My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Revista Española de Cirugía Oral y Maxilofacial
On-line version ISSN 2173-9161Print version ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 n.4 Madrid Jul./Aug. 2009
Mandibular ossifying fibroma: case report and literature review
Fibroma osificante de mandíbula: presentación de un caso y revisión de la literatura
A. Lombardi1, M. Cerullo2, J.C. Garzón2, J. Martínez3, E. Cuella4
1 Jefe de división. Especialista en Cirugía y Traumatología Buco-Máxilo-Facial
2 Especialista en Cirugía y Traumatología Buco-Máxilo-Facial
3 Jefe de residentes
4 Residente
Servicio de Cirugía y Traumatología Buco-Máxilo-Facial.
Hospital General de Agudos P. Piñero. Argentina
ABSTRACT
The benign fibro-osseous lesions include ossifying fibroma (OF). This condition is considered to be a true neoplasm consisting of an encapsulated proliferation of fibrous tissue that generally affects the jaws, especially the molar region of the mandible. Its growth is slow and it can cause tooth displacement, including dental rhizolysis.
In order to reach the diagnosis of OF, a clinico-radiologic correlation with intraoperative findings is required because the histology may be similar to other fibro-osseous lesions.
The case of a patient treated in our department for ossifying fibroma of the mandible is reported.
Key words: Ossifying fibroma; Benign fibro-osseous lesions.
RESUMEN
Dentro de las lesiones fibro-óseas benignas se encuentra el fibroma osificante (FO); esta entidad se considera una verdadera neoplasia que comprende una proliferación encapsulada de tejido fibroso; que afecta generalmente a los maxilares especialmente a la mandíbula en la región de molares. Su crecimiento es lento, pudiendo generar el desplazamiento dentario, incluso la rizólisis de los mismos.
Para el diagnóstico de FO se requiere de la correlación clínica-radiológica, con los hallazgos intraoperatorios; ya que la histología puede presentar similitudes con otras lesiones fibro-óseas.
Se describe el caso de un paciente tratado en nuestro servicio por fibroma osificante de maxilar inferior.
Palabras clave: Fibroma osificante; Lesiones fibro-óseas benignas.
Introduction
Benign fibro-osseous lesions include a group of clinically diverse bone disorders that share histopathologic characteristics. The replacement of normal bone by tissue composed of collagen fibers, fibroblasts, and a variable degree of mineralized tissue is characteristic of this group. Numerous classification models of these lesions have been proposed, of which the most widely recognized and accepted classification is that of Waldrom. This author divides benign fibro-osseous lesions into different categories: 1) developmental (hamartomatous), 2) reactive (dysplastic), and 3) neoplastic. Recently, Slater, Slootweg, Eversole, and Melrose have made recommendations and modifications to the classification proposed by Waldron.1 The following categorization is proposed:
Benign fibro-osseous lesions (modified)
1. Bone dysplasia
• Nonhereditary:
- Periapical
- Focal
- Florid• Hereditary:
- Familial gigantiform cementoma
2. Fibro-osseous neoplasms
• Conventional ossifying fibroma
• Juvenile, active, or aggressive ossifying fibroma
3. Fibrous dysplasia
• Polyostotic fibrous dys plasia due to endocrine disease (McCune-Albright)
• Polyostotic fibrous dysplasia
• Craniofacial fibrous dysplasia
The World Health Organization (WHO) classifies OF as a benign bone neoplasm of the craniofacial skeleton. It most frequently occurs in the jaw, but it also has been reported in the temporal and ethmoidal bones and orbital region. It generally presents between the second and fourth decades of life, more frequently in women. It is usually asymptomatic and facial deformity is the first clinical manifestation.2
Radiographically, a circumscribed unilocular lesion with a sclerotic margin appears in most cases, although multilocular OF has been reported. The appearance of the lesion depends on its maturity and may be radiolucent, radiopaque, or mixed.3
The histopathologic findings include dense fibrous connective tissue with variable degrees of cellularity. The stroma is relatively hypovascular and ovoid venules are visible. The bone is metaplastic and laminar trabeculae may be present but are not a constant finding.4,5
Treatment is complete surgical excision and the recurrence rate is low.
An OF variant has been described that affects children and adolescents. Its histopathologic characteristics are more complex and its growth tends to be aggressive: Aggressive juvenile ossifying fibroma (AJOF). The WHO defines AJOF as an actively growing bone lesion that affects people under the age of 15 years. It shows more predilection for the maxilla and consists of richly cellular fibrous tissue containing mainly fibrocytes and osteoblasts; osteoclasts are visualized in relation to the bone tissue. Two histologic varieties are described: 1) trabecular-desmo-osteoblastoma and 2) psammomatoid-desmoosteoblastoma. 6
The treatment of choice is surgical curettage. The recurrence rate is 30 to 58%.7
Clinical case
A 10-year-old male was referred to the Bucco-Maxillo- Facial Surgery Department of Hospital Piñero for study of an increase in the volume of the right mandibular angle over a two-week period. He had no medical history of interest. The mass was not tender and there was no paresthesia (Fig. 1).
The intraoral examination disclosed swelling of the vestibular and lingual table of the mandible. The dental pieces were apparently healthy and showed no mobility; the mucosa was of normal appearance.

Radiographically, the lesion was radiolucent and unilocular with sclerotic margins. Radicular resorption of piece 37 was evident (Figs. 2 and 3). Biopsy findings were consistent with ossifying fibroma, for which enucleation under general anesthesia was scheduled. Histopathologic study confirmed the ossifying fibroma (Figs. 4 and 5).
