My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.9 Madrid Sep. 2017
https://dx.doi.org/10.17235/reed.2017.4972/2017
EUS-guided recanalization of complete gastrointestinal strictures
Miguel Martínez-Guillén1,2, Joan B. Gornals1,4, Claudia F. Consiglieri1, Josep M. Castellvi2 and Carme Loras3,4
1Endoscopy Unit. Department of Digestive Diseases. Hospital Universitari de Bellvitge-IDIBELL. Barcelona, Spain.
2Digestive Diseases Department. Hospital de Mataró del Consorci Sanitari del Maresme. Mataró, Barcelona. Spain.
3Endoscopy Unit. Centre Mèdic Teknon. Barcelona. Endoscopy Unit. Hospital Universitari Mútua de Terrassa-CIBERehd. Terrassa, Barcelona. Spain.
4Faculty of Health Sciences. Universitat Oberta de Catalunya. Barcelona, Spain
Authors' contributions: All authors were involved in all stages of the manuscript development: the conception and design, analysis and interpretation of the data, drafting of the article, critical revision and final approval.
ABSTRACT
Background and aim: Complete gastrointestinal strictures are a technically demanding problem. In this setting, an anterograde technique is associated with a high risk of complications and a combined anterograde-retrograde technique requires a prior ostomy. Our aim was to assess the outcome of a first case series for the management of complete gastrointestinal strictures using endoscopic ultrasound (EUS)-guided puncture as a novel endoscopic approach.
Patients and methods: This retrospective case-series describes four cases that were referred for treatment of complete benign gastrointestinal strictures, three upper and one lower. Recanalization was attempted with EUS-guided puncture using a 22G or 19G needle and contrast filling was visualized by fluoroscopy. Afterwards, a cystotome and/or a dilator balloon were used under endoscopic and fluoroscopic guidance. A fully covered metal stent was placed in two cases, keeping the strictures open in order to prevent another stricture. Feasibility, adverse events, efficacy and the number of dilations required after recanalization were evaluated.
Results: Technical and clinical success was achieved in three of the four cases (75%). A first dilation was performed using a dilator balloon in all successful cases and fully covered metal stents were used in two cases. These patients underwent a consecutive number of balloon dilatations (range 1-4) and all three were able to eat a soft diet. No adverse events were related to the EUS-guided approach. In the failed case with a long stricture (> 3 cm), an endoscopic rendezvous technique was attempted which caused a pneumothorax requiring a chest tube placement.
Conclusion: EUS-guided recanalization, as a first approach in the treatment of complete digestive stricture, is a feasible and promising procedure that can help to avoid major surgery.
Key words: Endosonography. Therapeutics. Complete stricture. Stenosis. Recanalization.
Introduction
Benign strictures can occur throughout the gastrointestinal (GI) tract although they are most common in the esophagus. They are usually managed with endoscopic dilation with or without stent placement or surgical treatment. However, when they progress to complete obstruction of the lumen this becomes a technically demanding problem (1). In this setting, anterograde techniques are associated with a high risk of perforation or hemorrhage. A combined anterograde-retrograde technique is another option that has been described in a few short case series. This endoscopic rendezvous approach seems to be effective but requires a prior ostomy, two endoscopic devices and two endoscopists (1-3). Our aim was to report the outcomes of a first case series for managing complete gastrointestinal strictures using endoscopic ultrasound (EUS)-guided puncture as a new endoscopic approach.
Patients and methods
Four patients who were referred with complete benign stenosis of the digestive tract (three upper and one lower stricture) were consecutively treated with a novel endoscopic approach at a tertiary hospital. The period of inclusion was from November 2012 to June 2015. Technical success was defined as digestive lumen restoration by EUS-guidance. Clinical success was defined as normal functioning of the digestive tract and restored normal GI habits. Feasibility, adverse events (AE), efficacy and the number of dilations required after recanalization were evaluated. Only AE related with the EUS-guided approach were considered.
Technique
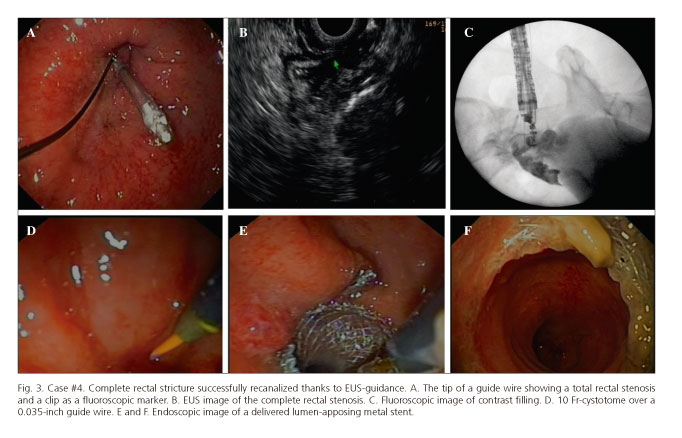
All the procedures were performed under general anesthesia. Written informed consent was obtained for EUS-guided intervention. In all cases, repermeabilization was attempted under endosonography guidance (Figs. 1-3).
