My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 n.11 Madrid Nov. 2017
https://dx.doi.org/10.17235/reed.2017.5068/2017
Serrated polyposis syndrome associated with long-standing inflammatory bowel disease
Jesús Castro1, Miriam Cuatrecasas2, Francesc Balaguer1, Elena Ricart1 and María Pellisé1
1Gastroenterology Department. Hospital Clinic Barcelona. Digestive and Hepatic Disease BioMedical Research Network (CIBERehd). Institut d'Investigacions Biomediques August Pi i Sunyer (IDIBAPS). Universidad de Barcelona. Barcelona, Spain.
2Pathology Department. Centre de Diagnostic Biomèdic (CDB). Hospital Clinic, University of Barcelona and Banc de Tumors-Biobank Clinic-IDIBAPS-XBTC. Barcelona, Spain
ABSTRACT
Inflammatory bowel disease (IBD) patients are at an increased risk of developing colorectal cancer (CRC), which is thought to develop via the adenoma-carcinoma pathway. Since the discovery of the serrated carcinogenesis pathway and serrated polyposis syndrome (SPS), the incidence of carcinomas arising from serrated lesions in IBD patients has increased. We report three cases of long-standing IBD patients with associated serrated polyposis syndrome. At present, the pathophysiology of serrated lesions in IBD patients is not fully understood and there is a lack of strong evidence to confirm whether the manifestation of both conditions represents an increased risk of developing cancer. Therefore, more accurate surveillance guidelines are needed and are being actively investigated at present.
Key words: Serrated polyposis syndrome. Ulcerative colitis. Crohn's disease. Inflammatory bowel disease. Colonoscopy. Colorectal cancer. Chromoendoscopy.
Introduction
Inflammatory bowel disease (IBD) patients are at an increased risk of developing colorectal cancer (CRC), thus, endoscopic screening should be performed in all patients with left sided or extensive long-standing colitis (1). In the general population, most cases of CRC develop via the traditional carcinogenesis pathway following the adenoma-carcinoma sequence of events. However, 20-30% of sporadic CRC and most cases of interval CRC arise from the serrated carcinogenesis pathway with serrated polyps as the precursor lesion (2). Serrated polyps are a heterogeneous group including hyperplasic polyps (HP), serrated sessile polyps (SSP) and traditional serrated adenomas (TSA) (2,3).
The serrated polyposis syndrome (SPS) in association with the serrated pathway is a rare entity and has a risk of CRC that is five times greater than that of the general population. The World Health Organization (WHO) criteria for the diagnosis of SPS include: a) the presence of at least five HPs proximal to the sigmoid colon, of which at least two are over 10 mm; b) any number of HPs proximal to the sigmoid colon and a family history of SPS; and c) over 20 HPs of any size, distributed throughout the colon (3). Recently, the association of serrated lesions and SPS with long-standing IBD has been briefly reported. However, our knowledge of the implications regarding this association is still limited. We present a case series report of three patients with long-standing IBD associated with SPS.
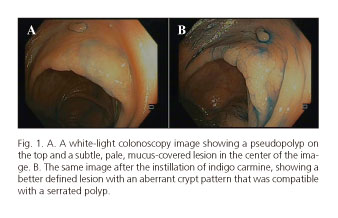
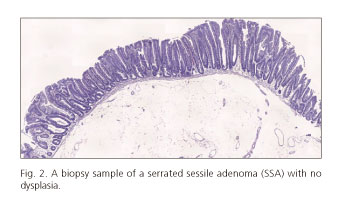
Case Report 1
We present the case of a 49-year-old woman with pancolonic involvement of Crohn's disease with a ten year evolution, in clinical remission and without treatment. White-light colonoscopy screening performed ten years after the initial diagnosis revealed around 30 flat-raised or sessile lesions of approximately 5-20 mm with a serrated appearance. The pathological diagnosis was SSPs. The patient met criteria 1 and 3 for the diagnosis of SPS. A microperforation occurred while performing an en-bloc mucosectomy of a 25 mm sessile polyp located in the transverse colon. This was conservatively managed with hemostatic clips. Pathological examination found that the lesion was an SSP without dysplasia. Immunohistochemical analysis identified a BRAF mutation in codon 600 (V600E/D), and the lesion was negative for a KRAS mutation. As endoscopic management of the serrated lesions was challenging, the patient underwent a subtotal colectomy with rectal preservation. The analysis of the surgical specimen revealed the presence of more than 25 serrated polyps without any evidence of dysplasia.
