INTRODUCTION
An anterior rectocele is an abnormal protrusion of the rectal wall, typically toward the posterior vagina, which occurs during defecation. The condition frequently occurs in females. Most rectoceles are small and asymptomatic, while some rectoceles, especially large ones, are associated with a difficult evacuation or with chronic constipation 1. However, the etiology and physiology of rectoceles are unclear and it is still not fully understood whether rectocele is a cause or a result of constipation.
Functional constipation is potentially associated with intestinal methane (CH4) according to breath testing and with delayed intestinal transit. Methane produced by enteric bacteria can slow small bowel transit and increase intestinal contractility 2) (3) (4. A positive lactulose breath test (LBT) for methane (CH4) (LMBT+), which indicates the presence of small intestinal bacterial overgrowth (SIBO) that produces CH4, has been recently related to functional constipation with delayed colonic transit 3) (4) (5. We hypothesize that a relationship could exist between breath CH4 levels and rectocele in constipated female patients.
The aims of the study were to compare the profiles of LMBT in constipated patients with rectocele to patients with functional constipation or healthy controls. In addition, the characteristics of clinical symptoms, colonic transit time and anorectal pressure according to LMBT+ in constipated patients with rectocele were evaluated.
MATERIALS AND METHODS
This study was performed by a retrospective review of medical charts. The study was approved by the Institutional Research Ethics Board of the Catholic University of Korea (VC16RISI0158) and adheres to the guidelines of the Declaration of Helsinki.
Study population
A prospective database of consecutive outpatients who visited the teaching hospital of the Catholic University School of Medicine at St. Vincent's Hospital for the evaluation of functional constipation between February 2012 and April 2016 was retrospectively reviewed. Female patients with functional constipation over 18 years of age who underwent the hydrogen (H2) - CH4 LBT, colon marker study, anorectal manometry, and defecography were enrolled into the study. Patients with functional constipation were identified according to the Rome III criteria during the preceding three months, with symptom at onset at least six months before diagnosis 5) (6) (7. At least two of the following symptoms were required for the diagnosis of functional constipation: a) straining during ≥ 25% of defecation; b) lumpy or hard stools in ≥ 25% of defecation; c) sensation of incomplete evacuation in ≥ 25% of defecation; d) sensation of anorectal obstruction/blockage in ≥ 25% of defecation; e) need for manual maneuvers to facilitate defecation in ≥ 25% of cases; and/or f) fewer than three defecations per week. Among constipated patients, subjects with rectocele were included if the size of the rectocele was ≥ 2 cm, as diagnosed by defecography 8.
Patients were excluded if they had a history of diabetes mellitus, connective tissue disease, thyroid disease or gastrointestinal surgery. Other exclusion criteria included the use of anti-secretory agents such as proton pump inhibitors or histamine (H2) receptor antagonists, antibiotics, probiotics, prokinetics, narcotics, laxatives, bulking agents or antidiarrheal drugs. Gastrointestinal disease, renal insufficiency, liver disease, major psychiatric disease, hearing impairment masticatory dysfunction, colonoscopy within the previous three months or incomplete data were also exclusion criteria. The LBT profiles of female patients with constipated rectocele or functional constipation were compared with 30 (historic) healthy female controls. The control subjects were enrolled in order to determine normal LBT values using data from the Catholic University of Medicine from 2007 4.
Lactulose breath tests
Lactulose breath tests were performed with gas chromatography equipment (Quintron BreathTracker SC; Quintron Instrument Company, Milwaukee, WI, USA) following an overnight fast of at least 12 hours. Subjects were asked to follow a strict low residual diet the day before the examination. Thirty minutes prior to the breath test, patients were instructed to wash their mouths with 20 ml of 0.05% chlorhexidine. Physical exercise and cigarette smoking were not permitted for 30 minutes prior to and during the test. After collecting a baseline breath sample, the patients ingested 10 g of lactulose syrup (lactulose concentrate; JW Pharmaceutical, Seoul, Korea). Duplicate samples of end expiratory breath air were collected at baseline and at 15-min intervals for 180 min. The breath H2 and CH4 concentrations were evaluated with the equipment. The definition of an LBT positive status indicating SIBO was defined and classified as follows 9: a) a baseline H2 concentration greater than 20 ppm or an increase in H2 concentration of more than 20 ppm above baseline within 90 min (lactulose H2 breath test (LHBT) + group); or b) a baseline CH4 concentration greater than 10 ppm or an increase in CH4 concentration of more than 10 ppm above baseline within 90 min (LMBT+ group). The LBT (mixed) + group was defined as satisfying both criteria.
