My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Cirugía Oral y Maxilofacial
On-line version ISSN 2173-9161Print version ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 n.3 Madrid May./Jun. 2007
ARTÍCULO CLÍNICO
Results of the multidisciplinary management of unilateral cleft lip and palate patients
Resultados del manejo multidisciplinario del labio y paladar fisurado unilateral*
M. Estrada Sarmiento1, R. Espinosa Fonseca2, E. Pérez Perdomo3
1 Consultante Profesor Auxiliar. Especialista II grado Cirugía Máxilo Facial. Jefe de Cátedra
Cirugía Máxilo Facial de la facultad de ciencias medicas Celia Sánchez
Manduley. Profesor principal de cirugía Buco-Máxilo Facial. Investigador
agegado.
2 Instructor. Especialista I grado en ortodoncia.
3 Licenciada logopedia.
Hospital Provincial Universitario, "Carlos Manuel de Cespedes", Bayamo.
Granma, Cuba.
*Trabajo Presentado en la XVI Jornada Científica del Hospital Carlos Manuel de Céspedes.
ABSTRACT
A model was designed to evaluate the protocol and strategy of the interdisciplinary team treating unilateral cleft lip and palate patients at the Maxillofacial Surgery department of the "University Provincial Hospital Carlos Manuel de Cespedes" Bayamo, Granma, Cuba. A maxillofacial surgeon, an orthodontist and a phoniatrician evaluated the current state of 60 patients with ages ranging between 14 and 22. The results showed that more than half of the patients had finished their treatment by one of the specialists. Only 27 patients (16.2%) had completed their treatment by the three specialists. The factors contributing to these percentages are discussed.
Key words: Protocol; Interdisciplinary team; Unilateral cleft lip and palate.
RESUMEN
Se diseñó un modelo para evaluar el protocolo y la estrategia del equipo multidisciplinario para el tratamiento del labio y paladar fisurado unilateral en el Servicio de Cirugía Máxilo Facial del Hospital Provincial Universitario "Carlos Manuel de Céspedes" de Bayamo. Cuba.
El estado presente de 60 pacientes de 14-22 años de edad fue evaluado por un cirujano máxilo facial, un ortodoncista y un foníatra. Los resultados indicaron que más de la mitad de esos pacientes tenían completado el tratamiento por uno de los especialistas. Solo 27 pacientes (16,2%) habían completado el tratamiento por los tres especialistas. Los factores que contribuyeron a este porcentaje fueron discutidos.
Palabras clave: Protocolo; Equipo multidisciplinario; Labio y paladar fisurado unilateral.
Introduction
A multidisciplinary team can improve the treatment for cleft lip and palate patients and a wide selection of associated problems.1,2 The team will have perfected their knowledge of the disciplines and a role will have been defined for each professional in the complex rehabilitation process of patients with cleft lips and palates. Not all multidisciplinary teams for cleft patients function in the same manner with regard to Human Resources or Management3 We designed this study as a model for evaluating strategic protocols and conducts for multidisciplinary treatment of cleft lip and palate patients in our activity.
Material and method
The object of the evaluation was to describe the current state of 60 patients (39 males and 21 females) with unilateral cleft lips and palates. The patients were selected randomly from the population treated between 1992-2004 by the multidisciplinary team of the department of Maxillofacial Surgery of the "Hospital Provincial Universitario Carlos Manuel de Céspedes" in Bayamo, Cuba. A maxillofacial surgeon, an orthodontist and a phoniatrician evaluated each patient.
The information in the medical histories was used to describe the original defect and the therapeutic behavior of the patients. The previously mentioned specialists were selected because they had been involved in the treatment of all the patients with this condition.
When the study was carried out, the age of the patients varied between 14 and 23. We chose the age of 14 because it was the lower limit for evaluating results in the long term, and because we expected the treatment to be completed at this age.
All the patients had complete unilateral clefts of the lip and palate, 13 on the right and 47 on the left. We chose complete clefts in order to have a homogenous group, although the multidisciplinary team knew the individual variations of the congenital malformations, cleft width, position of the maxillary segments, surgical techniques and the skill of the surgeon. The primary repair of the lip was carried out on average at between 3-12 months.
Evaluation by the Maxillofacial Surgeon
The Maxillofacial Surgeon (MES), who used a code with established norms for obtaining the subsequent results, evaluated all the patients. The results were evaluated by judging the existing deformities on examination. The number and severity of the deformities were used for classifying the result as good, regular or bad.
• Good: No additional treatment required.
• Regular: Optional additional treatment.
• Bad: Additional treatment indicated.
