My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.10 Madrid Oct. 2017
https://dx.doi.org/10.17235/reed.2017.4732/2016
REVIEW
Per-oral endoscopic myotomy (POEM): a new endoscopic treatment for achalasia
Pablo Miranda-García1, Fernando Casals-Seoane1, Jean-Michel Gonzalez2, Marc Barthet2 and Cecilio Santander-Vaquero1
1Gastroenterology Department. Hospital Universitario La Princesa. Madrid, Spain.
2Gastroenterology Department. Hôpital Nord. Université Aix-Marseille. Marseille, France
ABSTRACT
Background/aims: Per-oral endoscopic myotomy (POEM) is a new minimally invasive technique to treat achalasia.
Methods: We performed a review of the literature of POEM with a special focus on technical details and the results obtained with this technique in patients with achalasia and other esophageal motility disorders.
Results: Thousands of POEM procedures have been performed worldwide since its introduction in 2008. The procedure is based on the creation of a mucosal entry point in the proximal esophagus to reach the cardia through a submucosal tunnel and then perform a myotomy of the muscular layers of the cardia, esophagogastric junction and distal esophagus, as performed in a Heller myotomy. The clinical remission rate ranges from 82 to 100%. Although no randomized studies exist and available data are from single-center studies, no differences have been found between laparoscopic Heller myotomy (LHM) and POEM in terms of perioperative outcomes, short-term outcomes (12 months) and long-term outcomes (up to three years). Procedure time and length of hospital stay were lower for POEM. Post-POEM reflux is a concern, and controversial data have been reported compared to LHM. The technique is safe, with no reported deaths related to the procedure and an adverse event rate comparable to surgery. Potential complications include bleeding, perforation, aspiration and insufflation-related adverse events. Thus, this is a complex technique that needs specific training even in expert hands. The indication for this procedure is widening and other motor hypercontractil esophageal disorders have been treated by POEM with promising results. POEM can be performed in complicated situations such as in pediatric patients, sigmoid achalasia or after failure of previous treatments.
Conclusions: POEM is an effective treatment for achalasia and is a promising tool for other motor esophageal disorders. It is a safe procedure but, due to its technical difficulty and possible associated complications, the procedure should be performed in referral centers by trained endoscopists.
Key words: Per-oral endoscopic myotomy. Heller myotomy. Achalasia.
Introduction
Achalasia is an esophageal motility disorder characterized by an incomplete or absent lower esophageal sphincter relaxation associated with an abnormal peristalsis in response to swallowing. Classic treatment of achalasia aims to diminish the lower esophageal sphincter pressure, and different approaches have been used, including pharmacological therapy, endoscopic injection of botulinum toxin or pneumatic dilation and surgical myotomy.
Per-oral endoscopic myotomy (POEM) is an innovative, minimally invasive endoscopic treatment for achalasia first described by Inoue et al. (1) in 2008, after the preclinical description by Pasricha et al. in an animal model (2). Since its introduction, thousands of POEM procedures have been performed and indications have been extended to include the three types of achalasia and other spastic esophageal motility disorders.
There is no standard technique adopted by all centers and even the peri-procedural management varies from one center to another. Although good outcomes and excellent efficacy and safety are commonly reported, the rates of clinical success and adverse events vary among centers.
We present the technical aspects of this new technique and review the outcome, safety and results according to published data.
Indications
The main indication for POEM is achalasia. However, due to its intraluminal route, which allows the length, position and direction of the myotomy to be chosen, its indications are widening. Esophagogastric junction (EGJ) outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, nutcracker esophagus and failed surgical or endoscopic cases have been successfully treated with POEM (3-7). Nonetheless, improvement in chest pain and dysphagia in hypercontractile disorders after POEM seems to be less evident compared to symptom relief in patients suffering from achalasia type I and II.
Table 1 shows some accepted contraindications to POEM according to the responses to an international survey about the procedure (IPOEMS) from experts (8).
Pre-operative evaluation
Although some centers perform a barium esophagogram in order to study the dynamics of the esophagus such as the site of abnormal contractions, simultaneous contractions and barium accumulation (9), esophageal manometry is the gold standard to determine esophageal motility and it should be always performed to confirm the diagnosis and to define the best therapeutic approach (10). It can also be used to evaluate response to treatment. High-resolution manometry represents an unquestionable advance in esophageal motility assessment, allowing for a better characterization of esophageal disorders (11). The Chicago classification should be used to determine the type of esophageal motor disease (12). Obviously, previous treatments for achalasia and patient comorbidities should be identified in order to select good candidates for this procedure. Preoperative evaluation including ASA assessment by an anesthesiologist is advisable in order to prevent intraoperative adverse events. Some precautions must be taken, for example, achalasia patients are at increased risk of aspiration during intubation due to the presence of esophageal content. The anesthesiologist should be aware of this condition and airway protection methods should be routinely used.