Assessment of abdominal symptoms
Demographic data were collected and a bowel symptom questionnaire was routinely performed during LBT in order to diagnose patients with clinically suspected functional constipation. The Korean version of the Irritable Bowel Syndrome Quality of Life questionnaire, which consists of the Rome III criteria together with additional questions about bowel symptoms, was used. This questionnaire has been used and validated in other studies 9) (10) (11. In addition, 13 questions with regard to various bowel symptoms experienced during the preceding four weeks were included. Information about symptoms of abdominal discomfort, pain or cramps, hard or lumpy stools, lose or watery stools, straining during a bowel movement, having to rush to the toilet for a bowel movement (urgency), passing mucus during a bowel movement, abdominal fullness/bloating or swelling, passing gas (flatus), heartburn or chest pain, feeling full soon after starting a meal, passing urine frequently and nausea was collected. The severity of symptoms was evaluated by the total symptom score, which was defined as the sum of the scores for symptom frequency and intrusiveness. The frequency and intrusiveness of each symptom were assessed by each patient using a seven-point scale from 0 (never) to 6 (always or extremely). As the total symptom score was defined as the sum of the scores for symptom frequency and intrusiveness, the range of total symptom scores for each symptom was 0-12.
Anorectal manometry
The patients underwent anal manometry using a water-perfused catheter with eight radially aligned channels attached to a hydraulic capillary infusion system (Medtronic Inc., Minneapolis, MN, USA). The catheter was 4.5 mm in diameter with side holes of 0.8 mm in diameter. The examination was performed in the left lateral position using the rapid pull-through technique. The variables of basal and maximum resting pressure, anal canal length, resting and maximum high pressure zone (HPZ) pressure, HPZ length, basal and maximum squeezing pressure and sensory volume were recorded and analyzed using data collected in the Polygram software (version 4.1; Medtronic Inc.).
The manometry probe was inserted into the rectum and orientated so that the most distal sensor (1 cm level) was located posterior, at 1 cm from the anal verge. After probe placement, there was a rest period of about five minutes in order to give the patient time to relax and the sphincter tone to return to basal levels. Resting pressure was defined as the difference between the intrarectal pressure and the maximum anal sphincter pressure at rest (Fig. 3). After probe placement, the maximum sphincter pressure was measured as an average of a one minute segment at each level, i.e. at 1, 2 and 3 cm from the anal verge. The mean of the three highest values observed at any site in the anal canal was taken as the maximum resting pressure.
The patient was asked to squeeze the anus for as long as possible, for a maximum of 30 seconds, followed by a one minute rest. The maximum squeeze pressure was defined as the difference between the intrarectal pressure and the highest pressure recorded at any level within the anal canal during the squeezing maneuver. By scanning the two squeeze attempts, the mean of the highest pressures recorded at any site in the anal canal was used to calculate the maximum squeeze pressure 12.
Colon maker study
Twenty radio-opaque markers within one capsule (Kolon marker; M.I. Tech, Pyeongtaek, Korea) were used to measure bowel transit time. Subjects swallowed one capsule per day in the morning for three consecutive days. Two plain abdominal radiographs were taken on days 4 and 7 13. The location of markers was classified by bony structures on the abdominal films. The markers located to the right of the vertebral spinous processes and above a line from the fifth vertebrae to the pelvic outlet were included in the right colonic region. The markers on the left of the vertebral spinous processes and above an imaginary line from the fifth lumbar vertebrae to the anterior superior iliac crest were included in the left colonic region. The markers that were lower than a line from the pelvic brim on the right side and the superior iliac crest on the left side were assigned to the rectosigmoid region. Markers were counted in each of the right, left and rectosigmoid regions. The mean segmental and total colonic transit times were calculated as 1.2 xⅹthe sum of markers in the segmental colon on the radiographs on days 4 and 7, according to a formula described previously 14) (15) (16. Subjects were asked to perform their daily routines, to eat normal diets, and to avoid excessive fiber intake and unusually intensive physical activity. Types of constipation were defined as: a) normal transit constipation; and b) delayed transit constipation. The retention of at least 20% of the markers (n = 12) on day 7 was defined as delayed transit constipation 13.
