My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.7 Madrid Jul. 2018
https://dx.doi.org/10.17235/reed.2018.4719/2016
ORIGINAL PAPERS
Clinical-endoscopic relevance of incidental colorectal lesions detected by PET-CT
1Servicios de Aparato Digestivo. Hospital Universitario Son Espases. Palma de Mallorca, Spain
2Servicios de Medicina Nuclear. Hospital Universitario Son Espases. Palma de Mallorca, Spain
INTRODUCTION
Positron emission tomography (PET) is based on the capture of a radioactive analogue of glucose 18F-2-fluoro-2-deoxyglucose (18F-FDG) by metabolically active cells. The technique is mainly used to determine staging and monitor neoplasms. The combination of this procedure with computed tomography (CT) scanning improves the detection of metabolically active foci 1,2.
The increasing use of PET-CT for the assessment of oncologic patients has led to an increasing number of incidental uptakes detected in the colon 2,3. These unexpected uptakes are often unspecific but could be indicative of inflammatory, premalignant or malignant lesions 4. Low intensity uptake frequently tends to be diffuse or lineal, which corresponds to the physiological activity within the large intestine. However, with more focal images of a higher intensity, it is more difficult to differentiate between a malignant transformation and a normal variant, as there is a high rate of false negatives and positives 1,4,5.
The use of PET-CT for the differentiation of malignant and benign pulmonary nodules is well established. However, its ability to distinguish between malignant and benign pathology is less apparent with regard to colon assessment 1. Based on this, the current recommendation is that colonoscopy procedures should be performed in all cases of incidental uptakes in the large intestine by PET-CT 6,7. Nevertheless, due to the fact that not all findings are related to pathological conditions and that unnecessary investigations could lead to a delay in the onset of treatment of primary illness, the choice of an appropriate evaluation diagnostic tool is often challenging. Therefore, a predictive risk factor for malignancy such as the maximum standardized uptake value (SUVmax), which defines the intensity of uptake, could be useful to determine the urgency of colonoscopy procedures 8.
This study aimed to investigate the proportion of incidental PET-CT uptake in the colon, evaluate their correlation with endoscopy and histology and determine the value of SUVmax that discriminates between benign and malignant lesions.
MATERIALS AND METHODS
This was a retrospective study to identify colonic uptake in 3,000 patients who underwent PET-CT between December 2011 and February 2015. Endoscopic and histological reports were reviewed whenever relevant and PET-CT findings were correlated with endoscopic and histological findings. Patients with a prior history of colorectal cancer were not excluded from the analysis. It is important to note that patients who had not undergone subsequent endoscopies or cases with incomplete or poorly prepared procedures were excluded. Patients with a history of inflammatory bowel disease or actively undergoing treatment with metformin at the time of PET-CT were also excluded. This is due to the fact that metformin leads to an intense increase of diffuse images of 18F-FDG in the colon and, to a lesser extent, in the small intestine. This limits the capacity of PET-CT diagnosis and possibly masks the detection of a neoplasm 9. Incidental uptake was defined as the focal accumulation of 18F-FDG in patients that underwent a pathological study that was not related to the colon or in areas incompatible with the previously known pathology. The intensity of uptake was measured according to the value of SUVmax. All patients signed a written informed consent for all diagnostic and therapeutic procedures.
Imaging technique
Images were taken with a GE ST70 tomograph, in strict accordance with the standard operating protocol. A body scan was performed from lower orbit to third proximal of the femur after intravenous administration of 6-10 mCi of 18F-FDG. When areas of interest in the intestine with an unclear origin or elevated intensity were identified, a new "delayed" image was obtained at 90-180 minutes of 3 min/bed. When the original PET image identified a focal uptake which corresponded to the CT image, a repeat "delayed" procedure was deemed unnecessary.