Poem technique
Many centers perform an esophagogastroduodenoscopy (EGD) one to three days before the procedure in order to remove any residual material from the esophagus. However, fasting for at least 24 hours should be recommended before the procedure. POEM is performed under general anesthesia with airway intubation. There is no evidence in support of using either the left lateral or supine position; however, some experts recommend the supine position as it results in a more neutral position for the endoscope, thus minimizing the tension in the mucosal flap, and diminishes the angulations in the sigmoid esophagus (13). Broad-spectrum intravenous antibiotics are given before the procedure.
A forward-viewing endoscope with CO2 insufflation is used. A transparent plastic cap is attached to the tip of the endoscope. Before beginning the procedure, the gastroesophageal junction (GEJ) must be identified and its distance to the incisors should be determined. The anatomical landmarks such as the upper and lower esophageal sphincters, spine, trachea, left main bronchus and the aortic arch help to orient the operator during the procedure. Subsequently, the procedure is carried out as follows.
Mucosotomy
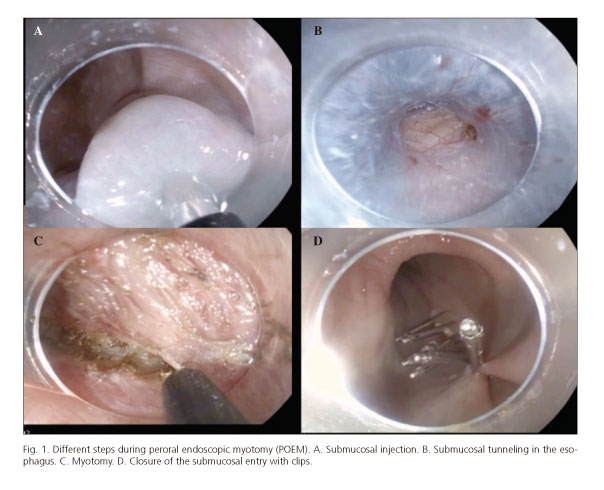
The site of submucosal entry is chosen between 10 and 15 cm proximal to the GEJ. Two different approaches have been proposed: the right-anterior orientation (11-2 o'clock) method, which is the most commonly used procedure (used by Inoue in his first 500 hundred cases) (1,14), and the posterolateral orientation (5 o'clock) approach (8). There is no evidence to define the best approach, although some practitioners think that the posterior method is more effective to reduce dysphagia and the anterior path may reduce reflux after POEM. Injection of approximately 10 cc of saline solution stained with indigo carmine is used to create a bleb in the mucosa (Fig. 1A). Subsequently, a 2 cm longitudinal incision of the mucosa (mucosotomy) is performed with a cutting current to expose the submucosal space (13) with the following parameters: dry cut mode 50 W, effect 3 (9) or with the following parameters if the ERBE300D is used: endocut 1, effect 1, duration 1, interval 3 (13).
Submucosal tunneling
A technique similar to endoscopic submucosal dissection is used to create a submucosal tunnel from the esophagus to 2-3 cm beyond the EGJ (Fig. 1B). Different devices and techniques have been described. The T-Type Hybrid Knife (ERBE, Tübingen, Germany) showed (16) a shorter procedure time, a lower bleeding rate and less frequent use of coagulation forceps to control bleeding compared to the most preferred Triangle-Tip Knife (Olympus Medical Systems, Tokyo, Japan) in a head to head prospective study. Other new devices such as the water-jet assisted triangle-tip knife have been developed to reduce procedure time (17). Experts recommend maintaining the dissection in proximity to the muscular layer to avoid injury of the mucosa and keeping the circular muscle bundles perpendicular to the endoscope to ensure progression in the desired direction (13). Some indicators to confirm that the GEJ has been reached have been described. These include the narrowing of the submucosal space as well as the presence of an increased vascularity with "spindle" shaped veins and the visualization of a blue hue on intraluminal inspection of the mucosa of the gastric cardia. The previous endoscopic measurements can be used and other anatomical changes should be checked, such as the presence of aberrant longitudinal muscle bundles at the GEJ, the presence of large perforating vessels in the cardia and palisading vessels at the distal end of the esophagus. For this step, soft coagulation mode 40-60 W, effect 1-2 is recommended (9,13,15).
Myotomy
Most endoscopists perform a selective dissection of the circular muscle alone, in a proximal to distal direction, starting at 2-3 cm above the mucosal entry. However, some centers use a distal to proximal direction and dissect both circular and longitudinal muscle layers, especially at the level of the lower esophageal sphincter (8,15) (Fig. 1C). One retrospective study found no differences in efficacy, GERD or adverse events, although the procedural time was shorter in the full thickness myotomy group (18). To avoid massive bleeding from the intramuscular vessels, spray coagulation current is recommended (40-60 W, effect 1-2). With regard to the Heller myotomy, the dissection in POEM is continued to 2-3 cm within the cardia for a total length of 8-10 cm, including the esophageal myotomy, lower esophageal sphincter and cardia myotomy. To ensure an adequate length of the myotomy, identification of the anatomical landmarks of the GEJ inside the tunnel is useful. The easy passage of the endoscope into the lumen without difficulty at the level of the lower esophageal sphincter (LES) is consistent with a good myotomy, and the integrity of the mucosa must be verified at the same time. However, Grimes et al. have recently proposed the use of a second ultra-slim endoscope to observe the transillumination at the end of the tunnel in the cardia from the stomach (19,20).