Defecography
Patients fasted from the evening before the procedure and performed a rectal cleaning enema at home a few hours before going to the hospital. At the beginning of the examination, the patient was positioned on the left side and around 300 ml of thick barium paste was injected into the rectum using a plastic syringe connected to a catheter. In female patients, the vagina was opacified with a commercially available barium sulfate paste for oral use. The fluoroscopic table was tilted vertically and a special commode was attached to the footboard with two or three water-filled annular pillows. The patient was then asked to sit on the commode at a right lateral projection. The patient was instructed to empty the rectum completely and without interruption; this process took less than 30 seconds in physiological conditions. An outpouching of the anterior rectal wall that bulged and dislocated the opacified vaginal lumen during straining and evacuation was observed in patients with rectocele 8.
Analysis
Demographic data and the LMBT profiles of patients with constipated rectocele or functional constipation were compared with the demographic data and LMBT profiles of healthy controls. Clinical evaluations included age, body mass index (BMI), intestinal symptoms, parameters of anorectal manometry and colon transit time, type of constipation and breath H2 or CH4 levels according to the presence of rectocele or to a LMBT+ result. Continuous data were expressed as mean ± SD and were analyzed using independent-sample t-tests, whereas the categorical variables were expressed as a quantity (i.e., analyzed using 2 tests or Fisher's exact tests). The Pearson coefficient () was used for the evaluation of the correlation between total breath CH4 concentration and colonic transit time. Multiple stepwise logistic regression analysis was used to identify the independent factors associated with LMBT+. A p value less than 0.05 was considered to be significant for all tests.
RESULTS
Study populations
During the study period, 39 rectocele patients and 44 patients with functional constipation were enrolled in the study. Among the patients with rectocele, six were excluded from the analysis as they were male (n = 4) or due to a lack of data from day 7 of the colon marker study (n = 2). In contrast, among the patients with functional constipation, 18 were excluded as they were male (n = 14) or due to a lack of data from day 7 of the colon marker study (n = 4). Thirty-three rectocele patients and 26 patients with functional constipation were finally analyzed. The age of patients with rectocele or functional constipation was significantly higher than the age of the healthy controls (Table 1). The mean size of rectoceles in cases was 3.52 ± 1.06 cm.
Comparison of lactulose breath test results in patients with rectocele, functional constipation and healthy controls
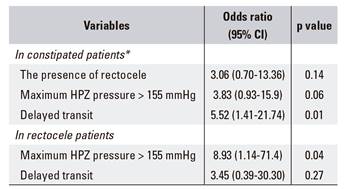
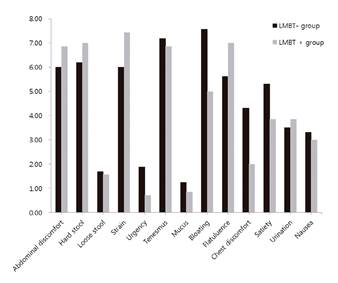
No differences were observed between patients with rectocele and control subjects in the breath H2 concentration at any time points, except at 30 and 45 min (Fig. 1). With regard to breath CH4, there were significant differences or different tendencies between patients with rectocele and control subjects at all of the time points (Fig. 2). Moreover, different tendencies were demonstrated at time point 0, 30, 75, 90, and 105 min between patients with rectocele and functional constipation (Fig. 2). The rate of positivity of the LBT was 48.5% (16/33), 34.6% (9/26) and 26.7% (8/30) in subjects with rectocele, functional constipation and healthy controls, respectively. The LMBT+ and total CH4 concentration were significantly higher in patients with rectocele than in patients with functional constipation or in the healthy controls (Table 1).
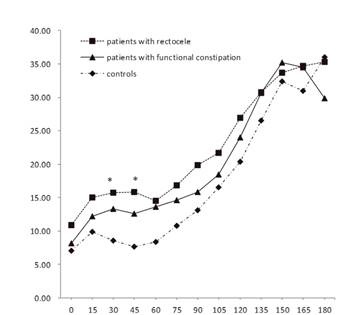
Fig. 1 Lactulose hydrogen (H2) profiles (ppm, parts per million) in constipated patients with rectocele, patients with functional constipation and control subjects (*p < 0.05).
