My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.8 Madrid Aug. 2017
https://dx.doi.org/10.17235/reed.2017.4809/2016
A real life study of Helicobacter pylori eradication with bismuth quadruple therapy in naïve and previously treated patients
Erradicación de Helicobacter pylori con terapia cuádruple con bismuto en pacientes naïve y fracasos previos: experiencia en la práctica clínica real
Blas José Gómez-Rodríguez, Luisa Castro-Laria, Federico Argüelles-Arias, Cristina Castro-Márquez, Ángel Caunedo-Álvarez and Manuel Romero Gómez
Clinical Management Unit of the Gastroenterology Department. Hospitales Universitarios Virgen Macarena y Virgen del Rocío. Seville, Spain
ABSTRACT
Objective: To evaluate the efficacy and safety of a quadruple regimen (BMTO) of the "3-in-1 capsule" (containing bismuth subcitrate potassium, metronidazole and tetracycline) plus omeprazole in naïve and previously treated patients diagnosed with Helicobacter pylori (H. pylori) infection in the clinical setting in Seville (Spain).
Methods: This is a prospective study carried out on consecutive patients with a confirmed H. pylori infection and upper gastrointestinal symptoms. After providing their informed consent, the patients were treated for ten days with a 3-in-1 capsule containing bismuth subcitrate potassium (140 mg), metronidazole (125 mg) and tetracycline (125 mg: Pylera®), three capsules four times daily, plus omeprazole (20 or 40 mg) twice daily. Eradication of infection was determined by a negative urea breath test at least 28 days after the end of treatment.
Results: A total of 58 consecutive patients were enrolled into this study, two of whom withdrew early due to vomiting on days three and five, respectively. In this cohort, 17 patients (29.3%) had a prior history of medication to treat H. pylori. In the intent-to-treat population, eradication was achieved in 97.6% (40/41) and 82.4% (14/17) of cases in patients treated with BMTO as a first-line or rescue therapy, respectively. At least one adverse event was reported by 28 (48%) patients, mostly mild effects (86%).
Conclusion: A ten day treatment with BMTO is an effective and safe strategy to combat confirmed H. pylori infection in patients.
Key words: Helicobacter pylori. Bismuth-based quadruple therapy. Pylera®. Eradication.
RESUMEN
Objetivo: evaluar la eficacia y seguridad de la terapia cuádruple con omeprazol más "una cápsula tres-en-uno" que contiene subcitrato de bismuto, metronidazol y tetraciclina (BMTO) en pacientes, naïve y fracasos previos, diagnosticados de infección con Helicobacter pylori, en el área de Sevilla, en condiciones de práctica clínica habitual.
Métodos: estudio prospectivo realizado en pacientes consecutivos con infección confirmada por Helicobacter pylori y síntomas gastrointestinales del tracto superior. Los pacientes fueron tratados, tras firmar el consentimiento, con Pylera® (cápsula tres-en-uno que contiene 140 mg de subcitrato de bismuto, 125 mg de metronidazol y 125 mg de tetraciclina) cuatro veces al día, más omeprazol (20 o 40 mg) dos veces al día, durante diez días. La erradicación fue establecida mediante un test de urea en aliento negativo realizado, al menos, 28 días después de finalizar el tratamiento.
Resultados: un total de 58 pacientes fueron incluidos consecutivamente, dos de ellos fueron retirados del estudio por vómitos al tercer y quinto día, respectivamente. Diecisiete (29,3%) pacientes tenían historia previa de tratamiento de su infección por Helicobacter pylori. En la población por intención de tratar las tasas de erradicación fueron del 97,6% (40/41) y del 82,4% (14/17) en los pacientes tratados con Pylera® como primera línea o como terapia de rescate, respectivamente. Veintiocho pacientes (48%) presentaron, al menos, un acontecimiento adverso, la mayoría (86%) leves.
Conclusión: diez días de tratamiento con BMTO es una estrategia eficaz y segura en pacientes con infección confirmada por Helicobacter pylori.
Palabras clave: Helicobacter pylori. Terapia cuádruple basada en bismuto. Pylera®. Erradicación.