Closure of the mucosal entry
To avoid a potential leakage of luminal content into the tunnel and mediastinum, the entry is closed with hemostatic clips (Fig. 1D). Alternative methods of closure include endoscopic sutures (Overstitch, Apollo, Austin, TX), over-the-scope clips (Ovesco, Tübingen, Germany) or fully covered metal stents. Some authors use a prophylactic antibiotic solution which is sprayed into the tunnel before closing the mucosa. The clips must be deployed symmetrically and the first clip must be deployed beyond the distal margin of the incision in order to create a symmetrical fold that will allow an easier closure which requires less clips (13), which diminishes the risk of pocket formation and tunnel infection (21).
Patients are hospitalized after the procedure. Twenty-four hours of fasting is recommended before starting a clear water intake on day 1 provided that the esophagogram with gastrografin (Bracco Diagnostics Inc., Princeton, NJ) and/or EGD confirm the absence of leaks and ischemic or hemorrhagic complications. On day 2, a soft diet can be started and maintained for some days and then a regular diet can be safely introduced. During hospitalization, intravenous antibiotics are administrated and then oral medication given (if the patient is discharged) until completion of a ten-day treatment. The postoperative hospitalization length after POEM is 3.6 ± 0.38 days.
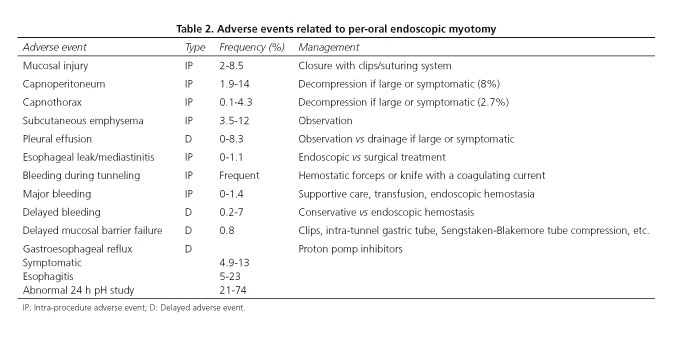
Adverse events in poem
Table 2 summarizes adverse events (AE) related to POEM, their frequencies and management. CO2 insufflation is mandatory. Ventilation with positive pressure helps to avoid complications related to gas insufflation such as a pneumothorax, pneumomediastinum, pneumoperitoneum, subcutaneous emphysema, etc. Even if these measures are taken, the escape of gas into the mediastinum, thorax and abdomen is common, and CO2 flow should be set as low as possible and the operator should avoid excessive insufflation especially while in the tunnel.
Bleeding during the creation of the tunnel is frequent and can usually be managed with endoscopic treatment. Pulsed irrigation, gentle suction and tamponade might help to recover visibility, and the bleeding vessel can be selectively coagulated with coagulation forceps (13) or with the tip of the knife. Bleeding is more frequent at the GEJ and cardia.
Mucosal perforation during tunneling must be avoided and perforations should be immediately closed with clips to prevent leakage of esophageal contents into the tunnel. If a full-thickness myotomy is present at the level of the mucosal entry, the use of over-the-scope-clips has been proposed to ensure a complete and safer closure (22).
Postoperative adverse events include mediastinitis caused by esophageal leakage. This is an uncommon but major complication of POEM and it often requires surgical drainage. Delayed hemorrhage incidence is low (16,23,24) and can be managed conservatively in most cases by observation and transfusion. Some authors advocate the use of Blakemore-Sengstaken tubes for EGD management (25) or tamponade (25,26) but others are concerned about the risk of continuous bleeding into the mediastinum or peritoneum when a complete myotomy has been performed, as there is no barrier to prevent this internal hemorrhage (13). Finally, no procedure-related deaths have been reported to date.
Outcomes and efficacy of poem
Global outcomes
POEM has shown its efficacy in both symptom relief and improvement of esophageal motility. Clinical remission after POEM ranges from 82 to 100% (27,28). Table 3 shows the results from the largest POEM studies. There are two meta-analysis (with more than 1,000 patients each) that demonstrate the short-term (one year) efficacy of POEM with both a reduction in the Eckardt score and LES pressure (29,30). Another meta-analysis evaluating 16 prospective and retrospective studies conducted between 2010 and 2013 with a total number of 551 patients suffering from achalasia found a technical and clinical success in 97% (95% CI: 94-98%) and 93% (95% CI: 90-95%) of cases respectively, after a median follow-up of six months (range 3-12). Major adverse events requiring surgical or medical intervention occurred in 14% of cases and only one patient needed post-POEM surgery (31).
