My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Cirugía Oral y Maxilofacial
On-line version ISSN 2173-9161Print version ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 n.6 Madrid Nov./Dec. 2007
CASO CLÍNICO
Injerto libre braquial medial
P. Martos Díaz1, F.J. Rodríguez Campo2, R. González García1, V. Escorial2, S. Guillermo2, F.J. Díaz González3
1 Médico Residente.
2 Medico Adjunto.
3 Jefe de Servicio. Servicio de Cirugía Oral y Maxilofacial Hospital Universitario de la Princesa. Madrid, España.
ABSTRACT
Introduction. Free medial microvascularized arm grafts have not become very popular for the reconstruction of head and neck defects due to anatomic variations in their vascularization. Our objective was to describe the anatomy and surgical technique and to review the literature on the advantages and disadvantages of free medial arm grafts.
Material and methods. We report the case of a patient with squamous cell carcinoma of the left jugal mucosa with same-side lymph node involvement. The tumor was resected with margins and a functional cervical dissection was performed. The defect was reconstructed using a free medial microvascularized graft from the left arm.
Discussion. We believe that free medial arm grafts are a safer option for the reconstruction of cervicofacial defects and that they offer advantages, among which can be highlighted: not sacrificing a terminal artery, primary closure of the donor zone, minimal esthetic defect, and yielding fine, elastic, hairless skin.
Key words: Medial arm flap; Superior ulnar collateral artery.
RESUMEN
Introducción. Entre las reconstrucciones de defectos titulares de cabeza y cuello, el injerto libre microvascularizado braquial medial no ha adquirido mucha popularidad debido a las variaciones anatómicas que se reflejan en la vascularización de éste. Nuestro objetivo es realizar una descripción de la anatomía y técnica quirúrgica, así como una revisión de la literatura describiendo las ventajas y desventajas de este tipo de injerto.
Material y método. Presentamos el caso de una paciente con carcinoma epidermoide de mucosa yugal izquierda con afectación ganglionar ipsilateral. Se procedió a su resección con márgenes más disección cervical funcional. La reconstrucción del defecto se llevó a cabo mediante un injerto libre microvascularizado braquial medial de brazo izquierdo.
Discusión. Pensamos que el injerto libre braquial medial de brazo se trata de una opción más segura a la hora de la reconstrucción de defectos cervicofaciales, aportando una serie de ventajas entre las que destacan: no sacrificio de una arteria terminal, cierre primario de la zona donante, mínimo defecto estético, y poseer una piel fina, elástica y sin vello.
Palabras clave: Colgajo branquial medial; Arteria colateral superior cubital.
Introduction
Many reconstructive techniques are now used to cover softtissue defects of the head and neck, particularly within the context of oncological resections or the repair of traumatic wounds with major tissue loss.
Among the free microvascularized grafts, the graft most widely used now in maxillofacial surgery is the free lower arm graft. This graft has become popular due to a series of advantages, including consistent anatomy, safety, design flexibility, and the feasibility of working simultaneously in two fields with two different teams.1
The choice of reconstructive method is influenced by the characteristics of the graft (skin characteristics, thickness, pedicle length, etc.) and receptor areas (intraoral, extraoral or mixed defect, presence or absence of osseous involvement, etc).
The medial arm graft is one of the options for repairing tissue defects in the cervicofacial region. Its advantages include: little hair, relatively fine and elastic skin, good donor zone healing, a location that is not very visible, permitting direct closure and a pedicle that does not contain a terminal artery. In this article, we briefly describe the anatomy and surgical technique for preparing a medial arm flap. We report a new clinical case and review the literature.