Introduction
Helicobacter pylori (H. pylori) is a ubiquitous gram-negative bacterium considered to be the most common bacterial infection in humans, affecting approximately 50-75% of the population worldwide (1,2). H. pylori is associated with a wide range of upper gastrointestinal diseases including peptic ulcer, gastric cancer and gastric mucosal-associated lymphoid tissue (MALT) lymphoma (3,4). Although a variety of treatment regimens have been proposed for the eradication of H. pylori, the ideal regimen to treat this infection has not been defined (5,6). During the last decades, standard triple regimens that combine a proton pump inhibitor (PPI) with two antibiotics (amoxicillin, clarithromycin or metronidazole) have been recommended as first-line therapies against H. pylori in several countries and regions (7-9). However, the use of PPI-based triple therapy has led to an increase in the prevalence of H. pylori resistance to metronidazole and clarithromycin (6,10,11), thus, reducing the rates of eradication by an order of 50 to 70% (12-15). According to the recommendations of the IV Spanish Consensus Conference on the treatment of H. pylori infection, a treatment should be considered as effective when it is capable of eradicating H. pylori infection in approximately 90% of patients (15).
The high rates of clarithromycin resistance have made triple therapy with omeprazole, amoxicillin and clarithromycin (OAC) inappropriate, especially given that local clarithromycin resistance rates may exceed 15% (15,16). Indeed, while the clarithromycin and/or metronidazole resistance rates are unknown in the current study area, the mean resistance to clarithromycin (18.3%) and metronidazole (40.8%), and the dual resistance rate (10.1%) in Spain are available (17). Indeed, this reduction in eradication rates has led to the development and use of new first-line treatments (18,19).
In Spain, a quadruple regimen without bismuth (PPI, clarithromycin, amoxicillin and metronidazole) is currently recommended as a first-line treatment (15). However, patients who fail to respond to these triple or quadruple therapies that include clarithromycin are recommended a regimen that includes levofloxacin and, preferably, a quadruple regimen (PPI, amoxicillin, levofloxacin and bismuth). In other cases these patients are recommended a quadruple bismuth-based therapy (PPI, bismuth, tetracycline and metronidazole) (15).
The Maastricht V/Florence Consensus Report recommended a quadruple regimen of bismuth, metronidazole and tetracycline plus omeprazole (BMTO) (16), indicating that it produces a high eradication rate in patients with a previously failed H. pylori eradication with other regimens (5,25-29). Furthermore, this consensus also recommended that in regions of high dual clarithromycin and metronidazole resistance (> 15%), bismuth-containing quadruple therapies should be the treatment of choice (16). The currently available evidence has consistently shown that BMTO therapy achieved eradication rates ranging between 84 and 97% when administered as a first line therapy (20-24). Moreover, BMTO therapy has the advantage that H. pylori does not become resistant to bismuth (30), and its effects are not influenced by clarithromycin or fluoroquinolone resistance (31).
Based on the above, this study aimed to evaluate the efficacy and safety of a quadruple therapy in a clinical setting in patients diagnosed with H. pylori infection. The regimen was based on a 3-in-1 capsule containing bismuth subcitrate, metronidazole and tetracycline, with the addition of omeprazole (BMTO).
Methods
This is a prospective, open-label, single-center, interventional study carried out at the Clinical Management Unit of the Gastroenterology Department of a hospital in Seville between February 15th and October 15th 2016. The cohort consisted of consecutive patients with a confirmed H. pylori infection receiving PPI-bismuth-based quadruple therapy (Pylera®, Allergan Inc., Irvine, CA) under real-life conditions. The patients were recruited at the outpatient clinic or referred for a study of their dyspeptic symptoms.
The study protocol was approved by the ethical research committee of the Virgen Macarena and Virgen del Rocío university hospitals. All patients were fully informed about the details of the study and they provided their written informed consent prior to inclusion into the study. The ethical principles outlined in the Declaration of Helsinki and those of the Good Clinical Practice were followed.
Eligible patients were aged 18 years or older, with a confirmed H. pylori infection, upper gastrointestinal symptoms and indications for treatment with an eradication therapy. H. pylori infection was confirmed by at least one of the following methods: 13C-urea breath test, histology, or a rapid urease test. Patients were excluded if they had contraindications/allergy to any of the drugs/excipients used in the study, substantial organ impairment, if they had undergone surgery of the upper gastrointestinal tract, if they presented clinically significant associated conditions (insulin dependent diabetes mellitus, neoplastic diseases, coagulation disorders and hepatic, cardiorespiratory or renal diseases), pregnancy or lactation. These inclusion/exclusion criteria were chosen to provide a study population as homogeneous as possible. In order to avoid any associated bowel motility disorders which could represent a confounding factor, patients undergoing upper digestive tract surgery and/or with diabetes mellitus were excluded.
