Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.5 Madrid sep./oct. 2009
What would your diagnosis be?
¿Cuál es su diagnóstico?
An 81 year-old woman with hypertension is being treated with calcium antagonists. She goes to oral and maxillofacial surgeries out patient department as recommended by her primary care physician. The presumed diagnosis is chronic Temporomandibular Joint disorder. The patient has been suffering for about 1 month from inflammation of the left preauricular region, pain when chewing, and progressive trismus. She does not report weight loss, fever disphagia or odynopagia.
During the physical exam we discovered a left preauricular parotid tumor measuring 4 cm in diameter, not inflamed, of stony consistency and not adhered to the skin but rather to the deep surfaces and slight pain upon palpation (Fig. 1). She does not report facial paralysis or cervical adenopathies. During an intraoral examination we measured an oral opening of 25 cm (from the maxillary gum to the mandible gum), advanced periodontal disease, multiple cavities and radicular remnants. Upon compressing the parotid serosa, saliva was thick.
The orthopantogram shows a compacted wisdom tooth in the ramus of the left mandible with a possible associated follicular cyst (Fig. 2).
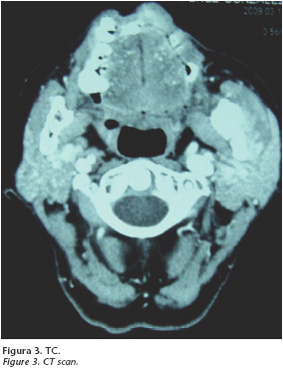
The CT reveals a diffused enlargement of the left masseter without abscessed collection, possible myositis, with sclerosis focus and a compacted tooth in the subjacent mandible. There are also bilateral cervical adenopathies with benign characteristics (Fig. 3).
The PAAF study results are "cellularity highly suggesting malignancy". The cytologist recommends a biopsy in order to obtain a definitive diagnosis. The operation is carried out under local anesthetic and nastrotraqueal tubation with a fiberscope. Local anesthetic and muscular relaxation do not improve oral opening. After removing all the teeth that are in a poor state we approach the included 38 intraorally using an inclined external left line. The ruptured zone of the lingual cortical is seen through the protrusion of the compacted wisdom tooth and an insufflation of the vestibular cortical. Tooth 38 is drilled with exodontics and a cystectomy is carried out using curettage of the cavity (Fig. 4).
The procedure is completed with the myotomy of the masseter muscle and the freeing of its insertion near the ramus and angle of the jaw. We send a fragment of the masseter that looks fibrous and devitalized for a biopsy.
Chronic submasseter secondary abscess of impacted wisdom tooth
Absceso crónico submaseterino secundario a cordal incluido
L. Pingarrón1, J. Arias2, V. Martorell3, E. Palacios1, N. Gisbert1, M. Burgueño4
1 Médico Residente.
2 Médico Adjunto.
3 Jefe Clínico.
4 Jefe de Servicio.
Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz. Madrid.
The intra operative biopsy is composed of severe and chronic inflammatory tissue with no tumor cellulosity. The oral opening after finishing liberation of the left masseter is 45mm (from maxillary gum to mandible gum). Finally hemostasia is carried out and the intraoral incision is closed.
Three months after the procedure the patient reports no symptoms, has an oral opening of 45mm and no pathologies are found during clinical examination.
Discussion
The limitation on oral opening with or with out TMJ pain is generally associated with a muscular or joint pathology, making it less common to be secondary to head and neck surgery, radiotherapy, extensive burns or maxillofacial traumas.1
At times, tumors and infections can start out with joint symptoms. The relative rarity of this clinical case can cause an erroneous diagnosis.2 The differential diagnosis in this case should be made mainly between TMJ pathologies, parotid tumors and chronic submasseter abscess.
Chronic TMJ appears in initial exploration of patients with trismus associated with a combination of pain when chewing and stony preauricular tumors near the condyle joint. The lack of mandible desviation or of disocclusion separates this diagnosis. The orthopantogram confirms the normal position of the condyle in the joint cavity. The differential diagnostic of parotid tumors is that they form like stony tumors and cause limitation of oral opening in the TMJ. They are made mainly of malignant tumors. Epidermoid carcinoma is the most common primary malignant parotid tumor among adults. This tumor appears as a stony mass, is slow growing and can be associated with pain symptoms (because of sensitive nervous affectation) and limited mandible functioning. Only in very advanced cases will we see general paralysis or facial paralysis.
