Dear Editor,
Benign extrahepatic biliary neoplasms are infrequent lesions with an incidence < 0.1% and account for 6% of all tumors of the extrahepatic bile duct 1. Approximately 75% are adenomas 2 and the most common location is the main hepatic duct 3. They are usually small (1-3 cm) but rarely diffuse. Obstructive jaundice is the most frequent symptom in about ninety percent of cases.
Case report
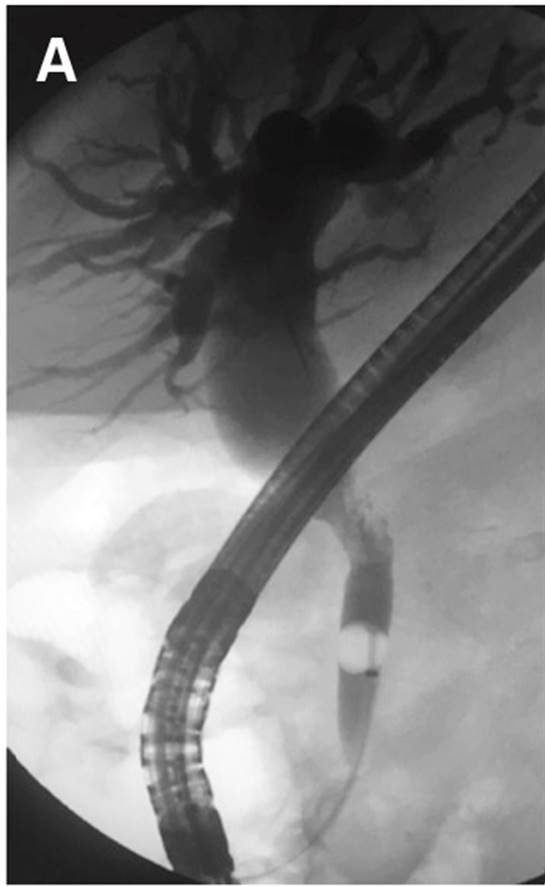
We present a case with obstructive jaundice and a dilatation up to the middle third of the common bile duct with a solid hyperechogenic material that was observed via abdominal ultrasound. An irregular and long stenosis of 2 cm in the proximal bile duct was observed via endoscopic retrograde cholangiopancreatography (ERCP) (Fig. 1A) and a biopsy was taken. A 22 x 14 mm polylobulated lesion was identified via computed tomography (CT) (Fig. 1B) in the common bile duct. Surgery was indicated due to the histological diagnosis of a villous adenoma. A resection of the common bile duct and hepaticojejunostomy was performed. The histological description of the surgical specimen was an intestinal type adenoma with papillary morphology and low grade dysplasia.
Discussion
Adenomas of the extrahepatic bile duct are a rare entity. They usually present with obstructive jaundice and the definitive diagnosis can only be made histologically. Imaging tests are essential, mainly ERCP. Its etiology is related to inflammatory processes and, in some cases, to cystic dilation of the bile duct.
They are polypoid lesions with a papillary, tubular or mixed architecture, lined by epithelium with different degrees of dysplasia 4. The lining is usually intestinal and they are similar to intestinal tubulo-villi.
These benign neoplasms have a risk of malignant transformation, thus surgical resection is mandatory. Local endoscopic resection is not indicated due to the high incidence of recurrence 3.
Although they manifest as several degrees, from mild dysplasia to carcinoma in situ, they are not considered as precursors of malignant tumors. This is due to the fact that adenomas are less frequent than carcinomas and there are no pre-existing adenoms in the majority of carcinomas, but rather flat dysplasia and carcinoma in situ 5.