My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.2 Madrid Feb. 2018
https://dx.doi.org/10.17235/reed.2018.5373/2017
EDITORIAL
Pursuing excellence in ERCP
1Servicio de Aparato Digestivo. Hospital Virgen de la Luz. Cuenca. España
2Servicio de Aparato Digestivo. Hospital General Universitario. Ciudad Real. España
The term "ERCP cannulation" returns 1,563 items in PubMed. In 1980, there were seven papers, and 92 were included in 2015. Any gastroenterologist knows endoscopic retrograde cholangiopancreatography (ERCP) is often a complex procedure, at times with uncertain results, that unfortunately leads every so often to lawsuits 1. Most issues derive from attempts at biliary cannulation, despite the improved instruments available since the days of the first sphincterotomy back in 1974 2. The initial priority goal of ERCP learning is a satisfactory rate of choledochal cannulation 3. Such rate has been somewhat arbitrarily set as at least 80% of successful biliary access 4.
In nearly 50 years of therapeutic ERCP, much has also been said on the need to engage in regular practice following initial training, in order to maintain acceptable biliary cannulation rates. Institutions performing over 200 ERCPs yearly are considered as high-volume sites, and outcomes seem better in them. However, what really matters is the number of ERCP procedures performed by each specific endoscopist. Ongoing personal commitment, study, and self-criticism improve the practice of such a complex procedure, and eventually provide very acceptable outcomes in low-volume centers 5.
Most ERCPs, whether in big or small institutions, are performed to drain the biliary tree because of obstruction or leaks. Therefore, deep choledochal cannulation is a primary requirement. Overall, one third of ERCPs are easy to carry out, one third are challenging, and the remaining third may be considered as highly difficult procedures. Such estimates are reflected in the paper by De la Morena et al. 6 in the present issue of the Revista Española de Enfermedades Digestivas (The Spanish Journal of Gastroenterology). The author, a highly experienced biliopancreatic endoscopist, successfully obtains "simple" biliary cannulation, i.e., cannulation using a sphincterotome loaded with a guidewire, in 73.4% of cases. This figure may well represent the easy- and challenging-cannulation group. There remains one third of highly complex ERCPs where advanced cannulation techniques are required.
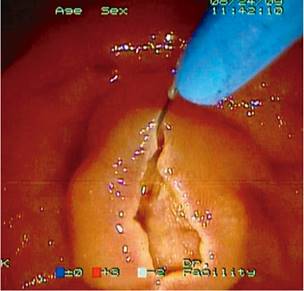
When a guidewire will not enter either the common bile or the pancreatic duct when pushed after sphincterotome insertion in the papillary orifice, the papilla is usually incised using a needle-knife sphincterotome, which in English is called "needle-knife papillotomy" (NKP) and De la Morena 5 describes as needle-knife precut (Fig. 1). Since the first extensive series of patients was reported by Huibregtse in 1986 7, rivers of ink have been spilled on the procedure's benefits and drawbacks. Obviously, it must be used when excellence in biliary cannulation is pursued. On the other hand, however, most endoscopists feel somewhat uneasy when the time comes for NKP during ERCP, as uncertainty is well grounded regarding the outcome.
It was 17 years ago that De la Morena published how he learned his needle-knife papillotomy technique 8. With such a protracted experience, complications in his present study (6) included three perforations and three bleeding events. That is, 6/53 (11.3%) patients, with no pancreatitis events. Perforation of the papillary area occurs retroperitoneally. It may indeed be initially managed in a conservative fashion. However, the word "perforation" renders most physicians shaky. Managing a papillary area perforation conservatively entails uncertainty for several days. Mortality is pretty high in case of intervention should the surgical team be inadequately experienced. Thus, an experienced endoscopist may expect 3/53 (6%) perforations, and a similar bleeding rate, after needle-knife papillotomy. Overall success rate was high for someone with at least 20 years' experience: 51/53 (96.2%).
The other precut type used by De la Morena 6 is the transpancreatic technique. During an attempt at cannulation, a guidewire will often enter the pancreatic duct rather than the biliary tree. This is so because the common bile duct is much more vertical than the pancreatic duct (Fig. 2). Consensus guidelines and protocols remain inconsistent in their defining the times a guidewire should be withdrawn from the pancreas in order to attempt conventional biliary cannulation again, before giving up and turning onto some pancreatic technique. A guidewire successfully located within the pacreatic duct is a real blessing for any endoscopist, as it may provide an initial step to access the common bile duct 9. Therefore, careful thought should be given to whether guidewire withdrawal rather than using the pancreas in the first place to access the biliary tree should be considered. On occasion a guidewire may become stuck within a side branch, and then will not advance to the tail of the pancreas. Notwithstanding this (guidewire in the tail of the pancreas or slightly inserted into the pancreatic duct), pancreatic sphincterotomy may always be used to open up the papillary orifice and expose the common bile duct.

Fig. 2 Several patients who underwent cholecystectomy are shown. Both biliary and pancreatic stents were inserted. The common bile duct takes a more vertical direction than the pancreatic one, making its cannulation more difficult.
Biliary endoscopists have always feared the pancreas from the very start. However, Goff 10) (11, even when initially attempting cannulation without a guidewire, described that when the sphincterotome was found within the pancreatic duct following contrast injection, a pancreatic sphincterotomy could be performed to easily access the common bile duct with no significant increase in complications rate. Transpancreatic precut really represents a pancreatic sphincterotomy directed to 12 o'clock on the papillary mound.
