My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.110 n.8 Madrid Aug. 2018
https://dx.doi.org/10.17235/reed.2018.5557/2018
CASE REPORTS
Tumor recurrence after liver transplantation for diffuse biliary papillomatosis in the absence of invasive carcinoma
1Departamento de Cirugía Hepatobiliar y Trasplante de Órganos Abdominales. Hospital Universitario 12 de Octubre. Madrid, Spain
2Departamento de Anatomía Patológica. Hospital Universitario 12 de Octubre. Madrid, Spain
INTRODUCTION
Intraductal papillary neoplasm of the bile duct (IPNB), also known as biliary papillomatosis (BP), is a rare entity characterized by the presence of multiple papillary tumors in the intrahepatic and/or extrahepatic biliary tree. Chappet 1 first described this condition in 1894 and less than 100 cases have been described in the literature since then. The disease mainly affects middle-aged adults and the male:female ratio is 2:1. It is considered as idiopathic, although there are cases associated with biliary stones, Caroli disease, Clonorchis infestation and hepatitis B and C virus infection 2. It is a premalignant entity with a high risk of malignant transformation 3. The risk of recurrence is high, even after radical surgery. When the disease extends widely from the intrahepatic to the extrahepatic biliary tree, liver transplantation (LT) is the only available option.
CASE REPORT
We present the case of a 43-year-old male with no relevant history who was admitted to our hospital with abdominal pain, fever and jaundice. Physical examination revealed right hypochondrium pain and the laboratory tests showed high levels of all liver enzymes, hyperbilirubinemia, leucocytosis and high levels of inflammatory parameters. An abdominal ultrasonography (US) revealed a wide dilatation of the intra- and extrahepatic biliary tree. Computed tomography (CT) and magnetic resonance (MR) (Fig. 1) confirmed the presence of a wide dilatation of the biliary duct and also identified a mass over the ampulla. An endoscopic retrograde cholangiopancreatography (ERCP) was subsequently performed and an adenomatous tumor over the ampulla was found. The initial histological study of the ampulla mass identified an intestinal adenocarcinoma. A cephalic pancreaticoduodenectomy was performed. The definitive histological study identified an IPNB with multiple foci of severe dysplasia that affected the margins of the biliary and pancreatic resections. The ampullary mass was a papillary tumor with severe dysplasia-in situ carcinoma. No stromal, vascular or perineural infiltration was observed and 12 negative lymph nodes were isolated.
The case was discussed in a multidisciplinary committee who decided to perform a total pancreatectomy prior to considering the patient as a candidate for a LT. The histological study identified papillomas within the entire remnant of the pancreatic duct with different grades of dysplasia, without infiltrative carcinoma. Finally, LT with a whole graft was performed 12 months after the onset of the disease. The definitive histological study showed a diffuse IPNB that involved the entire biliary tree with multiple foci of severe dysplasia, without the presence of infiltrative carcinoma and three negative lymph nodes (Fig. 2). A CT was performed every six months during follow-up and a CT scan at 24 months identified a large hepatic mass of 11 x 10 x 15 cm in the right hepatic lobe and multiple small nodules throughout the liver. A percutaneous biopsy was performed and the histological study confirmed the presence of a biliary adenocarcinoma. The patient worsened progressively and died six weeks after the diagnosis of disease recurrence.

Fig. 2 Pathological images. A. IPNB that affects the light of the extra-hepatic bile duct, with papillary projections and cylindrical epithelium and high-grade dysplasia in situ carcinoma (H-E 100x). B. IPNB that affects all intra-hepatic biliary ducts with high grade dysplasia, without stromal infiltration. (H-E 40x). Intraductal papillary neoplasm (red arrows). Liver parenchyma (blue arrow).
DISCUSSION
IPMB or BP is a rare disease which can involve any area of the biliary epithelium to a greater or lesser extension. It may even affect the main pancreatic duct. Diagnosis and establishment of extension are very difficult to accomplish preoperatively. Location and extension are very variable, affecting the intra- and extrahepatic biliary tree in 58% of cases, the intrahepatic biliary tree exclusively in 22%, the extrahepatic biliary tree exclusively in 14%, and the extrahepatic biliary tree and the main pancreatic duct in 3% of cases 4. It is considered as a premalignant condition with a high risk of malignant transformation. Surgical treatment must be aggressive in order to achieve resection of all affected areas. A LT may be necessary in cases in which the intrahepatic biliary tree is widely involved. With regard to cases in which the pancreatic duct is affected, its extent will determine the type of the pancreatectomy.
