abdominal pain and intense asthenia. Laboratory tests showed hemoglobin (Hb) 8.6 g/dl, hematocrit (Hct) 27.2%, white blood cells (WBC) 10,000 U/ml with 68% polymorphonuclear, platelets 627,000 U/ml, and C-reactive protein (CRP9 187.4 mg/l. An abdominal ultrasound was performed, during which a hepatic space occupying lesion (SOL) in segment III measuring about 10 x 6 cm with ultrasound signs of an abscess was observed. Percutaneous drainage was attempted, but it was not possible due to the lesion density. A fine-needle biopsy was performed and Enterobacter cloacae was isolated in the culture of the obtained material.
A follow-up abdominal CT scan after antibiotic therapy revealed the lesion described above, corresponding to a possible hepatic hematoma (Fig. 2). Since a high fever persisted, an 8-Fr drainage catheter was placed.
After drainage, the patient remained asymptomatic, afebrile and hemodynamically stable. The patient underwent weekly abdominal ultrasound examinations to monitor the hematoma evolution, observing its progressive reduction. Six weeks later, the drainage was removed with no complications.
Discussion
ERCP is an endoscopic procedure with a complication rate ranging from 2.5 to 8% and a mortality rate ranging from 0.5 to 1%. The most frequently described complications are acute pancreatitis (1-7%), acute cholangitis (1.4%), hemorrhage (1%) and duodenal perforation (1%) (1). Nevertheless, there are some exceptional complications, such as hepatic hematoma.
Hepatic hematoma after ERCP is a rare complication, the frequency of which is scarcely reported. We have reviewed the cases reported in the literature, and when entering the terms "hepatic hematoma after ERCP" and "ERCP complications" in PubMed 25 cases reported to date were found (Table I).
Etiopathogenesis is not completely clear. Two hypothesis have been proposed. One of them states that the lesion would be caused by the guide wire usually used to cannulate the common bile duct, which would perforate the bile duct, thus damaging the hepatic parenchyma. As a result of this, blood vessels would break and air would enter the bile duct and the hematoma, which would explain the presence of subphrenic air in our first patient's CT scan. The other hypothesis states that the hepatic damage is secondary to the traction force exerted with the balloon on the bile duct when trying to remove a retained calculus. This force would cause the rupture of bile ductules and vessels, as well as the consequent bleeding (2).
The clinical manifestations are variable, including abdominal pain, anemia, fever and hemodynamic shock. According to the cases reported in the literature, abdominal pain was the first clinical manifestation in 87% of the cases, associated with anemia (29%) and fever (25%). The onset of symptoms can vary as well, ranging from hours to days. The longest period described in a case was fifteen days after ERCP (3).
The treatment must be personalized depending on the case. Those patients clinically and hemodynamically stable can be managed conservatively (3,4,5). Prophylactic antibiotic therapy is usually administered, given the high risk of infection. For those cases presenting with hemodynamical instability or associated complications, such as hematoma breakage, urgent surgical treatment should be considered (6,7,8). There are some case reports in which an arteriography with embolization of the bleeding vessel has successfully resolved the clinical situation (9,10).
References
1. García-Cano J, González Martín JA, Morillas Ariño J, et al. Complications of endoscopic retrograde cholangiopancreatography. A study in a small ERCP unit. Rev Esp Enferm Dig 2004;96:163-73. [ Links ]
2. Baudet JS, Arguiñarena X, Redondo I, et al. Subcapsular hepatic hematoma: An uncommon complication of endoscopic retrograde cholangiopancreatography. Gastroenterol Hepatol 2011;34(2):79-82. DOI: 10.1016/j.gastrohep.2010.11.002. [ Links ]
3. Servide MJ, Prieto M, Marquina T. Una rara complicación tardía tras CPRE: Hematoma hepático subcapsular. Rev Esp Enferm Dig 2016;108(4):234-5. [ Links ]
4. Orellana F, Irarrazaval J, Galindo J, et al. Subcapsular hepatic hematoma post ERCP: A rare or an underdiagnosed complication? Endoscopy 2012;44(Supl 2)UCTN:E108-9. DOI: 10.1055/s-0031-1291493. [ Links ]
5. Oliveira-Ferreira A, Tato-Marinho R, Velosa J. Infected hepatic hematoma 10 days after ERCP. Endoscopy 2013;45(Supl 2)UCTN:E402-3. [ Links ]
6. González-López R, García-Cano E, Espinosa-González O, et al. Surgical treatment for liver haematoma following endoscopic retrograde cholangiopancreatography. An unusual case. Cir Cir 2015;83(6):506-9. DOI: 10.1016/j.circir.2015.05.028. [ Links ]
7. Pérez-Legaz J, Santos J, Ruiz-Tovar J, et al. Subcapsular hepatic hematoma after ERCP (endoscopic retrograde cholangipancreatography). Rev Esp Enferm Dig 2011;103(10):550-1. DOI: 10.4321/S1130-01082011001000011. [ Links ]
8. Priego P, Rodríguez G, Mena A, et al. Subcapsular liver hematoma after ERCP. Rev Esp Enferm Dig 2007;99:53-4. [ Links ]
9. Klimová K, Padilla-Suárez C, González-Asanza C, et al. Subcapsular hepatic hematoma after ERCP: A case report and revision of literature. Clin Med 2014;03(03):161-6. DOI: 10.4236/crcm.2014.33039. [ Links ]
10. Chi KD, Waxman I. Subcapsular hepatic hematoma after guide wire injury during endoscopic retrograde cholangiopancreatography: Management and review. Endoscopy 2004;36(11):1019-21. DOI: 10.1055/s-2004-825861. [ Links ]
![]() Correspondence:
Correspondence:
María del Moral Martínez.
UGC Digestive Diseases.
Hospital Universitario San Cecilio.
Calle Dr. Oloriz, 16.
18012 Granada, Spain
e-mail: mdelmoral87@gmail.com
Received: 28-02-2016
Accepted: 27-12-2016











 texto en
texto en