Finally, a more recent meta-analysis by Akintoye et al. (32) evaluated the results from 36 studies which included 2,373 patients. An Eckardt score of 3 or less was achieved in 98% of cases (95% CI: 97-100%), and symptoms relief was maintained at 1.6 and 12 months after treatment. They also found a significant decrease in the lower esophageal sphincter pressure and integrated relaxation pressure from 33 ± 1.7 and 30 ± 1.4 mmHg to 14 ± 1.2 and 13 ± 1.6 mmHg respectively within six months of the procedure (p < 0.05). Perioperative adverse events were frequent; these included mucosal injury (4.8%), esophageal perforation (0.2%), bleeding requiring intervention (0.2%), subcutaneous emphysema (7.5%), pneumothorax (1.2%), pleural effusion (1.2%), pneumomediastinum (1.1%) and pneumoperitoneum (6.8%).
Long-term follow-up
One cohort of 500 patients with at least three years of follow-up showed that the overall success was maintained over time (88.5%) in this study (14).
POEM versus laparoscopic Heller myotomy
There are only a few studies comparing POEM with historical laparoscopic Heller myotomy (LHM) controls (33-36). The results for both procedures were similar with regard to complications and clinical success rates; however, operative times, blood loss, postoperative pain, hospital stay and return to normal activity tended to be better after POEM. A meta-analysis by Marano et al. (37) investigated the efficacy and safety of POEM compared with LHM in 486 patients (196 in the POEM group and 290 in the LHM group). Outcomes were comparable with no significant differences in both groups with regard to clinical improvement, operative time, post-operative pain scores, analgesic requirements and complications. The length of hospital stay was significantly shorter for POEM. Remarkably, the quality of most of the studies included in this meta-analysis was poor due to the fact that the patients were not randomized, the patients included were treatment naïve or non-responders, and the follow-up was less than a year in all the cases.
Type III achalasia might be especially challenging due to its spastic nature and low incidence. Kumbhari et al. (38) compared the outcomes after POEM and LHM in patients with type III achalasia in a retrospective multicenter study. They found that the clinical response was more frequent in the POEM cohort (98% vs 80.8%; p = 0.01), with a shorter procedure time for POEM even if the myotomy length was longer. The author hypothesizes that a longer myotomy with POEM may result in improved clinical outcome in this type of achalasia where spastic contractions are found.
The current treatment for other hypercontractile esophageal motility disorders is challenging due to the inefficacy of pharmacological and endoscopic treatment, with failure rates above 70% (39). The potential need of a thoracoscopic approach to perform an extended surgical myotomy and its suboptimal success rates (69-86%) make it important to find new treatments for these entities. POEM has many potential benefits, such as the possibility to choose the length or the orientation of the myotomy in order to treat these disorders (40-42). Indeed, several case-reports and small series have been performed where POEM has shown good results in treating DES, jackhammer esophagus and nutcracker esophagus (4-6,43-45). In contrast, Sharata et al. found that complete dysphagia relief was better in achalasia patients than in other hypercontractile disorders (46/47 patients; 97% vs 17/24 patients; 70%) (7).
Post-POEM gastroesophageal reflux
The rate of reflux after POEM ranges from 5.7% to more than 50% depending on the series (46-49). Objective reflux confirmed on endoscopy or pH study is estimated to be between 20-46%; these rates are similar rates to LHM (33,50,51). The meta-analysis of Akintoye et al. (32) showed rates of symptomatic reflux, esophagitis on endoscopy and abnormal acid exposure during 24h of pH monitoring of 8.5% (CI 95%: 4.9-13%), 13% (CI 95%: 5-23%) and 47% (CI 95%: 21-74%), respectively. Two meta-analyses found no statistically significant differences between reflux rates after LHM and POEM (29,31). However, there is a concern about POEM and GERD due to the absence of an anti-reflux associated procedure in POEM compared with the systematic fundoplication during LHM. It is thought that many asymptomatic patients after POEM may have abnormal acid exposure. Familiari et al. (52) and Jones et al. (53) described the absence of a correlation between GERD symptoms and acid exposure after POEM. In the former study, acid exposure was elevated in 50% of patients, 20% had esophagitis (including 5.8% of grade C or D esophagitis) whereas only 18% complained about GERD symptoms.
There is no evidence-based recommendation with regard to handling this situation after POEM, but experts use two strategies. These are routine proton pump inhibitor (PPI) use after treatment or endoscopic follow-up in order to rule out the development of significant esophagitis before starting PPI therapy (54).
Special situations and future perspectives
POEM has been successfully used in patients with sigmoid-type 2 achalasia where the lumen of the tortuous esophagus turns upwards, a situation that was initially considered to be a contraindication for POEM (55-57). However, more technical difficulties may appear and some authors recommend posterior or bilateral POEM to increase the rates of success, although further experience and evidence is needed (56).