Correlation with colonoscopy
Data related to subsequent colonoscopies was collected from the clinical history of all patients with identified regions of interest from the PET-CT study. Pathological reports were correlated with incidental uptake during PET-CT. Histological reports of a biopsy or polypectomy were obtained and the final diagnosis was reached according to the endoscopic findings and the histology of the lesion. Each region captured with 18F-FDG with a subsequent negative colonoscopy was considered as physiological absorption.
Pathology
Histological analysis of a lesion obtained after colonoscopy was considered to be malignant when the following were identified: carcinomas, invasive adenomas, metastatic disease, primary malignancies and myeloproliferative processes infiltrating colonic mucosa. Hyperplastic polyps and adenomatous polyps (tubulous, villous and tubulovillous) were considered as non-malignant.
Statistical analysis
The statistical analysis was performed using the G-Stat version 2.0 and Epidat version 4.1 software. A descriptive analysis was performed to describe the characteristics of incidental uptake. Consistency was measured using the kappa (k) coefficient with an established confidence interval (CI) of 95%. The t-test was used for the evaluation of SUVmax to detect a relevant pathology or neoformation. The Mann-Whitney U test was used for the evaluation of SUVmax to detect advanced dysplasia and large polyps. The Pearson's product-moment correlation (r) was used in the study of SUVmax and polyp size (mm). The Chi-squared test, 2 x 2 and HxK were used to evaluate the presence of a relevant pathology by gender, position, symptoms and type of primary tumor. CI was estimated at 95% and statistical significance was set at p < 0.05.
RESULTS
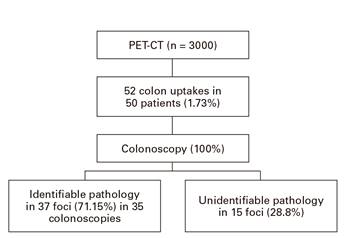
Of the 3,000 patients who underwent a PET-CT scan, 69% were male and 31% were female with a mean age of 65.77 years (± 11.2). Fifty-two uptakes (1.73%) were identified in the colon of 50 patients (Fig. 1).
The location of uptakes were the rectum in ten cases (19.23%), sigmoid colon in 18 cases (34.62%), descending colon in seven cases (13.46%), transverse colon in one case (1.9%), ascending colon in ten cases (19.23%), cecum in five cases (9.62%) and the ileocolic anastomosis in one case (1.92%) (Table 1).
A subsequent colonoscopy was performed in all cases with uptake, and a relevant pathology was found in 71.15% of cases (37 pathological findings, two during same colonoscopy); there were no mucosal alterations found by colonoscopy in 15 (28.8%) cases. The endoscopic lesions correspond to five neoplasms (13.5%) (four adenocarcinomas and one lymphoma), 30 polyps (81.1%) (13 tubulovillous adenomas, 12 tubulous adenomas, one villous adenoma, one hyperplastic polyp, one inflammatory polyp, two polyps with unknown pathological anatomy) and two inflammatory mucosal lesions (5.4%) (Table 2). The mean polyp size was 27 mm. There were no statistically significant differences between the SUVmax value with regard to the size (≥ 1 cm o < 1 cm) of polyps (p = 0.12) or the SUVmax value regarding the presence or absence of advanced dysplasia (p = 0.33).
Table 2 SUVmax correlation with PET-CT uptake and histology



ADC: adenocarcinoma; TA: tubulous adenoma; TVA: tubulovillous adenoma; VA: villous adenoma; IP: inflammatory polyp; IML: inflammatory mucosal lesion; HP: hyperplastic polyp; UHO: unknown histological origin; NC: normal colonoscopy. *Three incidental uptakes described during PET-CT, without specifying the SUVmax value.
