Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.5 Madrid sep./oct. 2009
Multicentric prospective study of MG-OSSEOUS implants at 2 year follow-up
Estudio multicéntrico prospectivo con implantes MG-OSSEOUS a los 2 años de seguimiento
E. Serrano1, R. Martín-Granizo2
1 Cirujano oral y maxilofacial. Práctica privada de cirugía maxilofacial e implantes, Barcelona. España
2 Médico adjunto. Servicio de cirugía oral y maxilofacial. Hospital Clínico San Carlos, Madrid. España
ABSTRACT
Introduction. Implantology is the most common therapeutic procedure nowadays. Professor P.I. Branemark began this procedure in 1965 and got very bad results. Since the Harvard Consensus Conference, 30 years ago, showing and explaining the surprising criteria of the implant's survey, until now we have moved to the opposite side. All the rules are broken and they try to convince you by publishing some trials that are not scientific enough. We present this truly scientific trial using MG-OSSEOUS implants (Mozo- Grau SL, Valladolid, Spain) as a humble contribution, based on well defined and realistic clinical uses.
Material and methods. The Spanish company Scientific Management in O&SS (Barcelona) designed a complete questionnaire to be completed by the implantologist dealing with each clinical case. The compilation and statistical processing were extremely rigorous. Data was managed, from the total rate of implants (N), to conclude if it was possible to obtain true data of different samples, and using ANOVA, to analyze selected parameters from these samples, in order to see the direct relation between them and the failure of the implants.
Results. 1,475 dental implants were placed in 480 patients, between June 2005 and May 2006. The global implants success rate was 98.2% with an average of 2 years follow-up with the connected prostheses. The implants' position, length and diameter are detailed and the samples are also analyzed, as post extraction implants, immediate loading implants and implants associated with grafts.
Discussion. We focused on, completing an exhaustive revision of actual bibliographical sources, the high failure rate obtained by the wide diameter implants (4,25 mm) post extraction and on the versatility of the strength diameter implants (3,4 mm) to be placed anywhere in the mouth, with no mean of the type of prosthesis associated.
Conclusions. This trial can be defined as the philosophy's antithesis, in which we allow scientific and reproducible conclusions in implant surgery, our scientific truth. We will extend this trial to reach, at least, 5 years of follow-up.
Key words: Dental implants; Edentulism; Titanium; Self-tapped implants.
RESUMEN
Introducción. La implantología es uno de los procedimientos terapéuticos más realizados en nuestros días. El objetivo del presente estudio es presentar los resultados de los los implantes MG-OSSEOUS (Mozo-Grau, S.L., Valladolid, España) a los 2 años de seguimiento.
Material y método. La empresa Scientific Management in O&SS (Barcelona, España), diseñó unos cuestionarios exhaustivos que rellenaron, por cada caso, cada uno de los profesionales del estudio. La compilación y el tratamiento estadístico de los datos obtenidos fue extremadamente pormenorizada. Se aplicaron estudios de subpoblaciones desde la población N de implantes totales colocados y, mediante la aplicación de ANOVA, se valoraron parámetros concretos en dichas subpoblaciones para determinar y concluir la influencia de los mismos sobre el fracaso de los implantes.
Resultados. Se colocaron 1475 implantes en 480 pacientes entre Junio de 2005 y Mayo de 2006, con una supervivencia del 98,2% con un seguimiento de 2 años de promedio con las prótesis cargadas. Se detallan los implantes por posiciones, diámetros y longitudes y se analizan los resultados en las subpoblaciones de implantes postexodoncia, implantes de carga inmediata e implantes asociados a injertos.
Discusión. Se focaliza, realizando un amplio repaso de la bibliografía actual, en el alto fracaso obtenido en nuestro estudio de los implantes de diámetro ancho (4,25 mm) postexodoncia y en la versatilidad del empleo de los implantes de diámetro estrecho (3,4 mm) en cualquier posición oral para cualquier tipo de carga.
Conclusiones. Este estudio es la completa antítesis de la filosofía, en el que se interpreta de una sola manera, científica y reproducible, una serie de resultados en el campo de la implantología oral, nuestra realidad. Seguiremos este estudio para alargar el tiempo observacional, como mínimo, a 5 años.
Palabras clave: Implantes dentales; Edentulismo; Titanio; Implantes autoroscantes.