Failure after surgical myotomy is another difficult clinical situation that may be solved with POEM. Although uncommon, recurrence after surgery due to incomplete myotomy, scarring, fibrosis, tight fundoplication or progression of disease is a challenging scenario if a redo Heller myotomy is attempted. In contrast, POEM has shown good results in this situation where the myotomy is performed at the opposite axis to the previous myotomy in order to avoid scars and fibrosis. No complications were reported and the rates of success reached 90% (3,58).
In the case of a failed POEM, re-performing the procedure in the opposite direction is recommended. However, it is important to note that LHM is an option, as POEM does not involve adjacent tissues surrounding the esophagus (59).
Pediatric achalasia patients have also been treated with POEM in some centers with a minimum age of three years (60,61). There are several series in pediatric patients that show similar results and safety to that in adult patients (62,63).
As a result of the acceptance of POEM in the treatment of achalasia, a similar tunneling approach has recently been proposed as an alternative to surgical pyloroplasty to treat dysfunctions of the pylorus and impaired gastric emptying. Per-oral pylorotomy (POP) would be less invasive than surgery and would have a more durable effect than other endoscopic treatments such us pyloric dilation, botulinium toxin injection or stent placement. Technically, POP is based on the same principles of POEM with the creation of a submucosal tunnel followed by the division of the pyloric sphincter muscles. Since the first two case reports describing the technique in patients with refractory gastroparesia, other prospective series and case reports have been published showing promising results (64-68).
Conclusions
POEM is an effective and safe treatment for achalasia. There are several technical issues that need to be clarified, including the optimal length and location of the myotomy. The management of periprocedural aspects or complications such as post-POEM reflux should be standardized. More evidence is required to establish the role of POEM in the management of achalasia, especially in relation to LHM.
References
1. Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. DOI: 10.1055/s-0029-1244080. [ Links ]
2. Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: A novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761-4. DOI: 10.1055/s-2007-966764. [ Links ]
3. Onimaru M, Inoue H, Ikeda H, et al. Peroral endoscopic myotomy is a viable option for failed surgical esophagocardiomyotomy instead of redo surgical Heller myotomy: A single center prospective study. J Am Coll Surg 2013;217:598-605. DOI: 10.1016/j.jamcollsurg.2013.05.025. [ Links ]
4. Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy (POEM) for diffuse esophageal spasm. Endoscopy 2014;46(Suppl 1)UCTN:E79-E81. DOI: 10.1055/s-0032-1309922. [ Links ]
5. Shiwaku H, Inoue H, Beppu R, et al. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc 2013;77:149-50. DOI: 10.1016/j.gie.2012.02.008. [ Links ]
6. Khashab MA, Messallam AA, Onimaru M, et al. International multicenter experience with peroral endoscopic myotomy for the treatment of spastic esophageal disorders refractory to medical therapy (with video) Gastrointest Endosc 2015;81:1170-7. E-pub 2015 Jan 26. DOI: 10.1016/j.gie.2014.10.011. [ Links ]
7. Sharata A, Kurian AA, Dunst CM, et al. Peroral endoscopic myotomy (POEM) is safe and effective in the setting of prior endoscopic intervention. J Gastrointest Surg 2013;17:1188-92. DOI: 10.1007/s11605-013-2193-6. [ Links ]
8. Stavropoulos SN, Modayil RJ, Friedel D, et al. The International Per Oral Endoscopic Myotomy Survey (IPOEMS): A snapshot of the global POEM experience. Surg Endosc 2013;27:3322-38. DOI: 10.1007/s00464-013-2913-8. [ Links ]
9. Youn YH, Minami H, Chiu PW, et al. Peroral endoscopic myotomy for treating achalasia and esophageal motility disorders. J Neurogastroenterol Motil 2016;22(1):14-24. [ Links ]
10. Ciriza de los Ríos C, García Menéndez L, Díez Hernández A, et al. Role of stationary esophageal manometry in clinical practice. Manometric results in patients with gastroesophageal reflux, dysphagia or non-cardiac chest pain. Rev Esp Enferm Dig 2004;96(9):606-11. DOI: 10.4321/S1130-01082004000900003. [ Links ]