A linear echoendoscope was advanced to the end, or cul-de-sac, of the stricture. It is important to note that the other end (distal or proximal GI lumen) of the stricture was identified by EUS following the muscularis propria of the digestive wall. An EUS-guided puncture was performed with a 22G (Expect, BostonSc, Natick, MA, USA) or 19G needle (Expect Flex), contrast filling was visualized by fluoroscopy and a guide wire (0.018; 0.025; 0.035-inch) was passed through the GI stricture. Afterwards, a cystotome and/or a dilator balloon (8, 10 or 12 mm) were used under endoscopic and fluoroscopic guidance. A fully covered metal stent (Niti-S-EnteralColonic, Taewoong; AXIOS 15-10-mm, Xlumena) was placed in two cases, keeping the strictures open in order to prevent repeat stricturing.
All cases were monitored and admitted to our center for clinical observation. Patients were followed-up at the clinical and endoscopic level during dilation sessions.
Results
General outcomes are summarized in table 1. This retrospective case series included four patients (mean age of 52 years) with complete digestive tract stricture, two esophageal (radiation-induced), one gastric (post-bariatric surgery) and one rectal (surgical anastomosis). EUS-guided recanalization was successful in three of the four cases and all three patients were able to eat a soft diet. Thus, the technical and clinical success was 75%. With regard to the successful cases, only one session was required to achieve repermeabilization. No adverse events were related with the EUS-guided approach.
Patient #1 required a total of four dilation sessions to achieve an esophageal lumen diameter of 15 mm. The patient responded well and was able to swallow secretions and to eat a soft diet (4).
With regard to patient #2, the EUS-guided recanalization was attempted, but after several punctures it was impossible to access the distal lumen due to a long esophageal stricture (> 3 cm). No adverse events were reported with this first procedure. A second endoscopic approach was performed with a combined antegrade-retrograde rendezvous technique using a needle-knife. Subcutaneous emphysema was observed during the procedure and the technique was stopped. A CT scan revealed a pneumothorax and pneumomediastinum. A chest tube was placed and the patient had a favorable clinical course. The patient is well and has requested a repeat attempt at endoscopic recanalization.
An enteral fully covered metal stent was placed during the same EUS-guided approach in patient #3. On day four, this stent had migrated to the small bowel, and enteroscopy was performed in order to rescue this stent. No further dilation sessions were needed and the oral diet was reinitiated without problems to date.
Finally, a lumen-apposing metal stent was placed during the EUS-guided reacanalization procedure and maintained for four weeks in patient #4. Two dilation sessions of up to 15 and 18 mm with hydrostatic balloons were required in the following 2-4 weeks. Surgical reconstruction was performed with no incidents and normal bowel habits were restored (4).
Discussion
Complete GI obstructions are rare and can be very challenging. A combined anterograde-retrograde dilation technique that has been described in some case series is a viable option. However, this requires retrograde access via a prior ostomy as well as two endoscopists and two endoscopic towers with two scopes (1,2). Thus, the use of EUS-guidance might be an optimal procedure as it requires only one endoscopist and one endoscopic device and it is a minimally invasive intervention.
We report a novel and pioneering first case series of complete digestive strictures treated with EUS-guidance. In this approach, only one interventional endoscopist is needed and no ostomy is required for the recanalization. In this case series, only one AE was reported and it was related to a combined antegrade/retrograde technique after a failed EUS-guided attempt.
Previous isolated experiences presented as case reports have described the use of special endoscopic catheters or needle-knife under scan tomography guidance (5,6). However, reports of EUS-guided puncture as a therapeutic approach in complete obstruction are unreliable. De Lusong et al. first described this approach in a complete colon anastomotic stricture case using a prototype forward-array echoendoscope facilitated with a SpyGlass probe (7). Artifon et al. also described an EUS-guided recanalization of a complete colorectal postoperative stricture in an infant with Hirschsprung's disease using a partially covered biliary metal stent (8). Finally, Saxena et al. reported a case of EUS-guided rendezvous of complete rectal anastomotic stenosis after Hartman's reversal, although they used a colonoscope and an echoendoscope at the same time. No complications were reported in any of these cases (9).