Study treatment
The ten day bismuth-based quadruple therapy regimen consisted of three Pylera® capsules (a three-in-one capsule containing bismuth subcitrate potassium 140 mg, metronidazole 125 mg, and tetracycline 125 mg) four times a day (breakfast, lunch, afternoon snack and dinner) plus omeprazole (20 or 40 mg based on the patient's needs: gastroesophageal reflux disease, gastric mucosa protection, etc.) twice daily (30 minutes before breakfast and afternoon snack).
Probiotic agents were added to the regimen at the beginning of the study for those patients who reported prior gastrointestinal symptoms, mainly diarrhea, either in association with earlier eradication regimens or in relation to prior antibiotic administration for other pathologies. Patients were asked to refrain from consuming alcohol or smoking during the entire treatment period and the subjects were instructed not to take Pylera® with milk or other dairy products and to refrain from sunbathing.
Objectives
The primary outcome measure of efficacy was H. pylori eradication, determined by a negative urea breath test performed at least 28 days after the end of treatment (no antibiotic or PPI consumption for four weeks). The secondary end-point was safety, which was monitored via the adverse events (AEs). AEs events were identified verbally in response to generic questions such as: how are you?, have you experienced any new symptom or discomfort since your last visit? In addition, the relationship of the AE with the study drug was determined by assessing whether any relationship existed between the AE and the mechanism of action of the drug, or if such an event had been experienced previously. AEs were classified as follows: a) mild: the patient was aware of the signs or symptoms but it was readily tolerated and no medical intervention/therapy was required; b) moderate: a discomfort that interfered with the patient's usual activities and that required minimal medical intervention/therapy; and c) severe: a disabling effect that impeded working or performing usual daily activities and that might even have been life threatening or required medical or surgical intervention.
Statistical analysis
A standard statistical analysis was performed using MedCalc 16.8.4 (MedCalc Software bvba, Ostend, Belgium). The data were expressed as the number (percentage), mean (standard deviation [SD]), mean (95% confidence interval [95% CI]) or median (95% CI) as appropriate. Categorical variables were compared using the Chi-squared test and Fisher's exact test, as necessary. The intent-to-treat (ITT) efficacy analyses were based on all the patients who received the study medication and had completed at least one valid follow-up visit. Patients with no observed outcome were considered as treatment failures. Per protocol (PP) analyses were also conducted to confirm the ITT results, which excluded patients who did not complete the study or who had seriously violated the protocol.
A conditional hazard model with patient intraclass correlation was used to estimate and to test factors associated with BMTO treatment failure. A conditional hazard model was used for univariate and multivariate analysis, adopting a backward strategy with a statistically significant cut-off for variable screening of 0.05. Potential predictors were categorized as having low or high values based on the median of the sample and the factors associated with failure in the univariate analysis at p ≤ 0.2 were included in a multivariate analysis. A p value < 0.05 was considered to be significant.
Results
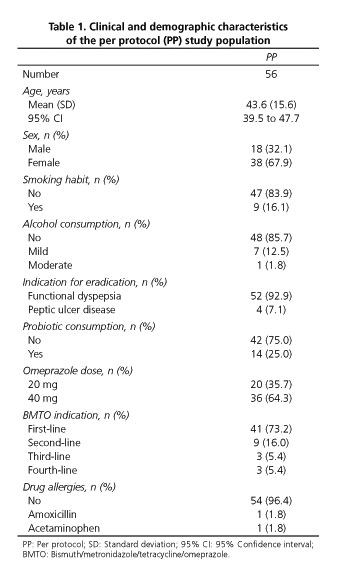
Of the 102 patients who were screened, 58 fulfilled the inclusion and exclusion criteria and were included in the ITT analysis (Fig. 1). Two of these patients withdrew from the study early after suffering bouts of vomiting on days three and five, respectively. Thus, a total of 56 of the 58 selected patients concluded the study; the principal demographic and clinical characteristics are shown in table 1. The mean treatment compliance with the study drug was greater than 90% for the patients who completed the full treatment course (56/58), and 17 (29.3%) of these patients had a prior history of using medication to treat H. pylori, most often clarithromycin, amoxicillin and PPIs.