The second parotid tumor that should be considered is the cylindroma or adenoid cystic carcinoma; in terms of frequency it follows the mucoepidermoid carcinoma. Different than the previously described tumor, this tumor usually starts with facial paralysis due to its great affinity for perineural invasion.
Metastasis parotids are 90% of head and neck tumors due to lymphatic dissemination and in 50% of these cases deal with melanoma metastasis.4
Any tumor is subsidiary to metastasis using hematogen of the parotid gland. An example of this is found in the literature in a published case of trismus and stony tumoration, its extremely rare initial appearance of parotid metastasis of cholangiocarcinoma.5 Despite this, adeno thyroid carcinoma is the carcinoma that metastasizes the parotid using hematogen the most.
The submasseter abscess is like a delimited infection, usually chronic, in patients with prior dental pathologies that are found between the mandible ramus and the masseter muscle.6
In 1948 Bransby-Zachary in his attempt to explain normal discoveries in physical examinations of patients that were suspected to have a parotid infection, was the first to describe the submasseter space.7 The submasseter space is a subdivision between the chewing spaces, which results in the division of the masseter muscle into 3 parts: superficial, middle and deep.
MacDougall8 carried out a study dissecting 141 cadavers and documented an area that lacked muscle insertion between the middle and deep portion of the masseter. This area makes up an area that could create an incomplete barrier to infection and provide a space where hidden abscesses with chronic symptoms could form and go unnoticed and be intra infradiagnosed by a specialist.9
Treatment delay could be prolonged for months or even years which results in the patient receiving incomplete cycles of antibiotherapy when they had prior periodontal pathologies or compacted wisdom teeth. This favors chronicity of the abscess and symptoms similar to those of parotid tumors temporal mandible disorders.6,9
This adds to the subtlety of the radiological discoveries, including CT which can make mistakes when determining the typical discoveries of the abscess. But radiological characteristics of masetero thickening and mandible ramus sclerosis are criteria that should make us suspicious of adjacent infection.10 An appropriate antibiotic treatment should be quickly established, the abscess should be drained with myotomy and the focus of the chronic myostis that cause restriction of mandible opening should be debrided.
Orthopantogram is the first radiological test that should be performed for differential diagnosis between the joint, odontogenic or parotid pathology.
![]() Correspondence:
Correspondence:
Lorena Pingarrón
Hospital Universitario La Paz
Po de la Castellana, 261
28046 Madrid, España
E-mail: lorenapingarron@yahoo.es
References
1. Abdel-Galil K, Anand R, Pratt C. Trismus: An unconventional approach to treatment. Br J Oral Maxillofac Surg 2007;45:339-40. [ Links ]
2. Ogi N, Nagao T, Toyama M. Chronic Dental Infections Mimicking Temporomandibular Disorders. Aus Dent J 2008;47:63-65. [ Links ]
3. Mathes ST. Tumors of the Head, Neck and Skin. Plast Surg. 2nd Edition 2006;5:69-90. [ Links ]
4. Conley J, Arena S. Parotid gland as a focus of metastasis. Arch Surg 1963;87:757. [ Links ]
5. Patrocinio LG, Patrocinio TG, Pacheco LF. Trismus as the first manifestation of cholangiocarcinoma. Med Oral Patol Oral Cir Bucal 2008;13:573-5. [ Links ]
6. Balatsouras DG, Kloutsos GM, Protopapas D. Submasseteric abscess. J Laryngol Otol 2001;115:68-70. [ Links ]
7. Bransby-Zachary GM. The sub-masseteric space. Br Dent J 1948; 84:10- 3. [ Links ]
8. MacDougall JDB. The attachments of the masseter muscle. Br Dent J 1955;98:193-9. [ Links ]
9. Seltzer SE, Wang AM. Modern imaging of the masseter muscle: normal anatomy and pathosis on CT and MRI. Oral Surg Oral Med Oral Pathol 1987;63:622-9. [ Links ]
10. Chronic Submasseteric Abscess: Anatomic, Radiologic, and Pathologic Features. Jones KC. Am J Neuroradiol 2003;24:1159-63. [ Links ]











 texto en
texto en