Case Report 2
The second case was that of a 57-year-old woman with pancolonic ulcerative colitis of 35 years duration, in clinical remission with mesalazine associated with primary sclerosing cholangitis. The patient underwent annual endoscopic screening via white-light endoscopy and no significant lesions were identified. A chromoendoscopy detected 20 to 30 flat-raised lesions of 5 to 20 mm in diameter that displayed changes compatible with hyperplastic polyps. The analysis of the KRAS and BRAF genes showed no mutation. The patient met criteria 1 and 3 for the diagnosis of SPS and continues to undergo annual screening via chromoendoscopy.
Case Report 3
The final case was a 44-year-old woman with left sided ulcerative colitis of two years duration, in clinical remission with mesalazine. The initial white-light colonoscopy revealed over seven lesions with a serrated polyp appearance in the ascending colon. The largest lesion was biopsied and displayed a histopathology compatible with a hyperplasic polyp. After a year without any evidence of active ulcerative colitis, the patient underwent endoscopic surveillance that identified a total of eight lesions compatible with SSSs of 4-15 mm in size (three of them larger than 10 mm) in the ascending colon. All of the lesions were removed and underwent a histopathology study, which confirmed the diagnosis of SSP. The analysis of one of the SSP revealed a BRAF mutation (V600E) and there was no KRAS mutation. This patient met criteria 1 for the diagnosis of SPS and continues to undergo annual screening via chromoendoscopy.
Discussion
This study presents three IBD female patients (two with ulcerative colitis and one with Crohn's disease) with left sided or pancolonic colitis matching the diagnostic criteria for SPS. All patients were in clinical and endoscopic remission. In this series, one of the patients needed surgical management and two were controlled endoscopically. To date, there are two other short case reports of long-standing IBD associated with SPS. Including the series reported here, ten patients have been described; these include six with ulcerative colitis and four with Crohn's disease (seven were female and three were male) (4,5).
The molecular pathogenesis of CRC occurs via two independent pathways: the traditional pathway involving chromosomal instability and the serrated pathway involving DNA microsatellite instability. The most frequent genetic alterations in the serrated pathway include BRAF and/or KRAS mutation, resulting in activation of the MAPK pathway and uncontrolled cell proliferation. BRAF is the most frequent mutation in serrated carcinomas and can be considered as specific of the serrated pathway (2). We found a BRAF mutation in 2/3 serrated lesions whereas no KRAS mutation was found in any sample. Srivastava et al. reported the absence of BRAF mutations in their samples, whereas the KRAS mutation was present in 5/11 samples (5). The pathophysiological mechanism of the serrated pathway in IBD is currently unknown. Chronic inflammation may predispose to the development of serrated lesions and these lesions have a different prognosis than BRAF mutated lesions.
However, in addition to their potential for malignancy, the presence of serrated lesions has been described to be associated with an increased prevalence of synchronous adenomas. Moreover, a recent study reported a prevalence of CRC of 15.8% in SPS patients (6). Boparai et al. reported a frequency of 35% of patients from a SPS cohort that presented with CRC during follow-up, yielding a cumulative CRC risk of 7% over five years (7). Johnson et al. reported an incidence of neoplasia of 30% at three years in IBD patients with serrated changes, compared to 12% in those without serrated changes (8).
Close surveillance with annual colonoscopies and resection of all lesions > 4 mm is recommended in SPS patients (6). Prophylactic surgery is indicated for those cases where endoscopic management is not possible (3). There are currently no specific recommendations for patients with colonic IBD and a concomitant SPS diagnosis. In these patients, a thorough examination and surveillance must be performed. Due to their macroscopic appearance (flat, pale and usually covered with mucus), serrated lesions often go undetected when examined by conventional white-light colonoscopy, meaning that SPS is an under-diagnosed condition. In fact, in the screened population, Rivero-Sánchez et al. observed that the rate of SPS diagnosis increased from 0.32% at baseline white-light colonoscopy to 0.90% after reassessment by chromoendoscopy (9). This fact reinforces the need for the routine use of chromoendoscopy for CRC screening of IBD patients (10).