11. Ciriza-de-Los-Ríos C, Canga-Rodríguez-Valcárcel F. High-resolution manometry and impedance-pH/manometry: Novel techniques for the advancement of knowledge on esophageal function and their clinical role. Rev Esp Enferm Dig 2009;101(12):861-9. DOI: 10.4321/S1130-01082009001200006. [ Links ]
12. Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: A new clinically relevant classification by high-resolution manometry. Gastroenterol 2008;135:1526-33. DOI: 10.1053/j.gastro.2008.07.022. [ Links ]
13. Bechara R, Ikeda H, Onimaru M, et al. H. Per-oral endoscopic myotomy, 1000 cases later: Pearls, pitfalls, and practical considerations. Gastrointest Endosc 2016;pii: S0016-5107(16)01763-6. DOI: 10.1016/j.gie.2016.03.1469. [ Links ]
14. Inoue H, Sato H, Ikeda H, et al. Per-oral endoscopic myotomy: A series of 500 patients. J Am Coll Surg 2015;221(2):256-64. E-pub 2015 Apr 11. DOI: 10.1016/j.jamcollsurg.2015.03.057. [ Links ]
15. Stavropoulos SN, Desilets DJ, Fuchs KH, et al. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc 2014;80:1-15. DOI: 10.1016/j.gie.2014.04.014. [ Links ]
16. Cai MY, Zhou PH, Yao LQ, et al. Peroral endoscopic myotomy for idiopathic achalasia: Randomized comparison of water-jet assisted versus conventional dissection technique. Surg Endosc 2014;28:1158-65. DOI: 10.1007/s00464-013-3300-1. [ Links ]
17. Balassone V, Sumi K, Inoue H. Peroral endoscopic myotomy: First human experience with a water-jet-assisted triangle knife. Gastrointest Endosc 2016;83(6):1279. E-pub 2016 Jan 6. DOI: 10.1016/j.gie.2015.12.031. [ Links ]
18. Li QL, Chen WF, Zhou PH, et al. Peroral endoscopic myotomy for the treatment of achalasia: A clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 2013;217(3):442-51. E-pub 2013 Jul 25. DOI: 10.1016/j.jamcollsurg.2013.04.033. [ Links ]
19. Hong HJ, Song GW, Ko WJ, et al. Double-scope peroral endoscopic myotomy (POEM) for esophageal achalasia: The first trial of a new double-scope POEM. Clin Endosc 2016. E-pub ahead of print. DOI: 10.5946/ce.2015.108. [ Links ]
20. Grimes KL, Inoue H, Onimaru M, et al. Double-scope per oral endoscopic myotomy (POEM): A prospective randomized controlled trial. Surg Endosc 2016;30(4):1344-51. E-pub 2015 Jul 15. DOI: 10.1007/s00464-015-4396-2. [ Links ]
21. Li QL, Yao LQ, Xu XY, et al. Repeat peroral endoscopic myotomy: A salvage option for persistent/recurrent symptoms. Endoscopy 2016;48(2):134-40. E-pub 2015 Sep 8. DOI: 10.1055/s-0034-1393095. [ Links ]
22. Kurian AA, Bhayani NH, Reavis K, et al. Endoscopic suture repair of full thickness esophagotomy during per-oral esophageal myotomy for achalasia. Surg Endosc 2013;27:3910. DOI: 10.1007/s00464-013-3002-8. [ Links ]
23. Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: An international prospective multicenter study. Gastroenterol 2013;145:309-11. DOI: 10.1053/j.gastro.2013.04.057. [ Links ]
24. Minami H, Isomoto H, Yamaguchi N, et al. Peroral endoscopic myotomy for esophageal achalasia: Clinical impact of 28 cases. Dig Endosc 2014;26:43-51. DOI: 10.1111/den.12086. [ Links ]
25. Ren Z, Zhong Y, Zhou P, et al. Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 2012;26:3267-72. [ Links ]
26. Khajanchee YS, Kanneganti S, Leatherwood AE, et al. Laparoscopic Heller myotomy with Toupet fundoplication: Outcomes predictors in 121 consecutive patients. Arch Surg 2005;140:827-33. DOI: 10.1001/archsurg.140.9.827. [ Links ]
27. ASGE. The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on peroral endoscopic myotomy. Gastrointest Endoscopy 2015;81(5). DOI: 10.18243/eon/2015.8.9.2. [ Links ]
28. Von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: An international prospective multicenter study. Gastroenterol 2013;145(2):309-11.e1-3. DOI: 10.1053/j.gastro.2013.04.057. [ Links ]
29. Talukdar R, Inoue H, Reddy DN. Efficacy of peroral endoscopic myotomy (POEM) in the treatment of achalasia: A systematic review and meta-analysis. Surg Endosc 2015;29(11):3030-46. DOI: 10.1007/s00464-014-4040-6. [ Links ]
30. Patel K, Abbassi-Ghadi N, Markar S, et al. Peroral endoscopic myotomy for the treatment of esophageal achalasia: Systematic review and pooled analysis. Dis Esophagus 2015;29(7):807-19. DOI: 10.1111/dote.12387. [ Links ]