The concordance between PET-CT and endoscopy location was high, with a κappa value of 0.90 (95% CI 0.83-0.93). The SUVmax value of all areas of incidental uptake varied between 2.8 and 21.1 g/ml, with a global average of 8.16 g/ml (typical deviation [TP] = 3.73). The SUVmax average of adenomatous polyps was 9.26 g/ml (TP = 4.53), neoplasia 11.7 g/ml (TP = 4.05), inflammatory lesions 10.5 g/ml (TP = 0.21) and 6.05 g/ml (TP = 1.78) in cases of colonoscopies without pathological findings (Fig. 2). Significant differences were observed in the SUVmax value in neoplasms (p = 0.03) and adenomatous polyps (p = 0.04) compared to inflammatory lesions.
Primary neoplasms with the largest number of incidental uptake by PET-CT in the colon during the study were lung, non-Hodgkin lymphoma and breast (Table 3). A multivariate analysis using logistic regression did not identify predictive factors of endoscopy findings such as age, sex, uptake location, PET-CT indication and type of primary tumor, and the p vales were 0.76, 0.51, 0.27, 0.19 and 0.19, respectively.
DISCUSSION
Fluorodeoxyglucose positron emission tomography (18F-FDG PET) is widely used in imaging tests of various malignancies for staging and surveillance. The integration of CT and PET images has increased the ability to locate regional areas of interest. However, the experience with PET-CT is limited and a consensus recommendation in terms of clinical application is still under assessment. Therefore, the use of colonoscopy and a histological study of colonic uptakes are the standard for subsequent evaluations 10,11.
In this study, the proportion of incidental uptake in the colon by PET-CT was 1.73%, which is similar to previously published studies 1,6,8,10. Colonoscopy revealed the presence of a relevant pathology in 37 (71.15%) of the 52 colonic uptake foci identified by PET-CT; the most common locations were in the rectum and sigmoid colon (51.9%). Of these 37 lesions, 13.51% were a neoplasm and 81.08% were polyps. These findings are also similar to those of previous studies 6,8,12,13,14. Nevertheless, our study demonstrated that despite a careful examination of the colonoscopy image, no lesions were found in 15 cases of 18F-FDG uptake. This represents a false-positive rate of 28.8% by PET-CT. These false-positive images could be due to intestinal inflammation, physiological uptake or imaging of gastrointestinal lymphoid tissue 15. Van Hoeij et al. 8 noted an absence of colonic lesions after colonoscopy in 38% of patients with focal uptakes in the colon by PET-CT. Peng et al. 16 noted and verified normal colonoscopies in 56% of patients evaluated with incidental colonic uptakes. Whereas studies conducted by Putora et al. 3 and Farquaharson et al. 17 reported a rate of 13.7 and 16.7% of normal colonoscopies in patients with incidental uptakes by PET-CT, respectively.
With regard to the standard uptake value, a significantly higher mean value of SUVmax was found for malignant lesions compared to other types of lesions (p = 0.03). A mean SUVmax value of 11.7 g/ml (10.5-19.5) for incidental uptake corresponded to neoplasms, with a lower mean value for polyps and inflammatory lesions (9.26 g/dl and 10.5 g/dl, respectively). Furthermore, there were differences between the SUVmax values of incidental uptake related to the endoscopic detection of polyps, with a mean value of 9.26 g/ml versus 69 g/ml in those of a normal endoscopy. In previous studies, the mean SUVmax of neoplasms fluctuated between 5.7 and 17.3 g/ml 3,13,18,19. In the study conducted by Luboldt et al. 19, the mean SUVmax of neoplasms and advanced adenoma were significantly higher than those corresponding to false positives, although other studies found no significant differences in the mean SUVmax amongst the different groups assessed 3,6,13,18.
In our study, a multivariate analysis found no differences between sex, age, PET-CT indication, location of PET-CT uptake, or type of primary tumor in reference to the defined diagnostic categories. This is in accordance with previous studies by Treglia G et al. 6. However, Peng et al. 16 described variations between age and location of PET-CT uptake with regard to the presence of a neoplasm, polyp or normal colonoscopy, with relevant pathological findings predominating in cases ≥ 60 years old and lesions in the distal colon and rectum.