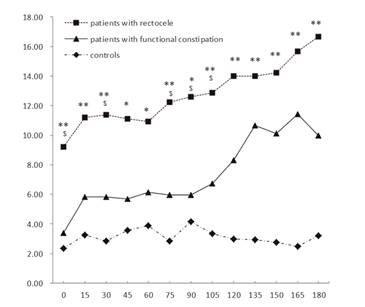
Fig. 2 Lactulose methane (CH4) profiles (ppm, parts per million) in constipated patients with rectocele, patients with functional constipation and control subjects (* or $, p < 0.1; **p < 0.05).
The total CH4 concentration was significantly higher in patients with rectocele than in the healthy controls and the LMBT+ was significantly higher than in patients with functional constipation or healthy controls (Table 1). In contrast, no differences were observed with regard to the rates of positivity of the LBT, LHBT or the total breath H2 concentration among the groups.
Table 1 Demographic clinical data of controls, patients with functional constipation and rectocele
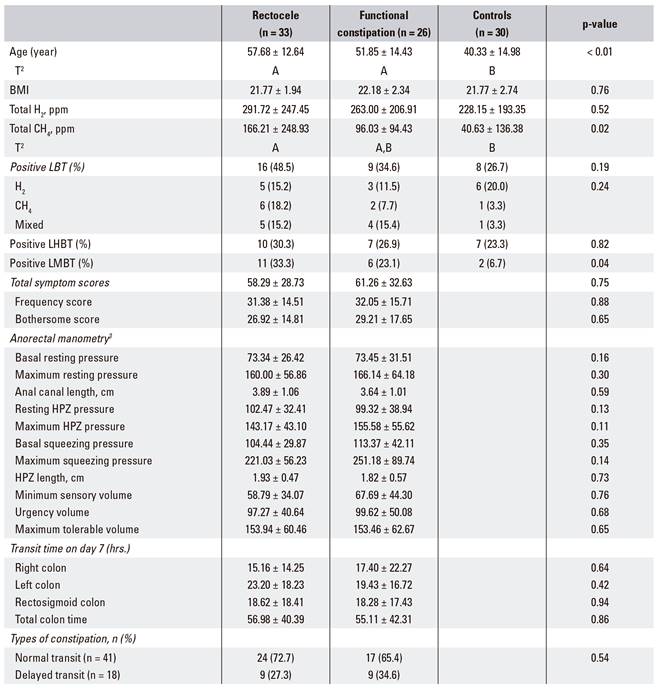
Data are expressed as mean ± SD or number (%). 1Statistical significance was tested by one-way analysis of variances or the chi-square test among groups. 2The same letters indicate non-significant differences between groups based on Tukey's multiple comparison test. 3Pressure (mmHg), length (cm) and volume (ml). BMI: body mass index (kg/m2); H2: hydrogen; CH4: methane; LBT: lactulose breath test; LHBT: lactulose hydrogen breath test; LMBT: lactulose methane breath test; HPZ: high pressure zone.
Characteristics in constipated patients including rectocele and functional constipation
There were no differences between the patients with rectocele and functional constipation with regard to total symptom scores, anorectal manometry parameters, colon transit time and type of constipation (Table 1). With regard to a positive LMBT, no differences were observed in age, BMI, presence of rectocele, total symptom score, anorectal manometry parameters and colon transit time. However, differences were observed with regard to the type of constipation (Table 2). There was a positive correlation between total CH4 concentration and left colonic transit time ( = 0.27, p = 0.04), rectosigmoid colonic transit time ( = 0.30, p = 0.02) and total colonic transit time ( = 0.31, p = 0.02). Delayed transit constipation was the only significant independent factor of LMBT+ according to multivariable logistic regression analysis (Table 3).
Table 2 Characteristics of constipated patients according to a positive LMBT
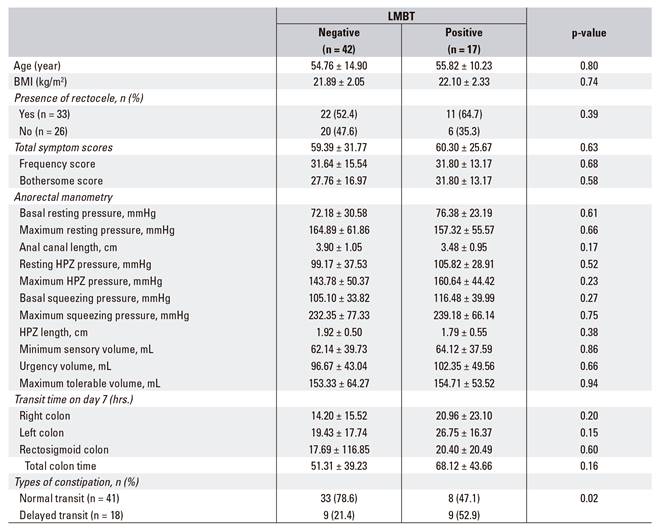
Data are expressed as mean ± SD or number (%). BMI: body mass index (kg/m2); LMBT: lactulose methane breath test; HPZ: high pressure zone.