Orthodontic evaluation
The orthodontist described the current state of the 60 patients regarding facial growth and occlusion using photographs, study models and cephalometric studies. Of the 60 patients, 40 had completed their orthodontic treatment, 17 patients still required treatment. The clinical examination indicated that 3 of the 60 patients had an anterior crossbite. They had not finished the treatment. The cephalometric data of the patients who had finished their treatment was compared with the cephalometric norms according to Steiners facial growth studies, as quoted by Mayoral. 4 The cephalometric measurement SNA0, SNB0 and ANB0 were used for comparison.
Phonetic evaluation
The phoniatrician carried out various evaluations of the 60 patients in relation to speech, some based on objective and others on subjective measurements5 such as:
• Stimulation test of Ps and Ss to determine if the patient could produce these sounds correctly.
• Physical examination of the oral cavity, with reference to occlusion.
• Orthodontic apparatus and oronasal and nasolabial fistulas.
Based on these finding, three clinical criteria were established for determining the possible causes of some of the speech disturbance.
• Velopharyngeal competence
• Dental risk
• Functional language factors
The reliability of these criteria has been reported in the literature.1,6
Results
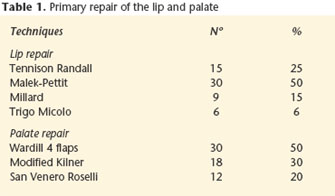
Table 1 shows the type of surgical technique used for the primary repair of a cleft lip. Of the 60 patients, 18 (30%) received secondary procedures for correcting residual defects. A total of 59 surgical interventions were carried out, with an average of 9.8 per patient. The more common secondary operations were scar revision (25%) and vermilion correction (28.3%). Vermilion correction was carried out on two occasions in 2 patients. Nasolabial fistulas were closed in 15% of the patients. In 9 of the 60 patients and in one patient the operation was carried out twice. Palate repair was carried out (Table 1) at 18- 30 months. Oronasal fistulas were closed in the anterior portion of the hard palate in one patient and 2 in the soft palate. A secondary intervention was carried out in one out of 60 patients because of velopharyngeal insufficiency, using a lower base flap. Nasal deformities were corrected in 16 of the 60 patients. A total of 53 secondary operations were carried out with a proportion of 8.8 per patient. The more common techniques included: Nasal tip rhinoplasty (32%), correction of deformed wing (20%) and reconstruction of the nasal floor (13.2%). Good functional and aesthetic results of the lip and nose were found in 29 (48.3%) of the 60 patients. For this group the surgical treatment was judged by the multidisciplinary team to be complete. Thirty-one patients appeared to require further surgery.
Table 2 shows the type and frequency of secondary deformities of the lip, nose and palate. The most common secondary deformity of the lip was associated with the vermilion notch and nasolabial fistulas. Sixteen patients (26.7) had nasolabial fistulas, which was due to the nasal floor not closing initially in the 9 patients (15%) who were operated using Millards technique, did not initially undergo closure of the nasal floor, and in 7 patients (11.7%) the fistulas were produced because of maxillary expansion during orthodontic treatment.
With the exception of 9 patients operated using Millards technique, the closure of the fistula was carried out in 85% of the sufferers, using the Tennison- Randall and Maleck Pettit techniques in which a nasal floor is made, which generally avoids this sequelae. The most common functional disturbance of the lip was associated with the inadequate reconstruction of the orbicular muscle of the lips. A final analysis of the lip surgery results considered 65% as good, 25% as regular and 10% as bad. The functional results of the lip were comparable. The most common secondary nasal deformity was asymmetry of the nasal tip (28%) and flat wing 11.7%. A depression in the nasal floor was also noted in 5 patients (8.3%).
The aesthetic results in the nose were catalogued as good in 61.6% of the cases, regular in 21.7% and bad in 10%. The functional results found were: good in 68.3%, regular in 25% and bad in 6.7%.
The palate repair analysis revealed that oronasal fistulas in the lower part of the hard palate were found in 1.7% of patients. In one patient the palate was short.
Palate movement was judged subjectively as adequate.
Overall results
Table 3 shows the number and percentage of patients who had completed their treatment in one, two or in the three specialties. In the 14-22 age group, just over half of the 60 patients had finished their treatment by one specialty, and only 21 patients (35%) had completed their treatment by the three specialties.
Discussion
The present study indicates that even when the treatment provided by the multidisciplinary team in our institution for cleft lips and palates was successful in many aspects, there were still conditions to be treated in the patients studied.