H. pylori eradication rates were 93.1% (95% CI: 88.1-98.1%) in the overall study population (ITT population) and 96.4% in the PP population (95% CI 92.8-100%). According to the ITT analysis, the eradication rate was 97.6% among the patients that received the BMTO treatment as first-line therapy (40/41, 95% CI: 94.6-100%) and 82.3% in the patients that received BMTO as a rescue therapy (14/17, 95% CI: 74.8-89.8%). In contrast, the eradication rates in the PP population were 97.6% as a first-line therapy (40/41, 95% CI: 94.6-100%) and 93.3% in those patients that received BMTO as a rescue therapy (14/15, 95% CI: 88.4-98.2%).
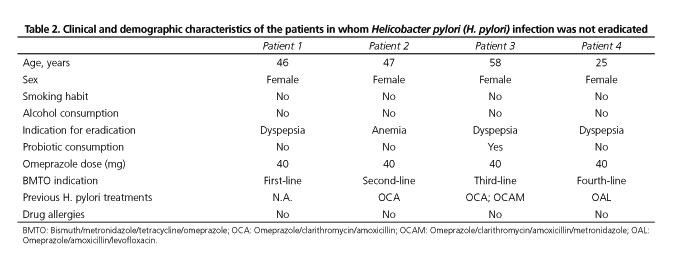
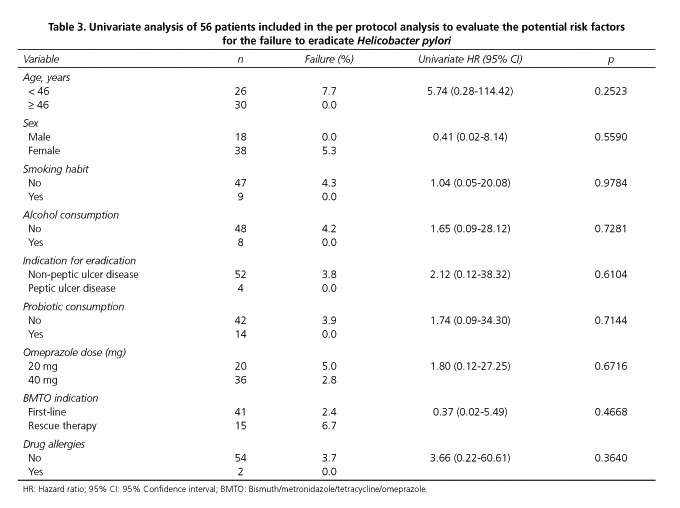
The characteristics of the patients in whom H. pylori infection was not eradicated were also assessed (Table 2). In a univariate analysis, none of the variables studied were significantly associated with successful eradication (Table 3). Since none of the study variables reached a significance value at or below 0.2 in the univariate analysis, no multivariate analysis was performed.
Of the 58 patients included in the safety analysis, 51 patients (88%) had a good tolerance of the BMTO therapy, although two (3.4%) patients withdrew from the study after vomiting on days three and five, respectively. The proportion of patients reporting at least one treatment-related AE was 48.2% (28/58), while nine patients (15.5%) reported more than one AE. The mean (SD) duration of the AE was 7.7 (2.9) days, with 28 patients (48.2%) reporting AEs related to the upper digestive tract and ten patients (17.2%) reporting AEs related to the central nervous system. The most commonly reported AEs were Diarrhea (ten, 17.2%), nausea (eight, 13.8%) and asthenia (seven, 12.1%). Other AEs reported by the patients were: dark stools (four), dyspepsia (two), dysgeusia (two), vomiting (one), headache (one) and upper abdominal pain (one). Most of the AEs were classified as mild (86%) and although one patient had an episode of diarrhea that was classified as severe, it was resolved with oral medication without the need for hospitalization.
Discussion
These data from a real-life study conducted in Seville demonstrate that ten days of Pylera® treatment is an effective and safe strategy to combat H. pylori infection in an ITT population, not only as first line but also as a second line therapy. These results were confirmed in the PP efficacy analysis. Moreover, the study failed to find significant differences between the use of BMTO therapy as a first line or as a rescue therapy in either the ITT or PP populations.
