My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.7 Madrid Jul. 2017
https://dx.doi.org/10.17235/reed.2017.4811/2015
CASE REPORT
Primary peripancreatic lymph node tuberculosis as a differential diagnosis of pancreatic neoplasia
Tuberculosis ganglionar peripancreática primaria como diagnóstico diferencial de neoplasia pancreática
Nuria García-del-Olmo, Andrea Boscà-Robledo, Rafael Penalba-Palmí, Elena Añón-Iranzo and Javier Aguiló-Lucía
Department of General Surgery and Digestive Diseases. Hospital Lluís Alcanyís. Xàtiva, Valencia. Spain
ABSTRACT
Primary peripancreatic lymph node tuberculosis is an exceptional entity in immunocompetent patients, but its incidence is increasing in developed countries in recent years due to increasing immigration. It usually presents as a pancreatic mass and is misdiagnosed as pancreatic neoplasia in most cases, with the diagnosis of tuberculosis occurring after surgery. We report the case of a 38 year old Pakistani man with abdominal pain of several months duration, who was initially diagnosed with a pancreatic neoplasm after detecting a mass in the pancreatic isthmus by computed tomography (CT) and abdominal magnetic resonance imaging (MRI). However, after performing an endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB), the patient was diagnosed with peripancreatic lymph node tuberculosis. After receiving anti-tuberculous treatment, the patient presented clinical improvement, despite a small reduction in the lesion size. In conclusion, peripancreatic lymph node tuberculosis is part of the differential diagnosis of pancreatic neoplasia. Endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB) represents a valuable and useful diagnostic tool for detecting this pathology, avoiding surgeries with a high morbidity and mortality.
Key words: Peripancreatic lymph node tuberculosis. Endoscopic ultrasound. Pancreatic neoplasm.
RESUMEN
La tuberculosis ganglionar peripancreática primaria es una entidad excepcional especialmente en pacientes inmunocompetentes, pero su incidencia está incrementándose en nuestro medio durante los últimos años debido a la creciente inmigración. Suele presentarse como una masa pancreática y se diagnostica erróneamente como neoplasia de páncreas en la mayoría de los casos, realizándose el diagnóstico de tuberculosis tras la cirugía. Presentamos el caso de un varón de 38 años pakistaní con un cuadro de dolor abdominal de varios meses de evolución que inicialmente se diagnosticó de neoplasia pancreática tras detectar mediante tomografía computarizada (TC) y resonancia magnética nuclear (RMN) abdominal una masa en el istmo pancreático. No obstante, tras realizar una ecoendoscopia con toma de biopsias mediante punción-aspiración con aguja fina (PAAF) se diagnosticó de tuberculosis ganglionar peripancreática. Tras recibir tratamiento antituberculoso el paciente presentó mejoría clínica, a pesar de una escasa reducción del tamaño de la lesión. En conclusión, la tuberculosis ganglionar peripancreática forma parte del diagnóstico diferencial de la neoplasia de páncreas. La toma de biopsias guiada por ecoendoscopia representa una herramienta diagnóstica de gran valor y utilidad en la detección de dicha patología, evitando realizar cirugías con elevada morbimortalidad.
Palabras clave: Tuberculosis ganglionar peripancreática. Ecoendoscopia. Neoplasia pancreática.
Introduction
Peripancreatic lymph node tuberculosis is a very rare disease, and is associated in most cases with immunodepression. It is an isolated peripancreatic lesion, which is confirmed microbiologically, in the absence of known tuberculosis (TB) and without the involvement of other organs or tissues. On imaging studies it is usually presented as a cystic or solid pancreatic mass, an abscess or pancreatitis. Most cases are misdiagnosed as pancreatic neoplasm, performing the correct diagnosis of TB after surgery.
Case report
We present the case of a 38-year-old Pakistani man, only residing in Spain for seven years with no medical history of interest or toxic habits, who had recently traveled to his country of origin. The patient reported a 4-month history of intermittent abdominal pain refractory to analgesia, with isolated episodes of dysthermia and coluria, but without jaundice. He did not present a constitutional syndrome, cough, hemoptysis, or other associated symptoms. Physical examination showed a good general condition, a normal cardiopulmonary auscultation and absence of inguinoaxillary and supraclavicular adenopathies. He did not present oral thrush or mucocutaneous jaundice. The abdomen was soft and depressible, painless at the time of examination and without masses or megalias.