Our data identified significant differences between SUVmax values in cases of endoscopically confirmed lesions, especially neoplasms. This suggests that SUVmax values ≥ 11 g/dl may indicate a higher risk of malignancy and should be evaluated by colonoscopy as a priority. Van Hoeij et al. 8 established a cut-off point for SUVmax of ≥ 11.4 to distinguish between malignant and non-malignant lesions, which is very similar to our results. However, we cannot conclude that the SUVmax value is capable of differentiating between advanced adenomas without submucosal invasion and benign lesions. Therefore, all incidental uptake by PET-CT in the colon should be studied by colonoscopy, regardless of the SUVmax value. This statement also falls in line with previously published studies 3,6,8,13,14,16,17,18.
In our study, patients with a history of previously treated colorectal cancer were not excluded and there were a total of six cases. Four of them were investigated in order to re-stage a rectal neoplasm and images were obtained of the rectum that confirmed the presence of a neoplasm in a subsequent colonoscopy in two cases. In the third case, the image corresponded to an inflammatory lesion, and the colonoscopy was normal in the fourth case. The two cases with a history of colon cancer underwent a colonoscopy due to an increase in tumor markers; no relevant pathology was identified.
A limitation of our study is that it was not possible to calculate the sensitivity or specificity of PET-CT for the detection of colon lesions due to the fact that only colonoscopies were performed in patients with a positive PET-CT. Therefore, we were unable to determine the false negative rate. This issue will be addressed in future studies.
In conclusion, the results of our study suggest that malignant lesions in the colon have higher SUVmax values by PET-CT than other types of lesions. This could help to distinguish between a malignant and non-malignant pathology, with a cut-off point of ≥ 11 g/dl, which assists in the prioritization of endoscopic evaluation. However, the SUVmax is not able to differentiate between a benign pathology of advanced adenomas. Therefore, any PET-CT with colonic uptake should be further studied endoscopically. Thus, the SUVmax could help to define the urgency of a colonoscopy but not whether it should be performed or not.
BIBLIOGRAFÍA
1. Weston BR, Iyer RB, Qiao W, et al. Ability of integrated positron emission and computed tomography to detect significant colonic pathology: the experience of a tertiary cancer center. Cancer 2010;116:1454-61. PMID: 20143447. DOI: 10.1002/cncr.24885 [ Links ]
2. Lin M, Koo JH, Abi-Hanna D. Management of patients following detection of unsuspected colon lesions by PET imaging. Clin Gastroenterol Hepatol 2011;9:1025-32. PMID 21723237 DOI: 10.1016/j.cgh.2011.06.028 [ Links ]
3. Putora RM, Müller J, Borovicka J, et al. Relevance of incidental colorectal FDG-PET-CT-enhanced lesions. Onkologie 2013;36:200-4. PMID: 23548969. DOI: 10.1159/000350302 [ Links ]
4. Cook GJ, Fogelman I, Maisey MN. Normal physiological and benign pathological variants of 18-fluoro-2-deoxyglucose positron emission tomography scanning: potential for error in interpretation. Semin Nucl Med 1996;26:308-14. PMID: 8916319. DOI: 10.1016/S0001-2998(96)80006-7 [ Links ]
5. Prabhakar HB, Sahani DV, Fischman AJ, et al. Bowel hot spots at PET-CT. Radiographics 2007;27(1):145-59. PMID: 17235004. DOI: 10.1148/rg.271065080 [ Links ]