Anatomic description
The blood supply to the skin of the medial part of the arm comes from branches of the brachial artery, a branch of the axillary artery. The brachial artery emits the deep brachial artery in the upper arm and the superficial collateral ulnar artery (SCUA) in the lower arm. Much less frequently, the SCUA branches from the deep brachial artery. The brachial artery can also emit direct cutaneous and musculocutaneous branches that contribute variably to the blood supply of the medial arm. In any case, a main branch of greater caliber than the others is always found and it is generally the SCUA, with a frequency of 80 to 100% depending on the author.2-5
In the surface anatomy, the SCUA originates approximately 4-6 cm distal to the insertion of the pectoral muscle on the humerus. It passes through the medial part of the arm to a point to 3-4 cm above the epitrochlea. The artery is accompanied in this trajectory by its two concomitant veins and it cutaneous branches that vascularize the skin. Overall pedicle length is 5- 8 cm and pedicle diameter is 1.3-1.6 mm.4,5
Surgical technique
The patient is placed in supine position with the arm supinated and abducted 90º. The elbow may be flexed 90º (Fig. 1).
The axis of the flap is a straight line drawn from the medial axilla to the epitrochlea. The lower edge of the skin flap is located 3-4 cm from the epitrochlea and the upper edge depends on the length needed, although it is always below the axilla. The anterior edge depends on the surface area required to cover the defect and is located about 3 or 4 cm from the axis. Total flap width should not exceed 8 cm for direct closure.5
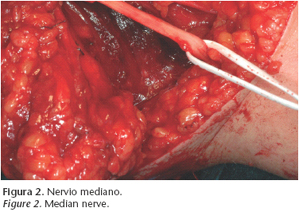
An incision is made in the skin on the anterior edge of the flap and the subcutaneous tissue is dissected. Before reaching the fascia of the brachial biceps, the basilic vein is located and dissected. Dissection continues and the median nerve is located deeper and anterior to the vein (Fig. 3). Prior to the location of the main trunk of the median nerve, cutaneous nerve branches will be visible, which may be preserved if they do not complicate dissection.
When the median nerve is located, the posterior incision is made, beginning from the lowest point. The flap is lifted subfascially until the ulnar nerve is located. This is not difficult because of its caliber.
A meticulous dissection is performed along the ulnar nerve and the graft pedicle, formed by the artery and the superficial collateral ulnar veins, is located. If the diameter of the vein is too small, the basilica vein can be used as the venous component of the flap. In most cases this is the first option.
Septocutaneous arterial branches of sufficient caliber may be found throughout the dissection. These branches must be conserved and reserved as a possible pedicle component if the caliber of the SCUA is smaller. Once the graft is lifted, the skin, which is sufficiently elastic, is closed directly.
Clinical case
The 58-year-old patient had a history of venous thrombosis of the lower limbs and no other findings of interest. The patient presented an ulcerated lesion of the left jugal mucosa that measured approximately 3 cm in diameter and was consistent with squamous cell carcinoma (Fig. 2). A lymph node 2 cm in diameter was palpated at cervical level I.
We performed surgery and resected the tumor with a safety margin and unilateral functional cervical dissection. The defect was reconstructed with a medial graft of the left arm. The flap pedicle used contained the SCUA, which was anastomosed to the facial artery. The thyro-linguo-facial venous trunk (TLFVT) was anastomosed to one of the concomitant veins of the SCUA because there was no retrograde blood flow through the basilic vein (Fig. 4).
Pedicle length was about 6 cm, artery diameter, 1.5 mm, and venous diameter, 1 mm The intraoral defect was covered completely with sufficient volume
(Fig. 5). The skin of the arm was closed directly (Fig.6) without need for a free graft.
The patient was released 10 days after the intervention and the viability of the graft was correct.
Discussion
Daniel et al.6 first studied the medial arm flap in 1975. They described the flap vascularization based on the dissection of 16 cadavers. The indicated that the vascularization is based on perforating cutaneous branches emitted by the SCUA. There have not been many publications since then on medial arm flaps. It is observed that there is a certain reluctance to use this flap, due mainly to the many variations found in the anatomy of the medial arm.
Dolman et al.2 in 1979 reported the absence of SCUA in 20% of 20 dissections of cadavers performed, noting the impossibility of preparing a medial arm flap if this artery is absent.
In 1981, Matloub et al.7 demonstrated five different types of blood supply to the middle arm region by dissecting 36 cadavers.
In 1987, Breidenbach et al.3 observed, in the dissection of 20 cadavers, that the blood supply to the medial region of the arm is conducted in 65% by cutaneous branches of the SCUA, in 20% by the brachial artery , and in 15% of cases, by both.