The aesthetic evaluation revealed residual deformities in the lip and nose that required additional surgical treatment. Strict criteria were used to evaluate the aesthetic results, although slight deformities were still found. More than half the group displayed some sort of nasal deformity. Secondary deformities of the lip were also found in more than half the patients, results that were similar to those reported by Henkel.7 The percentage of nasolabial fistulas found in our series was moderate, but lower that those reported by Bardach1 in his investigation.
The complete success of the primary palate repair compared with velopharyngeal competence was high (98.3%) in our investigation. Our results are similar to those achieved by Estrada Sarmiento,8 but better than those reported by some authors9 who suggested that a success rate should fluctuate reasonably between 60% and 70%.
Only one of the 60 patients showed an abnormal functional language pattern that required therapy to eliminate. Nearly a quarter of the patients continue to have minor speech errors. However, some of these patients appeared interested in acquiring treatment. An interesting finding is the absence in this group of glottal articulation.
Facial growth and occlusion were good in the patients that had completed orthodontic treatment. The percentage of residual defects found in our investigation are peculiar to this condition, and they are in accordance with those expected in the group studied, and those that appear in the medical literature10,11 for this type of malformation, regardless of the surgical technique used.9, 12-15
Many patients who had been brought in by their parents late could have had better aesthetic results with the surgery, which for the reasons given was delayed.
The main finding in our study was that in the 14-23 age group, only 35% (21 out of 60 patients) completed their treatment in the three specialties. Various factors may explain why the results of the multidisciplinary team were not as favorable as expected.
• The team for a time did not have an orthodontic service.
• Another factor that contributed to the low percentage of completely treated cases was that some parents did not want to submit their children to additional surgical interventions.
• A group of parents failed to attend the hospital after the cheilorrhaphy, and these children failed to carry out the remaining treatment phases.
• The strong criteria used by the investigating team for fully judging the treatment also contributed to the low number of cases.
The result of this study reveal the great need for the multidisciplinary team to continue with their perfections in order to obtain better results at an early age.
![]() Correspondence:
Correspondence:
Dr. Manuel Estrada Sarmiento
Máximo Gómez 6 / Maceo y Canducha Figueredo. Bayamo
85100 Granma, Cuba
Email: mesarmiento.grm@infomed.sld.cu
Recibido: 30.10.06
Aceptado: 28.05.07
References
1. Bardach J. Late results of multidisciplinary management of unilateral. Cleft Lip Palate Ann Plast Surg 1984;12:235-42. [ Links ]
2. Morris HL. Velopharyngeal competence and primary cleft palate Surgery. A critical review. Cleft Palate 1973;10:62. [ Links ]
3. Warren MM. The organization of the cleft palate team. Plast Reconst Surg 2001;21:201-6. [ Links ]
4. Mayoral J. Ortodoncia. Principios Fundamentales y Prácticos. Edición Revolucionaria 1986:241-57. [ Links ]
5. Lindsay WK. A study of the speech results of a large series of cleft palate patients. Plast Reconst Surg 1962;29:273. [ Links ]
6. Henkel KO. Incidence of secondary lip surgeries. Cleft Palate Craniofac J 2002; 21:204-9. [ Links ]
7. Bardach J. Speech development following primary veloplasty. J Speech Hear Res 2001;73:200-16. [ Links ]
8. Estrada Sarmiento M. Análisis del tratamiento quirúrgico de 53 Pacientes con fisuras palatinas. Rev Cubana Pediatría 1997;69:192-6. [ Links ]
9. Monserat Soto ER. Paladar hendido. Presentación de un caso. Acta Odontológica Venezolana 2002;40:180-5. [ Links ]
10. Hemprich A. Secondary operations in lip-jaw-palate clefts. Mund Kiefer Gesichtschir 2000;4:S61-7. [ Links ]
11. Louw B, Shibambu M, Roemer K. Cleft palate team: Cleft Palate. Craniofacial J 2006;43:47-54. [ Links ]
12. Millard. Extensions of the rotation-Advancement principle for wide unilateral. Cleft Lip Plast Reconst Surg 1968;42:535-44. [ Links ]
13. Trigo Micolo I. Queilonasoplastia primaria mediante la técnica del colgajo Triangular modificada. Cirugía Plástica. Ibero latinoamericana I 1980;297-305. [ Links ]
14. Vergara Piedra L. Evaluación de la técnica de Malek-Petit. Rev Cubana Estomatol 1981;24:283-89. [ Links ]
15. Estrada Sarmiento M. Evaluación de la técnica de Trigo Micolo Multimed: 2004;8:40-8. [ Links ]











 text in
text in