31. Barbieri LA, Hassan C, Rosati R, et al. Systematic review and meta-analysis: Efficacy and safety of POEM for achalasia. United European Gastroenterol J 2015;3(4):325-34. DOI: 10.1177/2050640615581732. [ Links ]
32. Akintoye E, Kumar N, Obaitan I, et al. Peroral endoscopic myotomy: A meta-analysis. Endoscopy 2016. E-pub ahead of print. DOI: 10.1055/s-0042-114426. [ Links ]
33. Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014;259(6):1098-103. DOI: 10.1097/SLA.0000000000000268. [ Links ]
34. Chan SM, Wu JC, Teoh AY, et al. Comparison of early outcomes and quality of life after laparoscopic Heller's cardiomyotomy to peroral endoscopic myotomy for treatment of achalasia. Dig Endosc 2016;28(1):27-32. DOI: 10.1111/den.12507. [ Links ]
35. Hungness ES, Teitelbaum EN, Santos BF, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg 2013;17(2):228-35. DOI: 10.1007/s11605-012-2030-3. [ Links ]
36. Ujiki MB, Yetasook AK, Zapf M, et al. Peroral endoscopic myotomy: A short-term comparison with the standard laparoscopic approach. Surgery 2013;154(4):893-7(discussion: 897-900). DOI: 10.1016/j.surg.2013.04.042. [ Links ]
37. Marano L, Pallabazzer G, Solito B, et al. Surgery or peroral esophageal myotomy for achalasia: A systematic review and meta-analysis. Medicine (Balt) 2016;95(10):e3001. DOI: 10.1097/MD.0000000000003001. [ Links ]
38. Kumbhari V, Tieu AH, Onimaru M, et al. Peroral endoscopic myotomy (POEM) vs laparoscopic Heller myotomy (LHM) for the treatment of type III achalasia in 75 patients: A multicenter comparative study. Endosc Int Open 2015;3(3):E195-201. E-pub 2015 Apr 13. DOI: 10.1055/s-0034-1391668. [ Links ]
39. Patti MG, Pellegrini CA, Arcerito M, et al. Comparison of medical and minimally invasive surgical therapy for primary esophageal motility disorders. Arch Surg 1995;130:609-15;(discussion 615-6). DOI: 10.1001/archsurg.1995.01430060047009. [ Links ]
40. Roman S, Kahrilas PJ. Distal esophageal spasm. Dysphagia 2012;24:115-23. DOI: 10.1007/s00455-011-9388-3. [ Links ]
41. Salvador R, Costantini M, Zaninotto G, et al. The preoperative manometric pattern predicts the outcome of surgical treatment for esophageal achalasia. J Gastrointest Surg 2010;14:1635-45. DOI: 10.1007/s11605-010-1318-4. [ Links ]
42. Rohof WO, Salvador R, Annese V, et al. Outcomes of treatment for achalasia depend on manometric subtype. Gastroenterol 2013;144:718-25;quiz e713-4. DOI: 10.1053/j.gastro.2012.12.027. [ Links ]
43. Louis H, Covas A, Coppens E, et al. Distal esophageal spasm treated by peroral endoscopic myotomy. Am J Gastroenterol 2012;107:1926-7. DOI: 10.1038/ajg.2012.317. [ Links ]
44. Kandulski A, Fuchs KH, Weigt J, et al. Jackhammer esophagus: High-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM). Dis Esophagus 2015. E-pub 2014 Jan 27. DOI: 10.1111/dote.12182. [ Links ]
45. Kristensen HO, Bjerregaard NC, Rask P, et al. Peroral endoscopic myotomy (POEM) for nutcracker esophagus. Three cases with 12 months follow-up. Scand J Gastroenterol 2014;49:1285-9. [ Links ]
46. Familiari P, Gigante G, Marchese M, et al. Peroral endoscopic myotomy for esophageal achalasia: Outcomes of the first 100 patients with short-term follow-up. Ann Surg 2016;263(1):82-7. DOI: 10.1097/SLA.0000000000000992. [ Links ]
47. Verlaan T, Rohof WO, Bredenoord AJ, et al. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc 2013;78(1):39-44. DOI: 10.1016/j.gie.2013.01.006. [ Links ]
48. Ling TS, Guo HM, Yang T, et al. Effectiveness of peroral endoscopic myotomy in the treatment of achalasia: A pilot trial in Chinese Han population with a minimum of one-year follow-up. J Dig Dis 2014;15(7):352-8. DOI: 10.1111/1751-2980.12153. [ Links ]
49. Teitelbaum EN, Soper NJ, Santos BF, et al. Symptomatic and physiologic outcomes one year after peroral esophageal myotomy (POEM) for treatment of achalasia. Surg Endosc 2014;28(12):3359-65. DOI: 10.1007/s00464-014-3628-1. [ Links ]
50. Pescarus R, Shlomovitz E, Swanstrom LL. Per-oral endoscopic myotomy (POEM) for esophageal achalasia. Curr Gastroenterology Rep 2013;16(369). DOI: 10.1007/s11894-013-0369-6. [ Links ]