Characteristics of rectocele patients according to a positive LMBT
There were no differences between patients that were LMBT+ and LMBT negative (LMBT-) with regard to age, size of rectocele, colonic transit time parameters or the type of constipation. With regard to BMI and manometry parameters, basal squeezing pressure (117.03 ± 32.73 vs 98.15 ± 26.93 mmHg, p = 0.09), maximum squeezing pressure (247.45 ± 54.88 vs 207.81 ± 53.24 mmHg, p = 0.06) and maximal HPZ pressure (167.31 ± 39.65 vs 131.10 ± 40.30 mmHg, p = 0.02) tended to be higher or were significantly higher in LMBT+, whereas BMI (20.77 ± 1.59 vs 22.27 ± 1.93, p = 0.03) and HPZ length (1.65 ± 0.43 vs 2.06 ± 0.43 cm, p = 0.02) were lower in LMBT+ patients than in LMBT- patients. However, LMBT+ patients had high individual total symptom scores in comparison to individuals in the LBMT- group with regard to abdominal discomfort, hard stool, straining during defecation and flatulence (Fig. 3). There were no significant differences between frequency scores, intrusiveness scores, total symptom scores or individual symptoms between the two groups. There was a positive correlation between total CH4 concentration and the rectosigmoid colon ( = 0.481, p < 0.01) and total colonic transit time ( = 0.402, p = 0.02). A maximum HPZ pressure of > 155 mmHg was the only significant independent factor of LMBT+ according to multivariable logistic regression analysis (Table 3).
DISCUSSION
This study demonstrated that LMBT+, which indicates the presence of CH4-producing SIBO, was frequent in constipated patients with rectocele. Moreover, breath CH4 is correlated with an increased rectosigmoid colonic transit time and LMBT+ is significantly associated with a high value of maximum HPZ pressure.
The overall rate of LMBT+ in constipated patients with rectocele was 33.3% (11/33), in comparison to 23.1% (6/23) in patients with functional constipation. There is no reported data for rectocele, however, the LMBT+ rate in patients with functional constipation in this study was consistent with the findings of previous studies, and the correlation was 25.8% (16/62) 4. Some researchers believe that jejunal aspirate and culture are the gold standard methods to identify SIBO. Jejunal aspiration has some limitations, including its invasive nature, lack of access to the distal small intestine, the potential for contamination during sampling, low reproducibility and the possibility of missing bacteria due to the patchy distribution of SIBO 2) (17) (18. However, the breath test is a simple alternative and an acceptable method for the diagnosis of SIBO. Currently, the glucose breath test is widely used to evaluate SIBO 19) (20 and this study used the LBT. Lactulose is a non-digestible sugar substrate that passes unabsorbed through the small bowel into the colon. This might be advantageous in the determination of SIBO, which is understood to be associated with an impaired intestinal motility status, which is expected in constipated cases. Glucose is easily absorbed in the proximal small bowel and rarely reaches the distal small bowel or the colon 20) (21. The North American Breath Testing Consensus published in 2017 stated that both the lactulose and glucose breath tests could be used for the diagnosis of SIBO or to evaluate excessive methane excretion in the breath test in association with clinical constipation 22.
Rectocele is commonly reported in adult female patients with an obstructed defecation syndrome 23. Small rectoceles (< 2 cm) are common even in the healthy population, they can be considered as a normal variant secondary to trauma and advanced age and do not require further treatment (17) (24) (25. Therefore, female patients with rectoceles 2 cm or greater in size were enrolled into the study. It is not clear whether rectoceles are a cause or a result of constipation. A recent study suggests that rectoceles are more likely to be a result, rather than the cause of obstructed defecation syndrome 26. This means that surgical procedures intended to correct a rectal wall prolapse are not effective for improving symptoms. In fact, studies of the postsurgical outcome of procedures to correct anatomic abnormalities presumed to be the cause of obstructed defecation syndrome are inconsistent 27) (28) (29) (30. We assumed that rectoceles could be relevant to the functional problem rather than organic disease. Therefore, we analyzed the association between rectocele in association with constipation and LMBT+ in this study.