Introduction
Dental implant is one of the most common therapeutic procedures used in mouth rehabilitation. Perhaps the real perspective of this technique has been lost and we often find indicators of this procedure, many of them guaranteed by clinical studies that are not very consistent and whose scientific validity is doubted. Sometimes they are even contaminated by commercial interests.
Not even half a century since 1965 when Professor P.I. Branemark, orthopedic surgeon, started to give implants to patients after he made an accidental discovery in rabbits. There were problems with the still precarious technique that caused by Swedish patients and doctors from that time. Almost 30 years of Harvard's Consensus Conference where successful implant criteria were stipulated, bone reabsorbing of less than one third of the length of the implant and its mobility of 1 mm. (Albrektsson and Wennerberg 2005).
There are a lot of commercial houses that have published studies about dental implants. Although there is a great variety of work, results and methodology used in scientific literature the published works don't allow us to draw concrete conclusions that are not corrupted by commercial interests.
In this multicentric prospective study, carried out with MG OSSEOUS implants (Mozo-Grau S.L. Valladolid, Spain) a group of professionals have participated, performing a well discussed and responsible implant, without dangerous or heroic procedures. This conclusion is drawn after exhaustive analysis of the completed questionnaires that these professionals filled out. The questionnaires documented implant details for each patient. The purpose of this article is to show the results after a two year follow-up obtained with MGOSSEOUS implants that were placed in different situations between 2005 and 2006. This implant is a conic implant AUTORROSCANTE, made of pure titanium and with RBM surface treatment that is altered with biocompatible measures (calcium phosphate ceramic); the connection is made of compatible external hexagon.
This study is a modest contribution to recognize and concentrate the diretrix of successful implantation, based on stable criteria and honest studies.
Materials and method
The design and development of this multicentric study was directed by a business that is independent and specialized in this type of analysis and there is no relation with the maker of the material, Scientific Management in O&SS S.L. (Barcelona, Spain). Dental implants MG-OSSEUS (Mozo- Grau SL, Valladolid Span) were used.
After analyzing the variables to study a detailed questionnaire (Fig. 1) was designed and sent to each one of the professionals that had agreed to take part in this study without commercial interests. This questionnaire was used to collect complete information that included:
• Patients state of health (prior medical and oral health conditions).
• Preoperative state (complimentary tests, ferules, bone analysis according to the Leckholm and Zarb classification (1989), restoring the maxilla, previewed prosthesis).
• Implant placement (lengths, diameters, explicit techniques, stitches used).
• Associated grafts (bones, soft tissues, donor zones).
• Prosthetic plantation (materials used, complications, taking measurements, prosthetic design).
• Patient and Doctor satisfaction (expressed on a objective and reproducible scale).
• Detailed complications during and after treatments.
• Detail of complications during and after treatment.
• Special box for particular observations in each case for observations.
The professionals that intervened in this study filled out the questionnaire for each patient. The cases were carried out between May 2005 and June 2006. All of the patients have been controlled up until today's date without reporting any new incidences.
The data from the questionnaire was collected by two people and materialized into tables specially designed for this case. One of had no knowledge of implantology, the contrast between the two people in charge of collecting and classifying the information would make it very difficult for the skewing of information to go unnoticed. The treatment of the data was carried out objectively without extrapolating or supposing any results that would benefit this study. 49 implants cases were not included in the study because their questionnaires were not filled out properly.
We could not determine the proportion of men and women since the questionnaires did not include the names of the patients and 45% of patients did not report their sex.
In this study when we define failure we do so as decrease or loss of implant stability, even though they take into account the criteria defined by Smith and Zarb in 1989.
The protocol in this study is applied to each case was exhaustive and included:
• Orthopantogram of all the patients.
• Helicoid CT when grafts were used and when they wanted to have control over the alveolar inferior nerve canal. When there was more favorable bone availability the clinical evaluation was performed without CT.
• Model Studies in all cases was designed of complete and hybrid prosthesis like in immediate loading for partially fixed prosthesis, complete or hybrid.
• Surgery of models in cases with immediate loading of the partially fixed, complete or hybrid prosthesis.
• Surgical Ferule in those cases of immediate or differed loading, in 17.4% of the implants.