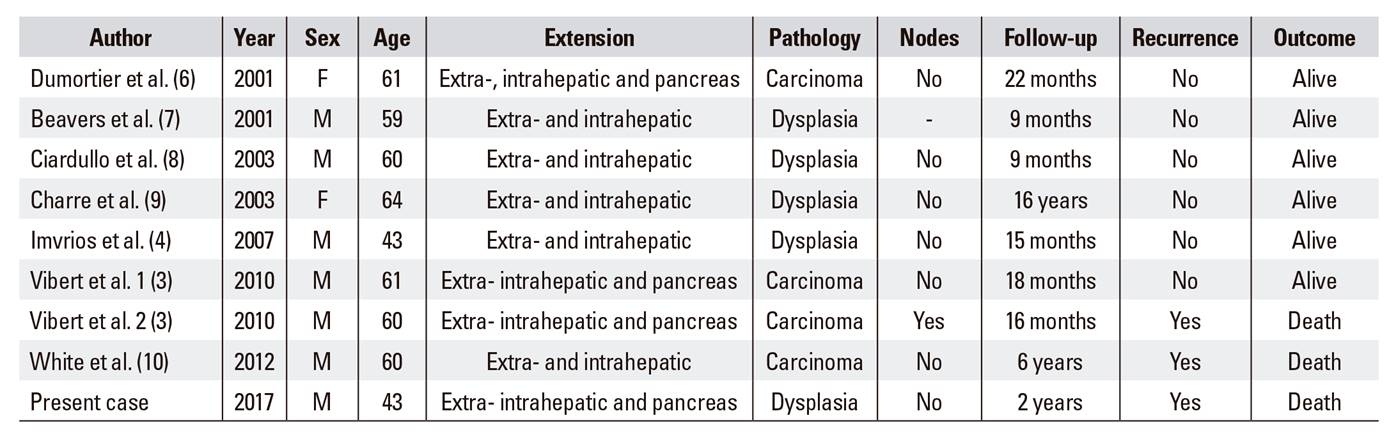
Since 2000, only eight cases of diffuse BP treated with LT have been described in the literature 3,5,6,7,8,9,10 (Table 1). All had both intra- and extrahepatic biliary tract involvement and the main pancreatic duct was also affected in three cases, as in the present case. In 2010, Vibert et al. 3 published a series of three cases with different clinical situations. They concluded that in the absence of invasive carcinoma and positive lymph nodes, LT can be performed successfully, even in cases in which there are foci of superficial infiltration. Provided that there is no lymphatic involvement, transplantation can still be an effective alternative in these patients. Of the eight cases, only four histological studies showed invasive carcinoma in the explant liver after transplantation; one had lymph node involvement. Two had a recurrence at 16 months and at six years respectively and the remaining two were alive without recurrence at 18 and 22 months, respectively. The present case is the first that describes recurrence of the disease after LT in the absence of invasive carcinoma and positive lymph nodes. There was a follow-up longer than two years in only one of the four described cases with an absence of infiltrating carcinoma and positive lymph nodes 10.
Our patient had a recurrence two years after transplantation and it would also be interesting to know how the rest of the patients have evolved since the study was published. It is important to appreciate that the diffuse nature of the disease makes it very difficult to perform a complete histological study of the entire biliary tissue of the specimen. Therefore, in the case of advanced lesions such as severe dysplasia or in situ carcinoma, the presence of small microinvasion foci may not be detected. However, if we analyze the conclusions obtained by Vibert et al. 3, superficial infiltration foci in the absence of lymphatic involvement should not compromise the results of the LT. On the other hand, although we know that it is a recurrent disease, its pathogenesis is unknown. Furthermore, the patterns of possible papillomatosis recurrence over the new liver in the absence of a previous invasive carcinoma are unknown. This problem should also be considered as a possible explanation of the evolution in the present case. What seems clear is that the prognosis in cases of a recurrence is poor, regardless of the presence of invasive carcinoma foci in the surgical specimen, as all published cases with recurrence after LT died in a short period of time. Probably, immunosuppression makes the recurrence of the disease more aggressive with a worse prognosis.
CONCLUSION
In conclusion, LT is the only curative treatment available for patients with diffuse BP. However, these patients are at risk of disease recurrence, so it is important to optimize the immunosuppressive treatment and perform a close follow-up by imaging studies in order to detect a recurrence as soon as possible.
BIBLIOGRAFÍA
1. Chapet V. Cancer epitelial primitif du canal clodedoque. Lyon Medical 1894;76:145. [ Links ]
2. Mourra N, Hannoun L, Rousvoal G, et al. Malignant intrahepatic biliary papillomatosis associated with viral C cirrosis. Arch Pathol Lab Med 2001;126:369. [ Links ]
3. Vibert E, Dokmak S, Belguiti J. Surgical strategy of biliary papillomatosis in Western countries. J Hepatobiliary Pancreat Sci 2010;17:241. DOI: 10.1007/s00534-009-0151-1 [ Links ]
4. Imvrios G, Papanikolau V, Lalountas M, et al. Papillomatosis of intra- and extrahepatic biliary tree: successful treatment with liver transplantation. Liver Transpl 2007;13:1045. DOI: 10.1002/lt.21207 [ Links ]
5. Lee SS, Kim MH, Lee SK, et al. Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer 2004;100:783. DOI: 10.1002/cncr.20031 [ Links ]
6. Dumortier J, Scoazec JY, Valette PJ, et al. Successful liver transplantation for diffuse biliary papillomatosis. J Hepatol 2001;35:542. DOI: 10.1016/S0168-8278(01)00126-X [ Links ]
7. Beavers KL, Fried MW, Johnson MW, et al. Orthotopic liver transplantation for biliary papillomatosis. Liver Transpl 2001;7:264. DOI: 10.1053/jlts.2001.22322 [ Links ]
8. Ciardullo MA, Pekolj J, Acuna Barrios JE, et al. Multifocal biliary papillomatosis: an indication for liver transplantation. Ann Chir 2003;128:188. DOI: 10.1016/S0003-3944(03)00038-5 [ Links ]
9. Charre L, Boillot O, Goffette P, et al. Long term survival after isolated liver transplantation for intrahepatic biliary papillomatosis. Transpl Int 2006;19:249. DOI: 10.1111/j.1432-2277.2005.00253.x [ Links ]
10. White AD, Young AL, Verbeke C, et al. Biliary papillomatosis in three Caucasian patients in a Western centre. EJSO 2012;38:181. DOI: 10.1016/j.ejso.2011.11.007 [ Links ]
Received: March 08, 2018; Accepted: April 26, 2018











 text in
text in