6. Treglia G, Calcagni ML, Rufini V, et al. Clinical significance of incidental focal colorectal F-fluorodeoxyglucose uptake: our experience and a review of the literature. Colorectal Dis 2011;14:174-80. PMID: 21689289. DOI: 10.1111/j.1463-1318.2011.02588.x [ Links ]
7. Beatty JS, Williams HT, Aldrige BA, et al. Incidental PET/CT findings in the cancer patient: how should they be managed? Surgery 2009;146:274-81. PMID: 19628085. DOI: 10.1016/j.surg.2009.04.024 [ Links ]
8. Van-Hoeij FB, Keijsers RG, Loffeld BC, et al. Incidental colonic focal FDG uptake on PET/CT: can the maximum standardized uptake value (SUVmax) guide us in the timing of colonoscopy? Eur J Nucl Med Mol Imaging 2015;42(1):66-71. PMID: 25139518. DOI: 10.1007/s00259-014-2887-3 [ Links ]
9. Steenkamp DW, McDonnell ME, Meibom S. Metformin may be associated with false-negative cancer detection in the gastrointestinal tract on PET/CT. Endocr Pract 2014;20(10):1079-83. PMID: 25100379. DOI: 10.4158/EP14127.RA [ Links ]
10. Fletcher JW, Djulbegovic B, Soares HP, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med 2008;49:480-508. PMID: 18287273. DOI: 10.2967/jnumed.107.047787 [ Links ]
11. Fuertes J, Montagut C, Bullich S, et al. Incidental focal uptake in colorectal location on oncologic 18FDG PET and PET/CT studies: histopathological findings and clinical significances. Rev Esp Med Nucl Imagen Mol 2015;34(2):95-101. PMID: 25263718. DOI: 10.1016/j.remn.2014.07.008 [ Links ]
12. Jamar F, Buscombe J, Chiti A, et al. EANM/SNMMI guideline for 18F-FDG use in inflammation and infections. J Nucl Med 2013;54(4):647-58. PMID: 23359660. DOI: 10.2967/jnumed.112.112524 [ Links ]
13. Gutman F, Alberini JL, Wartski M, et al. Incidental colonic focal lesions detected by FDG PET-TC. AJR Amb J Roentgenol 2005;185:495-500. PMID: 16037527 DOI: 10.2214/ajr.185.2.01850495 [ Links ]
14. Tatlidil R, Jadvar H, Bading JR, et al. Incidental colonic fluorodeoxyglucose uptake: correlation with colonoscopic and histopathologic findings. Radiology 2002;224:783-7. PMID: 12202714. DOI: 10.1148/radiol.2243011214 [ Links ]
15. Drenth JP, Nagengast FM, Oyen WJ. Evaluation of (pre-)malignant colonic abnormalities: endoscopic validation of FDG-PET findings. Eur J Nucl Med 2001;28:1766-9. PMID: 11734913 DOI: 10.1007/s002590100645 [ Links ]
16. Peng J, He Y, Xu J, et al. Detection of incidental colorectal tumours with 18F-labelled 2-fluoro-2-deoxyglucose positron emission tomography/computed tomography scans: results of a prospective study. Colorectal Dis 2011;13:e374-8. PMID: 21831098. DOI: 10.1111/j.1463-1318.2011. 02727.x [ Links ]
17. Farquaharson AL, Chopra A, Ford A, et al. Incidental focal colonic lesions found on (18)Fluorodeoxyglucose positron emission tomography/computed tomography scan: further support for a national guideline on definitive management. Colorectal Dis 2012;14:e56-63. PMID: 21831171. DOI: 10.1111/j.1463-1318.2011.02760.x [ Links ]
18. Kei PL, Vikram R, Yeung HW, et al. Incidental finding of focal FDG uptake in the bowel during PET-CT: CT features and correlation with histopathologic results. AJR Am J Roentgenol 2010;194(5):W401-6. PMID: 20410385. DOI: 10.2214/AJR.09.3703 [ Links ]
19. Luboldt W, Volker T, Wiedemann B, et al. Detection of relevant colonic neoplasms with PET/CT: promising accuracy with minimal CT dose and a standardized PET cut-off. Eur Radiol 2010;20(9):2274-85. PMID: 20503051. DOI: 10.1007/s00330-010-1772-0 [ Links ]
Received: November 16, 2017; Accepted: January 13, 2018











 text in
text in