An analysis was performed in which only a gamma glutamyl transferase (GGT) of 70 IU/l stood out, with levels of leukocytes, erythrocyte sedimentation rate (ESR), lutamic oxaloacetic transaminase (GOT), glutamate-pyruvate transaminase (GPT), total bilirubin, amylase and alkaline phosphatase within normal limits. Tumor markers carcinoembryonic antigen (CEA) and carbohydrate antigen (CA) 19.9 levels were normal and serology for HIV, hepatitis C (HCV) and hepatitis B (HBV) was negative.
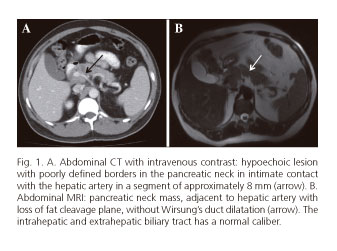
On ultrasound and abdominal computed tomography a heterogeneous and hypoechoic mass, with poorly defined edges and a 20 x 21.5 x 27 mm diameter, was observed. It affected the pancreatic isthmus and was in contact with the hepatic artery with possible infiltration, without Wirsung's duct dilatation or involvement of the bile duct (Fig. 1A). Given these findings, a locally advanced pancreatic neoplasm was suspected. However, due to the doubts with regard to the nature of the injury and in order to assess the possible vascular infiltration, an abdominal MRI was performed, which confirmed, in addition to the previously described findings, a loss of fatty cleavage plane between the hepatic artery and pancreatic mass (Fig. 1B). With the purpose of establishing the etiological diagnosis, a radial echoendoscopy was performed, which confirmed the presence of a heterogeneous periduodenal mass with poorly defined edges with a 2.3 cm diameter, at the level of the bulb and second duodenal portion, with no infiltration of the wall, adjacent to the superior mesenteric vein and the hepatic artery, but with a separation plane and with no apparent infiltration of the structures (Fig. 2.1). Finally, a linear echoendoscopy and 25G needle-biopsies of the mass were performed. The sample was submitted to cytology and a necrotizing granulomatous lymphadenitis compatible with tuberculosis was observed (Figs. 2.2A y 2.2B). Before these results, a microbiological study was also performed, obtaining a positive polymerase chain reaction (PCR) for Mycobacterium tuberculosis, despite a negative Ziehl-Neelsen staining and Lowenstein culture. The absence of pulmonary and thoracic node involvement was verified by a simple chest x-ray and thoracic CT. Therefore, the diagnosis of primary peripancreatic lymph node tuberculosis was confirmed. After six months of anti-tuberculous medical treatment (six months with quadruple therapy: rifampicin, isoniazid, pyrazinamide and ethambutol; and five months with double therapy: rifampicin and isoniazid), the patient presented almost complete symptom resolution, although the tumor size remained similar in the control CT (19 x 20 x 24 mm).
Discussion
TB is a common pathology in undeveloped countries, with an annual incidence of 9.7 million (4). However, due to increasing immigration and cases of HIV immunosuppression, its presence is increasing in developed countries in recent years (1-10). Pulmonary tuberculosis is the most frequent form of presentation. Extrapulmonary forms are uncommon, occurring especially in immunodeficient hosts. Abdominal CT affects mainly the ileocecal junction and may also affect the rest of the gastrointestinal tract, peritoneum, lymph nodes and solid organs such as the liver, spleen and, in exceptional cases, the pancreas (1-10). In this article, we present the case of a peripancreatic lymph node tuberculosis.
Peripancreatic and pancreatic ganglionic TBC are very rare entities, especially the latter, with an incidence reported since 1944 of less than 4.7% (1-3). Primary peripancreatic lymph node tuberculosis should have the following diagnostic criteria: isolated lesion with microbiological confirmation, absence of previous known TB and no affectation at other levels (8). Its initial diagnosis is complex given the lack of specificity of its symptoms (abdominal pain, constitutional syndrome, jaundice, pancreatitis or abdominal mass) and radiological findings. Due to all of these factors, and given the high clinical suspicion required, pancreatic neoplasm is frequently misdiagnosed, because its clinical and radiological manifestations are very similar (4-6,8). However, because of its different therapeutic approach, it is very important to perform a correct diagnosis in order to avoid unnecessary surgeries of a high morbidity and mortality. For this reason, it is essential to obtain an endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB) to perform a microbiological and cytological study (1-10). The presence of caseous granulomas in cytology is highly suspicious for TB, in which case a positive Ziehl-Neelsen and/or culture is required for microbiological confirmation. However, since the extrapulmonary forms of TB are paucibacillary, the diagnostic yield of these techniques may be low and depend on the quality of the sample obtained. Therefore, given the suspicion of TB and negative results from previous microbiological techniques, we can diagnose TB with positive results by using other faster methods, such as adenosine deaminase (ADA), interferon gamma (INF-γ) and the polymerase chain reaction (PCR) of tuberculous bacillus, as in our case. However, in spite of the available variety of diagnostic techniques, with inconclusive results of fine-needle aspiration (FNA) biopsies, it may be necessary to resort to surgery to reach a certain diagnosis (1-3,8).