The eradication rates with quadruple therapy were similar (ca. 82-97%) to those of previous studies that used the same three-in-one capsule four times daily with omeprazole twice daily (80-93.2%) (20,21,24,27). In a randomized, open-label, non-inferiority phase 3 trial carried out in China, a trend toward Pylera® superiority over a standard clarithromycin-based triple therapy was observed (80% vs 55% in the ITT analysis) (23). More recently, a multicenter, open-label, single-arm, multinational study conducted between March 2012 and January 2013 in France, Germany, Italy and Spain reported H. pylori eradication rates that ranged from 93.2% to 93.8% regardless of the definition of eradication (26). Moreover, in another study carried out in France (32), the eradication rates with Pylera® used as a rescue therapy ranged from 83% to 87%.
Pylera® is a three-in-one capsule containing bismuth subcitrate, metronidazole and tetracycline. While resistance to metronidazole and more rarely to tetracycline might influence the efficacy of Pylera®, H. pylori does not appear to develop resistance to bismuth (30). Moreover, it has been proposed that the addition of bismuth to distinct combinations of antibiotics used to eradicate H. pylori completely overcomes any resistance to metronidazole (26). Such an effect might justify why the eradication rates observed in Spain were high, despite the high rate of resistance to metronidazole in this country (17).
Risk factors that are potentially associated with treatment failure were assessed using a conditional risk model. However, no factor was found to be significantly associated with failure in the univariate analysis, thus, a multivariate analysis was not performed. These results differ from those reported previously (32), where eradication failure was associated with male gender and incomplete treatment. The differences between these two studies may reflect the possible differences in the populations studied.
During the study, 46% of patients reported AEs and gastrointestinal disorders were the most common, although symptoms of the nervous system affected 17% of patients and primarily involved asthenia. These results are consistent with the currently available evidence (20-27).
This study has inherent limitations regarding the interpretation of the results, mainly due to the fact that it is an open-label, non-randomized, non-controlled study by design. Thus, the study design does not allow us to reach decisive conclusions on the comparative efficacy and safety of the BMTO therapy. Nevertheless, as patients with frequent co-morbidities were excluded (e.g., diabetes) and the cohort includes a representative and varied sample of patients, the results of the study are likely to be relevant to current clinical practice. Indeed, the results obtained are in accordance with the findings of the previous randomized studies involving BMTO therapies (20,21,24). Nevertheless, as the study was carried out in a limited geographical region, some caution should be taken when reaching general conclusions based on the data obtained. Additional studies should be performed in other populations to confirm these results.
In conclusion, in this setting a ten day treatment with Pylera® produces high rates of H. pylori eradication, not only as a first line therapy but also as a rescue therapy. In addition, Pylera® was generally well tolerated.
Acknowledgements
The authors wish to thank Allergan Laboratories for their collaboration and assistance with the medical writing. It should be noted that Allergan S.A. was not involved in the preparation of the manuscript nor did the company influence in any way the scientific conclusions reached. Editorial assistance in the preparation of this manuscript was provided by Antonio Martínez MD (Ciencia y Deporte S.L.) and Dr Mark Sefton (BiomedRed S.L.). Support for this assistance was funded by Allergan S.A.