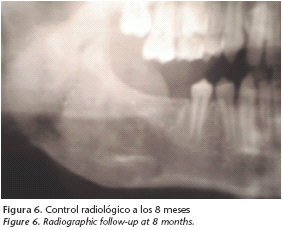
The most recent clinical and radiographic follow-up at eight months revealed favorable evolution of the patient and radiographic evidence of bone neoformation and increased basal mandible thickness. The patient continues under follow-up to detect tumor recurrence (Figs. 6 and 7).
Discussion
Ossifying fibroma, a term proposed by Montgomery in 1927, has been and continues to be a controversial topic in several ways: One point of controversy is the differentiation between OF and lesions of similar clinical and histologic appearance, such as fibrous dysplasia (FD) and focal osseous dysplasia (FOD). The importance of the diagnosis differential of OF with these benign lesions lies in the different treatment that each of these pathologies receives.1
What differentiates these lesions is that OF has a centrifugal growth pattern, generally erasing the basal mandible and producing dental displacement and/or radicular resorption.8 The intraoperative findings often are significant and have diagnostic value since OF tends to be enucleated intact as a solid mass. Biopsies that preserve relation between the cortical and the lesion are valuable for the histologic interpretation of these pathologies. The microscopic evidence of the margin is the key to differentiating OF, FD, and FOD.9
Another point of controversy is the differentiation of an aggressive, or juvenile, variant of the same pathology. Pathologists consider this diagnosis as subjective, arbitrary, and lacking in scientific support.10 Many authors consider AJOF to be a unique lesion that occurs in boys or adolescents and has more complex histologic characteristics and a tendency to behave aggressively.11 Nevertheless, reports on this pathology have established:
• Not all lesions described as AJOF occur in children and adolescents.
• Not all have aggressive local behavior.
• Not all lesions reported as AJOF have the same histologic characteristics.
The problem is distinguishing these aggressive varieties from conventional OF.
What is certain is that this diagnosis is confusing and controversial because OFs can grow to a considerable size and may not be histologically distinguishable from those with more limited growth. In addition, the histologic characteristics that supposedly separated AJOF, such as extremely cellular stroma, can vary from one tumor to another and the same characteristics can be observed in conventional OF.12 Myxoid tissue, cystic degeneration, and aneurysmal bone are not specific to AJOF; they may occur as reactive changes.13
Conclusion
The correct management of OF first requires a differential diagnosis with FD and FOD due to the different treatment that each of these conditions requires.
The treatment of choice of OF is tumor resection and follow- up, as was applied to the case presented here. FOD requires only follow-up and FD sometimes requires cosmetic surgery.
As for differentiating an aggressive juvenile variety, no consensus exists among pathologists on the exact criterion for defining this pathology. It is considered more prudent to individualize each particular case and highlight the histologic characteristics that may be related to aggressive local behavior in some of these cases.
Considering that the treatment indicated for any type of OF is surgical resection and follow-up, diagnosing AJOF is not particularly irrelevant.
![]() Correspondence:
Correspondence:
Dr. Antonio Lombardi
Servicio de Cirugía y Traumatología Buco-Máxilo-Facial
Hospital General de Agudos P. Piñero
Varela 1301 (Flores) c.p: 1406. Buenos Aires. Argentina
Recibido: 09.06.08
Aceptado: 17.12.08
References
1. Bannon R, Fowler C. Benign Fibro-osseous Lesions: A review of current concepts. Adv Anat Pathol 2001;8:126-43. [ Links ]
2. Gay Escoda C, Berini AL. Fibroma osificante maxilar: Presentación de un caso y revisión de la literatura. Med Oral 2004;9:333-9. [ Links ]
3. Eversole LR, Merrell PW, Strub D. Radiografic characteristics of central ossifying fibroma. Oral Surgery Oral Med Oral Pathol 1985;59:7-522. [ Links ]
4. Sciubba JJ, Younai F. Ossifying fibroma of the mandible and maxilla: review of 18 cases. J Oral Pathol Med 1989;18:21-315. [ Links ]
5. Waldron CA, Giansanti JS. Benign fibro-osseous lesions of the jaws: a clinical –radiologic-histologic reviwed of sixty-five cases. Part II Benign fibro-ossoeus lesions of periodontal ligament origin. Oral Surg Oral Med Oral Pathol 1973; 35:50-340. [ Links ]
6. Kramer Irh, Pindborg JJ, Shear M. Histological typing of odontogenic tumors. In: WHO International Histological classification of tumors. 2nd ed. Berlin: Springer- Verlag 1992:9-27. [ Links ]
7. Slootweg PJ, Panders AK, Koopmans R, et al. Juvenile ossifying fibroma. An analysis of 33 cases with emphasis on histopathologic aspects. J Oral Pathol Med 1994; 23:8-385. [ Links ]
8. Slater LJ. Fibro-osseous lesions. Oral and Maxillofacial Surgery knowledge Update 1995;1(Part II):33-47. [ Links ]
9. Eversole LR. Clinical outline of oral pathology: diagnosis and treatment. 3rd ed. Philadelhia: lea & Febiger 1992;436. [ Links ]
10. Sapp JP, Eversole LR, Wysocki GP. Contemporary oral and maxilofacial pathology. St. Lois: Mosby, 1997;88-125. [ Links ]
11. Slootweg PJ. Maxillofacial fibro-osseous lesions: classification and diferential diagnosis. Semin Diagn Pathol 1996;13:12-102. [ Links ]
12. Eversole LR. Craniofacial fibrous displasia and ossifying fibroma. Oral Maxillofacial Surg Clin North Am 1997;9:42-625. [ Links ]
13. Melrose RJ. The clínico-pathologic spectrum of cemento-osseous displasia. Oral Maxillofacial Surg Clin North Am 1997;9:53-643. [ Links ]











 text in
text in