Nowadays, most endoscopists use a guidewire for cannulation, hence an increasing number of pancreatic techniques are now available for biliary cannulation 12. From an academic, formal standpoint, it may be thought that this loss of fear of the pancreas has led endoscopists to refine their choledochal cannulation skills less, and to increasingly use transpapillary precut, the double-guidewire technique, or the insertion of pancreatic stents.
Any endoscopist will find transpancreatic precut easier than needle-knife papillotomy. However, De la Morena et al. 6 find more complications with pancreatic sphincterotomy. It might be argued that the use of NSAIDs for all ERCPs may have decreased pancreatitis rates. Similarly, Ito et al. 13 reported that, provided the guidewire had passed into the pancreatic duct, pancreatic stent insertion significantly decreased post-ERCP pancreatitis rates.
It may also be derived from this study 6 that optimal ERCP practice only rarely requires EUS biliary drainage 14. Whether complications arising from "early" EUS drainage are fewer when compared to precut remains to be seen.
In summary, the paper by De la Morena et al. 6 provides a major illustration of various aspects:
With both commitment and experience an endoscopist may use ERCP to solve almost all cases of common bile duct obstruction or leaks. A total of 98.4% in this study.
Conventional cannulation using a sphincterotome and guidewire is successful in approximately 70% of cases. Even in these non-extremely complex ERCPs, severe pancreatitis may occur in nearly 1% of procedures.
In order to achieve excellence in biliary cannulation, advanced techniques must be used. De la Morena uses two types of precut in almost 30% of cases. Other endoscopists may replace some of these precuts with advanced, precut-free cannulation techniques (double guidewire or pancreatic stents).
In addition to biliary cannulation, other maneuvers to approach biliary drainage, including sphincterotomy and sphincteroplasty, may add complications to the final outcome of ERCP. Some complication should be expected for almost one in every ten procedures. While most are luckily mild, the fact that overall mortality may be around 1% should not be overlooked.
The present study highlights the need for experience and ongoing commitment regarding the involved technique. Hence, to achieve excellence in ERCP the words spoken by Huibregtse in 1996 15, i.e., that "Maybe fewer endoscopists should perform more ERCPs", still remain valid.
BIBLIOGRAFÍA
1. Cotton PB. Have you had an ERCP lawsuit yet? Gastroenterol Nurs 2015;38:101-6. DOI: 10.1097/SGA.0000000000000095 [ Links ]
2. García-Cano J. 200 supervised procedures: The minimum threshold number for competency in performing endoscopic retrograde cholangiopancreatography. Surg Endosc 2007;21:1254-5. [ Links ]
3. García-Cano Lizcano J, González Martín JA. Training in cannulation of the bile ducts using endoscopic retrograde cholangiopancreatography. Gastroenterol Hepatol 2000;23:404-5. [ Links ]
4. Classen M, Demling L. Endoskopische Sphinkterotomie der Papilla Vateri und Steinextraktion aus dem Ductus choledochus. Dtsch Med Wochenschr 1974;99:496-7. DOI: 10.1055/s-0028-1107790 [ Links ]
5. Riesco-López JM, Vázquez-Romero M, Rizo-Pascual JM, et al. Efficacy and safety of ERCP in a low-volume hospital. Rev Esp Enferm Dig 2013;105:68-73. DOI: 10.4321/S1130-01082013000200002 [ Links ]
6. De la Morena Madrigal EJ, Rodríguez García MI, Galera Ródenas AB, et al. Eficacia de canulación biliar y riesgo de pancreatitis de dos técnicas de precorte empleadas de forma precoz. Rev Esp Enferm Dig 2018;110(2):74-81. [ Links ]
7. Huibregtse K, Katon RM, Tytgat GN. Precut papillotomy via fine-needle knife papillotome: A safe and effective technique. Gastrointest Endosc 1986;32:403-5. DOI: 10.1016/S0016-5107(86)71921-4 [ Links ]
8. De la Morena EJ, Domínguez M, Lumbreras M, et al. Self-training in needle-knife sphincterotomy. Gastroenterol Hepatol 2000;23:109-15. [ Links ]
9. García-Cano J. What is the most cost-effective method for a difficult biliary cannulation in ERCP? Rev Esp Enferm Dig 2017;109:171-3. DOI: 10.17235/reed.2017.4863/2017 [ Links ]
10. Goff JS. Common bile duct pre-cut sphincterotomy: Transpancreatic sphincter approach. Gastrointest Endosc 1995;41:502-5. DOI: 10.1016/S0016-5107(05)80011-2 [ Links ]
11. Goff JS. Long-term experience with the transpancreatic sphincter pre-cut approach to biliary sphincterotomy. Gastrointest Endosc 1999;50:642-5. DOI: 10.1016/S0016-5107(99)80012-1 [ Links ]
12. García-Cano J, Taberna-Arana L. A prospective assessment of pancreatic techniques used to achieve common bile duct cannulation in ERCP. Gastrointest Endosc 2012;75:(4S)AB389. DOI: 10.1016/j.gie.2012.03.1030 [ Links ]
13. Ito K, Fujita N, Noda Y, et al. Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation? A prospective randomized controlled trial. J Gastroenterol 2010;45:1183-91. DOI: 10.1007/s00535-010-0268-7 [ Links ]
14. Tonozuka R, Itoi T, Tsuchiya T, et al. EUS-guided biliary drainage is infrequently used even in high-volume centers of interventional EUS. Gastrointest Endosc 2016;84:206-7. DOI: 10.1016/j.gie.2016.03.020 [ Links ]
15. Huibregtese K. Complications of endoscopic sphincterotomy and their prevention. N Engl J Med 1996;335:961-3. DOI: 10.1056/NEJM199609263351309 [ Links ]











 text in
text in