The objective of this study is to value the survival of the placed implants. When dealing with a study of 1,475 implants, N global populations, placed according to different indicators and techniques we present a statistically exhaustive treatment that we go into more detail about later.
The first objective was to carry out the calculation to determine, from population N of the total implants, the creation of dependent samples (n) with a sufficient number of implants in each one, in order to obtain statistically valid results that are independent from the initial populations. All of this is intended to carry out independent survival studies of the different samples considered, immediate loading (ni) and post extraction (np). In order to do this we apply the following considerations (Pita 1995):
•To get the size of the sample we should define what the standard of error is going to be to get the variance and establish the fluctuation of E (average value of the variaverage value of the same variable in population N).
• On the other hand, once it has been established if we can create independent and representative subpopulations from the N population of implants, we study the failure of those implants in each of them, using the normal analysis of the variance (ANOVA). Our questionnaire reports two comparative parameters factors: patient hygiene and the type of bone according to the Leckholm and Zarb classification (1985). With this we determine, regarding the same parameters of population N, if the failure is in these subpopulations (ni and np) is a casual factor or if it is influenced by one of these parameters.
Results
A total of 1,475 implants were placed in 480 patients with an average age of 53.7 years (15-88 years) between may 2005 and june 2006, with an average clinical and radiological follow-up of 2 years (from 19 to 29 months).
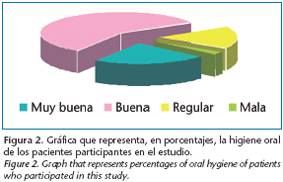
80% of patients had either good or very good oral hygiene (Fig. 2) and only 18% had periodontal disease (Fig. 3). The bones were predominant (according to Leckholm and Zarb 1995) type II (51%) and III (26%) (Fig. 4).
The length of the implants used in each of the restored dental positions is shown (Fig. 5), for example the diameter of each one of them in regards to the dental positions chosen (Fig. 6). In like manner these figures show the detail of length and diameter in absolute numbers. The length used the most was 13 mm, (40.5%) followed by 15 mm (27%). The most used diameter was 3.4 mm (36.3%) followed by 3.75 mm and 4.25 mm (both 31%).
Narrower diameters were used in the majority of cases in all positions, even in molar regions; they are the second option after 4.25 mm implants for superior maxilla implants.
After this average 2-year follow-up, 26 implants failed in 24 patients, which make up 1.8% of the total. The three variables of the subpopulation were analyzed which included patient hygiene, the type of bone where they were placed and the presence of periodontal disease (Fig. 7). The statistical analysis was performed using the ANOVA test, demonstrating that none of these two parameters is a dependent factor or conditional of failure of the implants. This changes notably when we analyze the hygiene of these patients (percentual expression with respect to the total number of implants in each patient), since ANOVA rejects the equality of these measures. Our study allows us to conclude that patients' hygiene is a determining factor in the failure of implants.
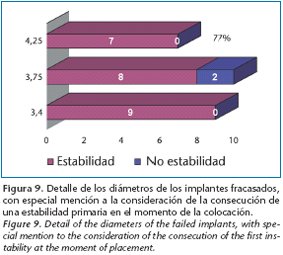
77% of failed implants were caused by an error in Osseo integration, periimplantitis is the cause in the remaining 23% (Fig. 8). The maxilla bone distribution reveals that 16 of the failed implants were located in the superior maxilla and 10 in the mandible. Analysis of the implants based on their diameters and the evaluation of their primary stability at the moment of placement by the implantologist is detailed in figure 9. Although implants with 3.4 mm diameter were the most often used, they are not the ones that have the most integration failure. Other factors have been analyzed it is this study that are showed independent from the failed implants (Table 1). 654 implant prosthesis´ were designed, with an average prosthesis/patient ratio of 1.4 and an average implant/prosthesis ratio of 2.2. The detail of the prosthesis type in total numbers as well as in percentages is in Fig 10, revealing that 46% were partially fixed prosthesis and 36% unitary. It is only related to prosthetic failure because of a screw fracture. The prosthetic survival in this study was 99.8%.
Post extraction implants
These implants have been called subpopulation np. The statistical calculation of variance and fluctuation of $ with respect to # applied to population N, this has allowed us to we can extract a series of results and conclusions. A total of 215 post extraction implants (np) that make up 14.6% of the total, in 79 patients (16.4%) of the patients in the study and 83 prosthesis were designed (12.7% of the total) over those post extraction implants. 67% were placed in the superior maxilla and 33% in the mandible. The figure 11 shows the distribution in both maxillas according to their dental positions.