In conclusion, peripancreatic lymph node TBC should be considered in the differential diagnosis of a pancreatic mass, especially in young people living in endemic areas. Endoscopic ultrasound-guided fine-needle aspiration biopsy is a necessary and useful technique for establishing a correct preoperative diagnosis and avoiding unnecessary surgical interventions with considerable morbidity and mortality (1-10).
References
1. Yamada R, Inoue H, Yoshizawa N, et al. Peripancreatic tuberculous lymphadenitis with biliary obstruction diagnosed by endoscopic ultrasound-guided fine-needle aspiration biopsy. Intern Med 2016;55:919-23. DOI: 10.2169/internalmedicine.55.6123. [ Links ]
2. Kim J-B, Lee S, Kim S-H, et al. Peripancreatic tuberculous lymphadenopaty masquerading as pancreatic malignancy: A single-center experience. J Gastroenterol Hepatol 2014;29:409-16. DOI: 10.1111/jgh.12410. [ Links ]
3. Chaudhary P, Bhadara U, Arora M, et al. Pancreatic tuberculosis. Indian J Surg 2015;77(6):517-24. DOI: 10.1007/s12262-015-1318-4. [ Links ]
4. Sonthalia N, Ray S, Pal P, et al. Fine needdle aspiration diagnosis of isolated pancreatic tuberculosis: A case report. World J Clin Cases 2013;16;1(5):181-6. DOI: 10.12998/wjcc.v1.i5.181. [ Links ]
5. Sportes A, Kpossou R, Bernardin S. Isolated pandreatic tuberculosis mimicking inoperable pancreatic cancer: A diagnostic challenge resolved using endoscopic ultrasound-guided fine-needle aspiration. Can J Gastroenterolol 2013;27(8):445-7. DOI: 10.1155/2013/198715. [ Links ]
6. Goel V, Shivakumar K, Rajaram B, et al. Tuberculous celiac axis lymphadenopathy mimicking cystic pancreatic neoplasm - A diagnostic dilemma. Indian J Surg Oncol 2014;5(4):278-81. DOI: 10.1007/s13193-014-0320-9. [ Links ]
7. Liu Q, He Z, Bie P. Solitary pancreatic tuberculous abscess mimicking prancreatic cystadenocarcinoma: A case report. BMC Gastroenterol 2003;10;3:1. DOI: 10.1186/1471-230X-3-1. [ Links ]
8. Barquilla-Cordero P, Chiquero-Palomo M, Martín-Noguerol E, et al. Primary pancreatic tuberculosis in an immunocompetent patient: First case report in Spain. Gastroenterol Hepatol 2010; 33(8): 582-5. DOI: 10.1016/j.gastrohep.2010.06.002. [ Links ]
9. Vafa H, Arvanitakis M, Matos C, et al. Pancreatic tuberculosis diagnosed by EUS: One disease, many faces. JOP 2013;10;14(3):256-60. [ Links ]
10. Ray S, Das K, Mridha AR. Pancreatic and peripancreatic nodal tuberculosis in immunocompetent patients: Report of three cases. JOP 2012;10;13(6):667-70. [ Links ]
![]() Correspondence:
Correspondence:
Nuria García del Olmo.
Department of General Surgery and Digestive Diseases.
Hospital Lluís Alcanyís.
Ctra. Xátiva-Silla, km. 2.
46800 Xàtiva, Valencia.
Spain
e-mail: nuriagarciadelolmo@gmail.com
Received: 12-01-2017
Accepted: 04-03-2017











 text in
text in