The rectocele patients were divided into two groups (LMBT+ group and LMBT- group) and the characteristics of both groups were compared. In terms of BMI and manometry parameters, squeezing pressure and maximal HPZ pressure were higher in LMBT+ cases, whereas the levels of BMI and HPZ length were lower in LMBT+ patients in comparison to LMBT- cases. However, multivariate analysis showed that a maximum HPZ pressure of > 155 mmHg was the only independent factor of LMBT+. Although the reason is not clear, it is possible that, anatomically speaking, BMI could be related to the HPZ length, which mutually act as the confounding variables. HPZ pressure itself may be less affected by BMI, which was the only independent factor identified in the multivariate analysis. Although the precise association between LMBT+ and a status of rectocele with constipation is unclear, a previous study reported that breath CH4 was related to functional constipation, particularly in left colonic transit (4). In our study, no significant differences were found in the LHBT profiles among the three groups (i.e., rectocele, functional constipation and control groups). However, the LMBT profiles are the highest at all the time points in the constipated rectocele group and the lowest at all the time points in the control group; the profile of the functional constipation group is in between the two (Fig. 2). A high concentration of breath CH4 might be an important etiological indicator in constipated patients with rectocele. The proposed pathophysiological mechanism is that methanogenic bacteria are predominantly found in the left colon, which could slow intestinal transit 31) (32) (33. In our study, total breath CH4 concentrations in all the constipated patients (including patients with functional constipation or rectocele) were strongly related with an increased left colonic transit time or rectosigmoid colonic transit time, and delayed transit was an independent factor for a positive LMBT. On the other hand, in this study, breath CH4 was significantly associated with increased rectosigmoid colonic transit time and independently related to high HPZ pressure only in constipated patients with rectocele. Intestinal CH4 has been shown to increase the contractile response of the small bowel in animal models 2. We hypothesize that the localization and accumulation of CH4 gas in the anatomical site of the rectocele herniation in the anal canal might interact with and delay rectosigmoid colonic transit and increase rectosigmoid contractile activity. These together cause a vicious cycle.
In this study, the LMBT+ group had high individual bowel symptom scores, including a difficulty with defecation-related symptoms such as abdominal discomfort, hard stool, straining during defecation and flatulence, in comparison to the LMBT- group. However, there were no significant differences in individual symptoms between the LMBT positive and negative groups. Intestinal symptoms such as functional constipation, bloating and diarrhea are potentially ameliorated by treatment with antibiotics targeting intestinal bacteria, possibly represented by a positive breath test 34) (35. These previous studies suggest that antibiotics can improve the symptoms of LMBT+ patients. However, this needs to be verified in further studies.
There are some limitations in this study. First, the study used historical controls. The LBT+ rate in control subjects was similar to that of normal subjects 36 and this approach has been validated in previous studies 4) (9) (10. However, age differences between patients and controls may influence the results of the breath test. Further studies are needed due to the limited information for historic controls. Secondly, there was no information with regard to symptomatic rectocele as well as pelvic outlet dysfunction due to the limitation in the retrospective design of the study. Some patients defined as having functional constipation also show signs of pelvic outlet dysfunction, which could delay colonic transit time. Although the main limitation of the study is the retrospective design, all data were collected consecutively and prospectively with the same standard approach. Demographic data was collected from participants and they completed a validated intestinal symptom questionnaire and were also asked about their history of drug use or surgical procedures prior to the test in order to avoid recall bias. Strict precautions were taken when performing the breath and motility tests, irrespective of the enrollment into the study, in order to obtain an adequate clinical evaluation.
In conclusion, the prevalence of SIBO (which produces the CH4 detected in the LMBT) in constipated patients with rectocele is common. Moreover, increased rectosigmoid colonic transit time or high anorectal pressure might be associated with CH4 breath levels detected by the LBT. Future studies are needed to fully understand the role of intestinal bacteria in patients with rectocele and to demonstrate the potential responses of intestinal bacteria to antibiotic treatment.