Conclusions
We describe three cases of IBD in association with SPS which are known to be associated with an increased risk of CRC development. The association of both diseases demonstrates the importance of an adequate endoscopic screening program in patients with IBD via validated techniques, such as chromoendoscopy, which improve the detection rate of lesions. To date, there is no sufficient evidence to determine whether the co-presence of IBD and SPS produces a synergistic effect on CRC development. Furthermore, there are no established guidelines for the treatment and screening of this subgroup. It is clear that this is a population at increased risk of developing CRC and therefore, a more aggressive management and close monitoring of these patients should be performed.
References
1. Annese V, Beaugerie L, Egan L, et al. European evidence-based consensus: Inflammatory bowel disease and malignancies. J Crohn's Colitis 2015;9(11):945-65. DOI: 10.1093/ecco-jcc/jjv141. [ Links ]
2. Yamane L, Scapulatempo-Neto C, Reis RM, et al. Serrated pathway in colorectal carcinogenesis. World J Gastroenterol 2014;20(10):2634-40. DOI: 10.3748/wjg.v20.i10.2634. [ Links ]
3. Orlowska J. Serrated lesions and hyperplastic (serrated) polyposis relationship with colorectal cancer: Classification and surveillance recommendations. Gastrointestinal Endoscopy 2013;77(6):858-71. DOI: 10.1016/j.gie.2013.02.016. [ Links ]
4. Feuerstein JD, Flier SN, Yee EU, et al. A rare case series of concomitant inflammatory bowel disease, sporadic adenomas, and serrated polyposis syndrome. J Crohn's Colitis 2014;8(12):1735-9. DOI: 10.1016/j.crohns.2014.07.001. [ Links ]
5. Srivastava A, Redston M, Farraye FA, et al. Hyperplastic/serrated polyposis in inflammatory bowel disease: A case series of a previously undescribed entity. Am J Surg Pathol 2008;32(2):296-303. DOI: 10.1097/PAS.0b013e318150d51b. [ Links ]
6. Carballal S, Rodríguez-Alcalde D, Moreira L, et al. Colorectal cancer risk factors in patients with serrated polyposis syndrome: A large multicentre study. Gut 2015;gutjnl-2015. [ Links ]
7. Boparai KS, Mathus-Vliegen EM, Koornstra JJ, et al. Increased colorectal cancer risk during follow-up in patients with hyperplastic polyposis syndrome: A multicentre cohort study. Gut 2010;59(8):1094-100. DOI: 10.1016/S0016-5085(09)62067-9. [ Links ]
8. Johnson DH, Khanna S, Smyrk TC, et al. Detection rate and outcome of colonic serrated epithelial changes in patients with ulcerative colitis or Crohn's colitis. Aliment Pharmacol Ther 2014;39(12):1408-17. DOI: 10.1111/apt.12774. [ Links ]
9. Rivero-Sánchez L, López-Cerón M, Carballal S, et al. Reassessment colonoscopy to diagnose serrated polyposis syndrome in a colorectal cancer screening population. Endoscopy 2017;49(01):44-53. [ Links ]
10. Subramanian V, Mannath J, Ragunath K, et al. Meta-analysis: The diagnostic yield of chromoendoscopy for detecting dysplasia in patients with colonic inflammatory bowel disease. Aliment Pharmacol Ther 2011;33(3):304-12. DOI: 10.1111/j.1365-2036.2010.04525.x. [ Links ]
![]() Correspondence:
Correspondence:
María Pellisé.
Department of Gastroenterology and Endoscopy.
Hospital Clinic Barcelona.
Carrer de Villarroel, 170.
08036 Barcelona, Spain
e-mail: mpellise@clinic.cat
Received: 22-05-2017
Accepted: 14-07-2017