Our group has had previous success using both techniques, rendezvous and/or EUS-guided puncture for complete upper GI stenosis. Some of these have been published as case reports (3,4,10). We prefer a direct EUS-guided puncture instead of a rendezvous technique, as this eliminates the need for two endoscopic devices and it is also less time-consuming. It is important to note that we were able to access the distal (or proximal) lumen by following the muscularis propria. This is an important technical consideration for a successful outcome.
The strength of this new EUS guided approach is its novelty and feasibility. In cases of failure, it does not preclude other endoscopic techniques such as rendezvous dilation. However, our study has some limitations. The current case series is a retrospective study with a small sample size (n = 4). In addition, the technical demands of the EUS-guided puncture in reaching the GI lumen after the stricture and the risk of stent migration are two important concerns. It requires previous expertise in EUS-guided puncture and a preference for the use of stents especially designed to prevent migrations.
In summary, EUS-guided recanalization of complete GI stricture is feasible and may prevent the need for more invasive procedures such as surgery.
References
1. Dellon ES, Cullen NR, Madanick RD, et al. Outcomes of a combined antegrade and retrograde approach for dilatation of radiation-induced esophageal strictures (with video). Gastrointest Endosc 2010;71:1122-9. DOI: 10.1016/j.gie.2009.12.057. [ Links ]
2. González JM, Vanbiervliet G, Gasmi M, et al. Efficacy of the endoscopic rendez-vous technique for the reconstruction of complete esophageal disruptions. Endoscopy. E-pub 2015 Oct 1. DOI: 10.1055/s-0034-1393129. [ Links ]
3. Gornals JB, Nogueira J, Castellvi JM, et al. Combined antegrade and retrograde esophageal endoscopic dilation for radiation-induced complete esophageal stenosis. Dig Endosc 2012;24:483. DOI: 10.1111/j.1443-1661.2012.01342.x. [ Links ]
4. Gornals JB, Consiglieri C, Castellví JM, et al. Treatment of complete esophageal stenosis using endoscopic ultrasound-guided puncture: A novel technique for access to the distal lumen. Endoscopy 2013;45:E1-2. [ Links ]
5. Curcio G, Spada M, Di Francesco F, et al. Completely obstructed colorectal anastomosis: A new non-electrosurgical endoscopic approach before balloon dilatation. World J Gastroenterol 2010;16:4751-4. DOI: 10.3748/wjg.v16.i37.4751. [ Links ]
6. Probst A, Gölder S, Knöpfle E, et al. Computed tomography-guided endoscopic recanalization of a completely obstructed rectal anastomosis. Endoscopy 2015;47:E32-3. DOI: 10.1055/s-0034-1391131. [ Links ]
7. De Lusong MA, Shah JN, Soetikno R, et al. Treatment of a completely obstructed colonic anastomotic stricture by using a prototype forward-array echoendoscope and facilitated by SpyGlass (with videos). Gastrointest Endosc 2008;68:988-92. DOI: 10.1016/j.gie.2008.05.028. [ Links ]
8. Artifon EL, Ferreira F, Baracat R, et al. EUS-guided fistulization of postoperative colorectal stenosis in an infant with Hirschsprung's disease: A new technique. Gastrointest Endosc 2012;75:459-61. DOI: 10.1016/j.gie.2011.03.1241. [ Links ]
9. Saxena P, Azola A, Kumbhari V, et al. EUS-guided rendezvous and reversal of complete rectal anastomotic stenosis after Hartmann's reversal. Gastrointest Endosc 2015;81:467-8. DOI: 10.1016/j.gie.2014.04.055. [ Links ]
10. Gornals JB, Albines G, Trenti L, et al. EUS-guided recanalization of a complete rectal anastomotic stenosis by use of a lumen-apposing metal stent. Gastrointest Endosc 2015;82:752. DOI: 10.1016/j.gie.2015.05.003. [ Links ]
![]() Correspondence:
Correspondence:
Joan B. Gornals.
Endoscopy Unit. Department of Digestive Diseases.
Hospital Universitari de Bellvitge-IDIBELL
(Bellvitge Biomedical Research Institute).
Feixa Llarga, s/n. 08907
L'Hospitalet de Llobregat, Barcelona. Spain
e-mail: jgornals@bellvitgehospital.cat
Received: 03-04-2017
Accepted: 22-05-2017