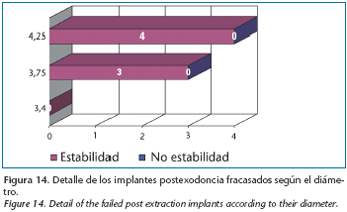
The diameters selected the most were 3.75 mm and 3.4 mm (Fig. 12). Mainly partially fixed and unitary prosthesis of the same proportion were designed both 36%) (Fig. 13).
7 implants failed in the 2 years of follow up and the global survival rate of the np subpopulation was 96.8%. Four failures happened in the superior maxilla and 3 in the mandible, they all happened because of failed Osseo integration. Figure 14 details the failure according to the distinct diameters, the percentage of failure for 4.25 mm in np is 7.3% and the percentage for all 4.25mm diameter implants is 1.5%. It can be deduced that the diameter is a determining factor in the failure of post extraction implants.
Other factors were analyzed to determine their implication in the failure of the post extraction implants (np): the type of bone and the hygiene of patients (Fig. 15). Using the application of the ANOVA statistical parameter we conclude that these factors are not determinant in the failure of post extraction implants.
Implants that immediately load
Another special consideration that we do in this study of immediate loading implants (Hourichi y cols. 2000: Malo and cols. 2003). Immediate loading implants are the ones that had prosthesis in the within 24-48 hours after their placement. This is according to the criteria described in the World Congress Consensus Meeting in Barcelona in 2002 (Aparicio and cols. 2003; Chochran and cols 2004).
Immediate loading took place in 58 implants (ni) in our study, 3.9% of the total. This small representation in regards to the global number of the subpopulation ni means that the results we obtain of this subpopulation won't be statistically guaranteed which will limit our ability to express results without the power to draw valid conclusion from them. 41 of these implants (71%) were placed in the mandible (Fig. 16). All the implants were longer than 10mm in length prevailing the ones that are 13mm (Fig. 17). In almost all of the cases implants 3.75 mm and 4.25mm in diameter (Fig. 18) were used.
32 prosthesis of immediate loading were designed, 50% of which were for partially fixed prosthesis and 44% for unitary. The rest were hybrid and complete mandible (Fig. 19). 97% of the prosthesis was cemented.
One implant failed that was 4.25 by 13 mm (1.7% respect to ni). It was an immediate post extraction, there was pain although there was no movement in patients with bruxism.9,10 Survival of the implants subjected to immediate loading in our series of follow up of 2 years was 98.3%.
107 implants (no) (7.2% of the total) along with a bone graft procedure in 55 patients (11.5% of the total) the autologous graft was used in 76% of the cases (Fig. 20). 61% were onlay bone grafts (Fig. 21) among the autologous bone grafts, 82% were particulated. In figure 22 the origin and donor zone of each one of them is detailed.
Discussion
Out of the results presented in this study, it is interesting to discuss two fundamental aspects. Given the statistical treatment applied, it is obvious we need to analyze the box of immediate loading since, because of the analysis of the variance and fluctuation of the ni subpopulation; the results are not extrapolated or reproducible. As a result a high survival rate (98.7%) after two years is not significant.
We analyze immediate post extraction implants, specifically the high failure rate seen in wide diameter implants (4.25mm and 4.1mm platform). So the use of narrow implants (3.4 mm and standard 4.1 mm platform) in any of the oral positions, since they have been the most used implants (36.3% of the total).
It is not easy to find a recent biography that analyzes the use of wide immediate post extraction implants. There is one study that demonstrates that there is more crestal bone reabsorbing compared to the use of implants with a standard diameter (Davarpanah, 2001).