51. Rawlings A, Soper NJ, Oelschlager B, et al. Laparoscopic Dor versus Toupet fundoplication following Heller myotomy for achalasia: Results of a multicenter, prospective, randomized-controlled trial. Surg Endoscopy 2012;26(1):18-26. DOI: 10.1007/s00464-011-1822-y. [ Links ]
52. Familiari P, Greco S, Gigante G, et al. Gastro-esophageal reflux disease after per-oral endoscopic myotomy (POEM). Analysis of clinical, procedural and functional factors, associated with GERD and esophagitis. Dig Endosc 2016;28(1):33-41. DOI: 10.1111/den.12511. [ Links ]
53. Jones EL, Meara MP, Schwartz JS, et al. Gastroesophageal reflux symptoms do not correlate with objective pH testing after peroral endoscopic myotomy. Surg Endosc 2015. DOI: 10.1007/s00464-015-4321-8. [ Links ]
54. Grimes KL, Inoue H. Per oral endoscopic myotomy for achalasia: A detailed description of the technique and review of the literature. Thorac Surg Clin 2016;26(2):147-62. E-pub 2016 Feb 10. Review. DOI: 10.1016/j.thorsurg.2015.12.003. [ Links ]
55. Hu JW, Li QL, Zhou PH, et al. Peroral endoscopic myotomy for advanced achalasia with sigmoid-shaped esophagus: Long-term outcomes from a prospective, single-center study. Surg Endosc 2015;29:2841-50. DOI: 10.1007/s00464-014-4013-9. [ Links ]
56. Eleftheriadis N, Protopapas A, Katsogridakis J, et al. Successful peroral endoscopic myotomy for radical treatment of sigmoid-type esophageal achalasia by Greek gastroenterologists. Ann Gastroenterol 2014;27:430-1. [ Links ]
57. Li QL, Zhou PH. Perspective on peroral endoscopic myotomy for achalasia: Zhongshan experience. Gut Liver 2015;9:152-8. DOI: 10.5009/gnl14227. [ Links ]
58. Zhou PH, Li QL, Yao LQ, et al. Peroral endoscopic remyotomy for failed Heller myotomy: A prospective single-center study. Endoscopy 2013;45:161-6. DOI: 10.1055/s-0032-1326203. [ Links ]
59. Onimaru M, Inoue H, Ikeda H, et al. Greater curvature myotomy is a safe and effective modified technique in per-oral endoscopic myotomy (with videos). Gastrointest Endosc 2015;81:1370-7. DOI: 10.1016/j.gie.2014.11.014. [ Links ]
60. Maselli R, Inoue H, Misawa M, et al. Peroral endoscopic myotomy (POEM) in a 3-year-old girl with severe growth retardation, achalasia, and Down syndrome. Endoscopy 2012;44(Suppl 2)UCTN:E285-7. DOI: 10.1055/s-0032-1309924. [ Links ]
61. Familiari P, Marchese M, Gigante G, et al. Peroral endoscopic myotomy for the treatment of achalasia in children. J Pediatr Gastroenterol Nutr 2013;57(6):794-7. DOI: 10.1097/MPG.0b013e3182a803f7. [ Links ]
62. Nabi Z, Ramchandani M, Reddy DN, et al. Per-oral endoscopic myotomy in children with achalasia cardia. J Neurogastroenterol Motil 2016. E-pub ahead of print. DOI: 10.5056/jnm15172. [ Links ]
63. Chen WF, Li QL, Zhou PH, et al. Long-term outcomes of peroral endoscopic myotomy for achalasia in pediatric patients: A prospective, single-center study. Gastrointest Endosc 2015;81(1):91-100. [ Links ]
64. Khashab MA, Stein E, Clarke JO, et al. Gastric peroral endoscopic myotomy for refractory gastroparesis: First human endoscopic pyloromyotomy (with video). Gastrointest Endosc 2013;78(5):764-8. DOI: 10.1016/j.gie.2013.07.019. [ Links ]
65. Chaves DM, De Moura EG, Mestieri LH, et al. Endoscopic pyloromyotomy via a gastric submucosal tunnel dissection for the treatment of gastroparesis after surgical vagal lesion. Gastrointest Endosc 2014;80(1):164. DOI: 10.1016/j.gie.2014.03.045. [ Links ]
66. González JM, Vanbiervliet G, Vitton V, et al. First European human gastric peroral endoscopic myotomy, for treatment of refractory gastroparesis. Endoscopy 2015;47(Suppl 1)UCTN:E135-6. DOI: 10.1055/s-0034-1391821. [ Links ]
67. Mekaroonkamol P, Li LY, Dacha S, et al. Gastric peroral endoscopic pyloromyotomy (G-POEM) as a salvage therapy for refractory gastroparesis: A case series of different subtypes. Neurogastroenterol Motil 2016. DOI: 10.1111/nmo.12854. [ Links ]
68. Shlomovitz E, Pescarus R, Cassera MA, et al. Early human experience with per-oral endoscopic pyloromyotomy (POP). Surg Endosc 2015;29(3):543-51. DOI: 10.1007/s00464-014-3720-6. [ Links ]
![]() Correspondence:
Correspondence:
Pablo Miranda García.
Gastroenterology Department.
Hospital Universitario La Princesa.
Av. Diego de León, 63.
28028 Madrid, Spain
e-mail: pmpablomiranda@gmail.com
Received: 26-11-2016
Accepted: 16-01-2017