References
1. Calvet X, Ramírez Lázaro MJ, Lehours P, et al. Diagnosis and epidemiology of Helicobacter pylori infection. Helicobacter 2013;18(Suppl 1):5-11. DOI: 10.1111/hel.12071. [ Links ]
2. Mentis A, Lehours P, Mégraud F. Epidemiology and diagnosis of Helicobacter pylori infection. Helicobacter 2015;20(Suppl 1):1-7. DOI: 10.1111/hel.12250. [ Links ]
3. Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 2001; 345(11):784-9. DOI: 10.1056/NEJMoa001999. [ Links ]
4. McColl KE. Clinical practice. Helicobacter pylori infection. N Engl J Med 2010;362:1597-604. DOI: 10.1056/NEJMcp1001110. [ Links ]
5. Gisbert JP, Romano M, Gravina AG, et al. Helicobacter pylori second-line rescue therapy with levofloxacin- and bismuth-containing quadruple therapy, after failure of standard triple or non-bismuth quadruple treatments. Aliment Pharmacol Ther 2015;41(8):768-75. DOI: 10.1111/apt.13128. [ Links ]
6. Safavi M, Sabourian R, Foroumadi A. Treatment of Helicobacter pylori infection: Current and future insights. World J Clin Cases 2016;4(1):5-19. DOI: 10.12998/wjcc.v4.i1.5. [ Links ]
7. Malfertheiner P, Megraud F, O'Morain C. Current concepts in the management of Helicobacter pylori infection: The Maastricht III Consensus Report. Gut 2007;56:772-81. DOI: 10.1136/gut.2006.101634. [ Links ]
8. Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol 2007;102:1808-25. DOI: 10.1111/j.1572-0241.2007.01393.x. [ Links ]
9. Olokoba AB, Obateru OA, Bojuwoye MO. Helicobacter pylori eradication therapy: A review of current trends. Niger Med J 2013;54:1-4. DOI: 10.4103/0300-1652.108884. [ Links ]
10. Megraud F, Coenen S, Versporten A, et al; Study Group participants. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut 2013;62(1):34-42. DOI: 10.1136/gutjnl-2012-302254. [ Links ]
11. Lv ZF, Wang FC, Zheng HL, et al. Meta-analysis: Is combination of tetracycline and amoxicillin suitable for Helicobacter pylori infection? World J Gastroenterol 2015;21(8):2522-33. DOI: 10.3748/wjg.v21.i8.2522. [ Links ]
12. Laine L, Fennerty MB, Osato M, et al. Esomeprazole-based Helicobacter pylori eradication therapy and the effect of antibiotic resistance: Results of three US multicenter, double-blind trials. Am J Gastroenterol 2000;95(12):3393-8. DOI: 10.1111/j.1572-0241.2000.03349.x. [ Links ]
13. Vakil N, Lanza F, Schwartz H, et al. Seven-day therapy for Helicobacter pylori in the United States. Aliment Pharmacol Ther 2004;20(1):99-107. DOI: 10.1111/j.1365-2036.2004.02029.x. [ Links ]
14. Seddik H, Ahid S, El Adioui T, et al. Sequential therapy versus standard tripledrug therapy for Helicobacter pylori eradication: A prospective randomized study. Eur J Clin Pharmacol 2013;69:1709-15. DOI: 10.1007/s00228-013-1524-6. [ Links ]
15. Gisbert JP, Molina-Infante J, Amador J, et al. IV Conferencia Española de Consenso sobre el tratamiento de la infección por Helicobacter pylori. Gastroenterol Hepatol 2016;pii:S0210-5705(16)30058-9. DOI: 10.1016/j.gastrohep.2016.05.003. [ Links ]
16. Malfertheiner P, Megraud F, O'Morain CA, et al; European Helicobacter and Microbiota Study Group and Consensus panel. Management of Helicobacter pylori infection-the Maastricht V/Florence Consensus Report. Gut 2016;pii:gutjnl-2016-312288. DOI: 10.1136/gutjnl-2016-312288. [ Links ]
17. Molina-Infante J, Gisbert JP. Actualización de la eficacia de la terapia triple para la infección por Helicobacter pylori y de la resistencia a claritromicina en España (2007-2012). Gastroenterol Hepatol 2013;36(6):375-81. DOI: 10.1016/j.gastrohep.2013.02.006. [ Links ]
18. Graham DY, Lu H, Yamaoka Y. Therapy for Helicobacter pylori infection can be improved: Sequential therapy and beyond. Drugs 2008;68:725-36. DOI: 10.2165/00003495-200868060-00001. [ Links ]
19. Dos Santos AA, Carvalho AA. Pharmacological therapy used in the elimination of Helicobacter pylori infection: A review. World J Gastroenterol 2015;21:139-54. DOI: 10.3748/wjg.v21.i1.139. [ Links ]