If we analyze the morphological changes that happen in the alveolar bed after extraction, we will see that the horizontal distance and width of the lingual vestibule reduces between 5-7 mm in a period of 6-12 months. This represents almost 50% of the initial alveolar width. The majority of these changes take place during the first 4 months of scarring (Lam 1960). These biological data suggest surgical recommendations when carrying out extraction prior to placing an immediate implant. They are the maximum preservation of the alveolar walls especially the vestibular in the superior maxilla and the lingual of the mandible (Peñarrocha and cols. 2004). When an implant is placed in the floor after extraction we look for primary stability when drilling between 3 and 5 mm minimum above the apex of the alveolar bed, like using implants with a diameter that is slightly wider than the remaining alveolar process (Becker and Becker 1996). If implants with a wide diameter are used to decrease the distance between the bone and the implant surface, along with weakening the alveolar walls after extraction it seems that there is a greater possibility of bone reabsorbing by compression of a weak alveolar wall when a wide diameter implant is used. This could be the cause of the elevated failure index proportional to wider implants in immediate post extraction. Because of this it could be convenient to establish primary stability of the post extraction implants using a more apical drill for the alveolar bed in stead of compromising the alveolar walls with implants that are wider in diameter.
Many authors are in favor of discrete discrepancy between the surface of the implant and the alveolar walls, resorting to regenerative bone techniques intended to fill this space. Authors like Brugnami and cols, 1996 or Dealemans and cols 1997 recommend the use of autologous bone grafts to improve the bone inductive capacity. Other authors (Moscovitch 2001) propose and defend the use of 2 implants with smaller diameters for the restoration of post extraction alveolar bed in molar zones, avoiding compression of bone walls and using bone regenerative techniques.
Despite this, the 96.8% survival rate in the 2 year follow- up of these implants is similar to the results of Meta analysis by Chen and cols in 2004 when reviewing 18 studies that put survival between 89.9% and 100%.
It is also interesting to analyze the increased percentage of implants with a 3.4 mm diameter (narrow) used in any oral position, including restoring molars (mainly in first molars) in both maxillas. The narrow implants were commercially introduced in the 90's, initially used as transitional implants (Petrungaro and Windmiller 2001; Brown Tarnow 2001).
Today they are generally used for any type of rehabilitation. Various studies have show that they integrate the same way the ones with a standard diameter do. Results have been published with 6 and 27 months of follow- up that oscillate between 93% and 98% survival (English and Bohle 2003; Froum and cols. 2005; Cho and cols. 2007; Labarre and cols 2008). A study of 2,514 of these implants has a survival rate of 94.2% after 5 years.
The results of this study's 3.4mm diameter implant survival rate (535 placed, 9 failed with 98.3% survival alter 2 years) are very acceptable. After analyzing the high survival rates of the implants published in the literature it seems that their use is very useful and guarantees good or better results, in any position of the mouth, than the implants with a standard 3.75 mm diameter (451 placed, 10 failed with 97.8% survival after 2 years).
The current study of MG-OSSEOUS implants can be compared to other published studies in the literature, like those that are reflected in table 2.
Conclusions
A good study protocol that is personalized for each one of these indicators assures good final results. Implants with narrow diameters can be used in any oral position including the molar zone, mainly in the superior maxilla, with a survival rate of 2 years similar to the standard. The oral hygiene of patients is a factor that seems to condition failure of the implants although it doesn't seem to be a determining factor in failed immediate post extraction implants. The use of wide diameter implants (4.25 mm) in post extraction cases could be a risk factor for failure.
Acknowledgements
To the Dres. Juan Luis Alonso de Dios, Luis Antonio Hernandez Martin, Luis Naval Gías, Carlos Orduña Domingo, Salvador Ortuño Laguia, Juan Jose Rodriguez Ortega, Angel Sancho Garcia, Fermin Terron Miron y Marcos Terron Gonzalez for your disinterested participation in thisstudy.