In the patient reported, we did not contemplate the existence of direct cutaneous branches because the predominant vessel was the SCUA, which emitted small branches to the subcutaneous tissue and skin.
In 1992, Matloub et al.4 concluded, based on the dissection of 40 cadavers, that the perfusion of the medial arm derives from a combination of vessels that originate along the course of the brachial artery. Among these vessels, one always has a caliber of more than 1 mm and is dominant. In 95% of cases, this vessel is the SCUA.
Karamursel et al.5 in 2005 studied the dissection of 5 cadavers and 12 clinical cases, concluding that a flap can be prepared using direct cutaneous branches of the superficial brachial artery or SCUA, which are almost always present, thus ensuring the pedicle of the flap.
In relation to venous return, authors5,6 usually agree to use the basilic vein if the veins that accompany the SCUA are not large enough for the flap, because this vein also is suitable. Our intention was to use the basilic vein in the case described, but it was found to lack venous return when the artery was anastomosed. For that reason, the concomitant vein of the SCUA was used despite the difference in caliber with the TLFVT.
The flap can also be prepared by including the cutaneous sensory branches of the medial brachial cutaneous nerve, thus endowing the skin with a certain sensitivity, although it is more time-consuming and prolongs the duration of the intervention. This is why the nerve is usually sectioned during dissection. 6
Thanks to the elasticity of the skin in this location, a flap approximately 8 cm wide can be obtained without interposing a graft and the wound can be closed directly. The graft will also have a considerable subcutaneous tissue volume (depending on each persons fatty layer), which is a point to be considered in reconstructions that require more tissue volume for replacement. If more width is needed, a free graft will have to be prepared to cover the defect, which is not advisable because it leaves the ulnar nerve relatively unprotected. In this case, it is necessary to use another type of microvascularized graft.
This type of graft in no case involves sacrificing a terminal artery, so if any problem of pedicle viability is observed in the course of surgery, we have the option of changing to a forearm flap in the same surgical act. The flap of the medial arm can then be used as free skin coverage for replacement with a lower arm flap. The arm is closed directly and the cosmetic defect is small because it is an area with good healing and a discrete location.
Conclusions
We consider the free medial arm graft to be an option for the reconstruction of defects in the head and neck region. It is an alternative to lower arm grafts if a larger volume defect has to be treated, and it has other advantages like the possibility of performing direct closure, a smaller esthetic defect, and not having to sacrifice a terminal artery.
![]() Correspondence:
Correspondence:
Pedro Luis Martos Díaz.
Hospital de la Princesa.
Departamento de Cirugía Maxilofacial.
C/ Diego de León N° 62, 28006, Madrid, España.
Email: plmartos@mixmail.com
Received: 17.10.05
Accepted: 23.03.07
References
1. Urken ML, Cheney ML, Sullivan MJ, Biller HF. Atlas of Regional and Free Flaps for Head and Neck Reconstruction. Raven Pres Ltd, New York 1995;p.p.149-68. [ Links ]
2. Dolmans S, Guinberteau JC, Baudet J. The upper arm flap. J Microsurg 1979;1:162- 3. [ Links ]
3. Breidenbach WC, Adamson W, Terzis JK. Medial arm flap revisited. Ann Plast Surg 1987;18:156-63. [ Links ]
4. Matloub HS, Ye Z, Yousif NJ, Sanger JR. The medial arm flap. Ann Plast Surg 1992;29:517-22. [ Links ]
5. Karamürsel S, Bagdath D, Demir Z, Tüccar E, Celebioglu S. Use of medial arm skin as a free flap. J Oral Maxillofac Surg 2005;115:2025-31. [ Links ]
6. Daniel RK, Terzis J, Schwarz G. Neurovascular free flaps: a preliminary report. Plast Reconstr Surg 1975;56:13-20. [ Links ]
7. Matloub HS, Trevisani TT, Eder E, Godina M. The medial arm neurosensory free flap. Presented at the Annual Meeting of the American Society for Plastic and Reconstructive Surgery, New York, NY, October 20,1981. [ Links ]











 text in
text in