20. O'Morain C, Borody T, Farley A, et al; International multicentre study. Efficacy and safety of single-triple capsules of bismuth biskalcitrate, metronidazole and tetracycline, given with omeprazole, for the eradication of Helicobacter pylori: An international multicentre study. Aliment Pharmacol Ther 2003;17(3):415-20. DOI: 10.1046/j.1365-2036.2003.01434.x. [ Links ]
21. Laine L, Hunt R, El-Zimaity H, et al. Bismuth-based quadruple therapy using a single capsule of bismuth biskalcitrate, metronidazole, and tetracycline given with omeprazole versus omeprazole, amoxicillin, and clarithromycin for eradication of Helicobacter pylori in duodenal ulcer patients: A prospective, randomized, multicenter, North American trial. Am J Gastroenterol 2003;98(3):562-7. DOI: 10.1111/j.1572-0241.2003.t01-1-07288.x. [ Links ]
22. Saleem A, Qasim A, O'Connor HJ, et al. Pylera for the eradication of Helicobacter pylori infection. Expert Rev Anti Infect Ther 2009;7(7):793-9. DOI: 10.1586/eri.09.55. [ Links ]
23. Sun Q, Liang X, Zheng Q, et al. High efficacy of 14-day triple therapy-based, bismuth-containing quadruple therapy for initial Helicobacter pylori eradication. Helicobacter 2010;15(3):233-8. DOI: 10.1111/j.1523-5378.2010.00758.x. [ Links ]
24. Malfertheiner P, Bazzoli F, Delchier JC, et al; Pylera Study Group. Helicobacter pylori eradication with a capsule containing bismuth subcitrate potassium, metronidazole, and tetracycline given with omeprazole versus clarithromycin-based triple therapy: A randomised, open-label, non-inferiority, phase 3 trial. Lancet 2011;377(9769):905-13. DOI: 10.1016/S0140-6736(11)60020-2. [ Links ]
25. Uygun A, Ozel AM, Yildiz O, et al. Comparison of three different second-line quadruple therapies including bismuth subcitrate in Turkish patients with non-ulcer dyspepsia who failed to eradicate Helicobacter pylori with a 14-day standard first-line therapy. J Gastroenterol Hepatol 2008;23:42-5. [ Links ]
26. Liang X, Xu X, Zheng Q, et al. Efficacy of bismuth-containing quadruple therapies for clarithromycin-, metronidazole-, and fluoroquinolone-resistant Helicobacter pylori infections in a prospective study. Clin Gastroenterol Hepatol 2013;11(7):802-7.e1. DOI: 10.1016/j.cgh.2013.01.008. [ Links ]
27. Delchier JC, Malfertheiner P, Thieroff-Ekerdt R. Use of a combination formulation of bismuth, metronidazole and tetracycline with omeprazole as a rescue therapy for eradication of Helicobacter pylori. Aliment Pharmacol Ther 2014;40(2):171-7. DOI: 10.1111/apt.12808. [ Links ]
28. Hsu PI, Chen WC, Tsay FW, et al; Taiwan Acid-Related Disease (TARD) Study Group. Ten-day quadruple therapy comprising proton-pump inhibitor, bismuth, tetracycline, and levofloxacin achieves a high eradication rate for Helicobacter pylori infection after failure of sequential therapy. Helicobacter 2014;19(1):74-9. DOI: 10.1111/hel.12085. [ Links ]
29. Gisbert JP, Pérez-Aisa A, Rodrigo L, et al. Third-line rescue therapy with bismuth-containing quadruple regimen after failure of two treatments (with clarithromycin and levofloxacin) for H. pylori infection. Dig Dis Sci 2014;59:383-9. DOI: 10.1007/s10620-013-2900-x. [ Links ]
30. Malfertheiner P. Infection: Bismuth improves PPI-based triple therapy for H. pylori eradication. Nat Rev Gastroenterol Hepatol 2010;7:538-9. DOI: 10.1038/nrgastro.2010.131. [ Links ]
31. Malfertheiner P, Link A, Selgrad M. Helicobacter pylori: Perspectives and time trends. Nat Rev Gastroenterol Hepatol 2014;11:628-38. DOI: 10.1038/nrgastro.2014.99. [ Links ]
32. Muller N, Amiot A, Le Thuaut A, et al. Rescue therapy with bismuth-containing quadruple therapy in patients infected with metronidazole-resistant Helicobacter pylori strains. Clin Res Hepatol Gastroenterol 2016;40(4):517-24. DOI: 10.1016/j.clinre.2015.12.012. [ Links ]
![]() Correspondence:
Correspondence:
Blas José Gómez-Rodríguez.
Clinical Management Unit of the Gastroenterology Department.
Hospital Universitario Virgen Macarena.
Av. Doctor Fedriani, 3.
41009 Sevilla, Spain
e-mail: gomezblasj@gmail.com
Received: 29-12-2016
Accepted: 08-03-2017











 text in
text in