![]() Correspondence:
Correspondence:
C/ Gran Via Carles III 58-60, esc A. At 1o
08028 Barcelona. España
E-mail: 31188esc@comb.es
Recibido: 24.06.2009
Aceptado: 30.10.2009
References
1. Albrektsson T, Wennerberg A. The impact of oral implants-past and future, 1966-2042. J Canad Dent Ass 2005;71:327. [ Links ]
2. Aparicio C, Rangert B, Sennerby L. Immediate/early loading of dental implants: a report form the Sociedad Española de Implantes World Congress Consensus Meeting in Barcelona, Spain. Clin Impl Dent Rel Res 2002;5:57-60. [ Links ]
3. Barajas Pinzón OM. Breve Historia de la Ingeniería Mecánica. Parte I. Ingenierias 2003;19:47- 53. [ Links ]
4. Becker W, Becker BE. Flap designs for minimization of recession adjacent to maxillary anterior implant sites. A clinical study. Inter J Oral Maxillofac Impl 1996;11:46-54. [ Links ]
5. Brown M, Tarnow D. Fixed provisionalization with transtional implants for partially edentulous patients: a case study. Pract Procc Aesth Dent 2001;13:123-127. [ Links ]
6. Brugnami F, Then P, Moproi H. Histological evaluation of human extraction sockets treated with demineralized freeze-dried bone allograft and cell occlusive membrane. J Periodontol 1996;67:821-825. [ Links ]
7. Chen ST, Wilson TG, Hämmerle CHF. Immediate or early placement of implants following tooth extraction: review of biologic bases, clinical procedures and outcomes. Int Jo Oral Maxillofac Impl 2004;19(suppl): 12-25. [ Links ]
8. Cho SC, Froum SJ, et al. Immediate loading of narrow diameter implants with overdentures in severely atrophic mandibles. Practical Proccedings of Aesthethic Dentistry 2007;19:168-174. [ Links ]
9. Cochran DL, Mortin D, Weber HP. Consensus statements and recommended clinical procedure regarding loading protocols for endosseous dental implants. Int J Oral Maxillofac Impl 2004;19(Suppl):109-1.3 [ Links ]
10. Davarpanah M, Martinez H, Kebir M, Etienne D, Tecucianu JF. Wide-diameter implants: new concepts. Int J Period Rest Dent 2001;21:149-159. [ Links ]
11. Dealemans P, Hermanns M, Godet F. Autologous bone graft to augment the maxillary sinus in conjunction with immediate endosseous implants: a retrospective study up to 5 years. Int J Period Rest Dent 1997;17:27-39. [ Links ]
12. English CE, Bohle GC. Diagnostic, procedural and clinical issues with the Sendax mini dental implant. Comp Cont Educ Dent 2003;24:3-25. [ Links ]
13. Froum SJ, Simon H, et al. Histologic evaluation of bone implant contact of immediately loaded transitional implants after six to 27 months. J Oral Maxillofac Impl 2005;20:54-60. [ Links ]
14. Hourichi K, Uchida H, Yamamoto K, Sugimura M. Inmediate loading of Branemark system implants following placement in edentulous patiens: a clinical report. Int J Oral Maxillofac Impl 2000;15:824-839. [ Links ]
15. Labarre E, Alhstrom R, Noble W. Narrow diameter implants for mandibular denture retention. CDA Journal 2008;36:283-286. [ Links ]
16. Lam RV. Contour changes of the alveolar processes following extractions. J Prosth Dent 1960;10:25-32. [ Links ]
17. Lekholm U, Zarb GA. Patient selection and preparation. En: Branemark PI, Zarb GA, Albrektsson T. Tissue-integrated prostheses: osseointegration in Clinical Dentistry. Chicago: Quintessence 1985. [ Links ]
18. Maló P, Rangert B, Mech Eng, Nobre M. «All-on-four» Inmediate-function concept with Branemark system implants for completely edentulous Mandibles: a retrospective clinical study. Clin Impl Dent Relat Rese 2003;5(Suppl 1):2-9. [ Links ]
19. Moscovitch M. Molar restorations supported by 2 implants. An alternative to wide implants. J Canad Dent Ass 2001;67:535-9. [ Links ]
20. Petrungaro PS, Windmiller N. Using transitional implants during the healing phase of implant reconstruction. Gen Dent 2001;49:46-51. [ Links ]
21. Peñarrocha M, Uribe R, Balaguer J. Implantes inmediatos a la exodoncia. Situación actual. Med Oral 2004;9:234-242. [ Links ]
22. Pita Fernández S. Epidemiología. Conceptos básicos. En: Tratado de Epidemiología Clínica. Madrid; DuPont Pharma SA; Unidad de epidemiología Clínica, Departamento de Medicina y Psiquiatría. Universidad de Alicante. 1995;p.25-47. [ Links ]
23. Shatkin TE, Shatkin S, y cols. Mini dental implants for long term fixed and removable prosthetics: a retrospective analysis of 2,514 implants placed over a fiveyear period. Com Cont Ed Dent 2007;28:92-100. [ Links ]
24. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosth Dent 1989;62:567-72. [ Links ]











 texto en
texto en