My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.6 Madrid Jun. 2017
https://dx.doi.org/10.17235/reed.2017.4597/2016
LETTERS TO THE EDITOR
Atraumatic splenic rupture as a complication of acute exacerbation of chronic pancreatitis, an unusual disease
Rotura esplénica atraumática como complicación de pancreatitis crónica reagudizada, un fenómeno poco frecuente
Key words: Splenic rupture. Pancreatitis. Pseudocyst.
Palabras clave: Rotura esplénica. Pancreatitis. Pseudoquiste.
Dear Editor,
Atraumatic splenic rupture is a rare though serious complication of chronic pancreatitis. Approximately 11% of cases are associated with neighboring inflammatory processes.
Case report
A 48-year-old male patient with a history of chronic calcifying pancreatitis with frequent flare-ups of alcoholic origin presented with progressively increasing severe epigastric pain radiating to the back in a belt-like fashion following the ingestion of large amounts of alcohol.
Physical examination revealed a pale, sweaty patient with tachycardia and abdominal epigastric and bilateral hypochondrial tenderness. Lab results included hemoglobin at 7.8 g/dl and hematocrit at 23.5%. Amylase was also increased (338 U/l).
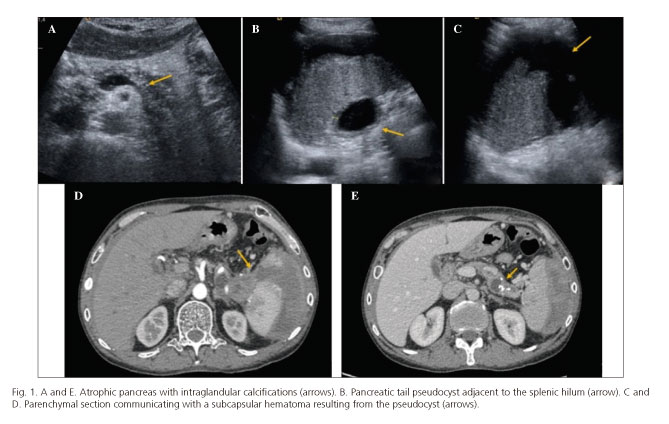
An abdominal ultrasound and contrast-enhanced computed tomography (CT) scan obtained in the late arterial phase and portal phase revealed an atrophic pancreas with disperse calcifications (Fig. 1A and E), as well as a pseudocyst at the splenic hilum (Fig. 1B), which extended across the visceral aspect towards the splenic parenchyma. This resulted in a splenic section communicating with a large subcapsular hematoma (Fig. 1C and D).
The patient underwent a CT-guided puncture draining of the perisplenic hematoma with a favorable outcome.
Discussion
The spleen is anatomically located near the tail of the pancreas, which partly accounts for the pathophysiology of splenic complications most commonly associated with chronic pancreatitis: pseudocysts, subcapsular hematoma, and rupture (1,2).
Among such complications, splenic rupture is rare (0.1-0.5%) (3), and is associated with local inflammatory processes in up to 11% of cases (4).
Initial treatment includes conservative management, percutaneous drainage (indicated for patients ineligible for surgery), and surgery (distal pancreatectomy and splenectomy), which represents a definitive therapy albeit with a high complication rate (5).
To conclude, diagnosing a splenic rupture in the absence of trauma is challenging, with a high index of suspicion being required in cases with pancreatitis.
Elena Moya-Sánchez and Antonio Medina-Benítez
Department of Radiodiagnosis. Complejo Hospitalario Universitario de Granada.
Granada, Spain
References
1. Hernani BL, Silva PC, Nishio RT, et al. Acute pancreatitis complicated with splenic rupture: A case report. World J Gastrointest Surg 2015;7:219-22. DOI: 10.4240/wjgs.v7.i9.219. [ Links ]
2. Sharada S, Olakkengil S, Rozario AP. Occult splenic rupture in a case of chronic calcific pancreatitis with a brief review of literature. Int J Surg Case Rep 2015;14:95-7. DOI: 10.1016/j.ijscr.2015.06.015. [ Links ]
3. Gedik E, Girgin S, Aldemir M, et al. Non-traumatic splenic rupture: Report of seven cases and review of the literature. World J Gastroenterol 2008;14:6711-6. DOI: 10.3748/wjg.14.6711. [ Links ]
4. Renzulli P, Hostettler A, Schoepfer AM, et al. Systematic review of atraumatic splenic rupture. Br J Surg 2009;96:1114-21. DOI: 10.1002/bjs.6737. [ Links ]
5. Heider R, Behrns KE. Pancreatic pseudocysts complicated by splenic parenchymal involvement: Results of operative and percutaneous management. Pancreas 2001;23:20-5. DOI: 10.1097/00006676-200107000-00003. [ Links ]











 text in
text in