INTRODUCTION
The peripheral giant cell granuloma (PGCG) is considered a reactive lesion, characterized by mononuclear cells and osteoclast giant cells in a vascular stroma outside the bone1. First described as giant cell reparative granuloma by Jaffe in 19532, PGCG is not considered as a true neoplasm but a hyperplastic reaction to a local irritant stimulus. These lesions occur over a wide age range, affecting mainly women between the fifth and sixth decade of life3,4. PGCG is usually found on any part of the gingiva or alveolar mucosa more specifically in the incisive and canine region of the jaw. Clinically, it arises as an exophytic growth with sessile or pedunculated base, the color fluctuates from pale pink to bluish purple. There might be signs of slight erosion of the adjacent alveolar bone as well as ulceration of the mucosa1,4,5.
The present case report describes the clinical, radiographic and histopathological characteristics of a large PGCG, treated with surgical excision and with no evidence of recurrence at 12 months.
CASE PRESENTATION
A 64-year-old female was referred to pathology service of the faculty of dentistry of the autonomous university of Chihuahua, Mexico, complaining of having a "small lump for 4 weeks". The patient mentioned she has been diagnosed with schizophrenia for 40 years, and she is at the moment controlled by multiple antipsychotic medications. She mentioned to have undergone a tooth extraction and after a week she noticed the area was swollen. After extraoral inspection a swelling of the anterior area of the maxilla was identified, which was associated to the previous tooth extraction.
The intraoral examination revealed a single irregularly shaped swelling lesion on the anterior portion of the maxilla of approximately 7 x 5 x 5 cm width-length, reddish in color, firm consistency, ulcerated surface, pedunculated base, defined edges and asymptomatic (Figure 1).
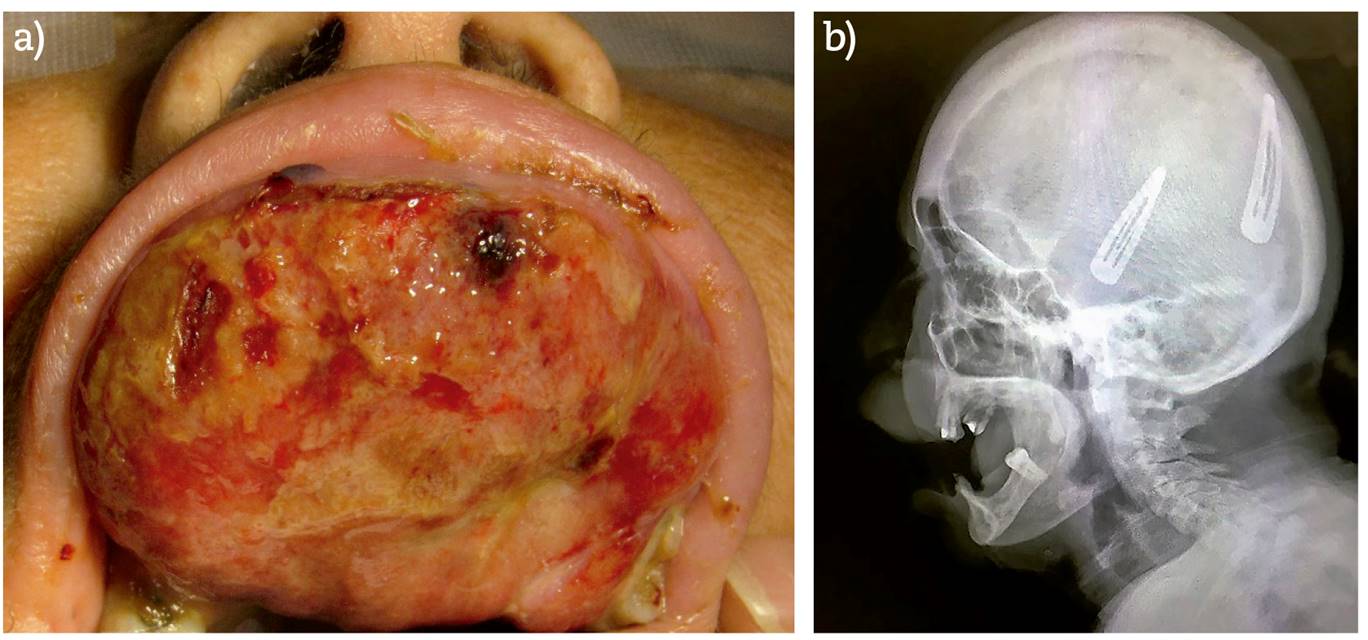
Figure 1. a) Clinical intraoral presentation of swelling site in the anterior area of the maxilla. b) X-ray lateral view of the skull. No evidence of bone involvement.
No sign of bone involvement was found in either orthopantomograph or lateral skull x-ray (Figure 1). Based on the clinical and radiographic findings, the following were proposed as a presumptive diagnosis: PGCG, pyogenic granuloma and peripheral ossifying fibroma. Excisional biopsy under general anesthesia was the treatment choice suggested by the surgeon.
There was abundant bleeding during the surgical procedure which was controlled by cauterization using an electrocautery. The adjacent bone showed slight erosion, therefore, conservative curettage was performed.
The histopathological report of the biopsied specimen (Figure 2) identified a benign lesion derived from the mesenchymal lineage, characterized by the diffuse and perivascular proliferation of multinucleated giant cells (osteoclast-like-cells), arranged on a layer of numerous spindle cells. Additionally, abundant blood vessels were found covered by stratified squamous epithelium. The above histology findings confirmed the diagnosis of PGCG.

Figure 2. Histopathological micrograph of the PGCG. a) 40 X magnification, benign lesion of menschymatous strain. b) 400 x magnification, diffuse and perivascular proliferation of multinucleated giant osteoclast cells (*), arranged on a layer of spindle cells composed mostly of ovoid and fusiform mononuclear cells (**) the lesion had abundant blood vessels and was covered by stratified squamous epithelium.
DISCUSSION
Due to the high vascularization of the lesion, the risk of bleeding and the mental condition of the patient, which could generate some complication of the procedure, the surgical team decides to perform the excisional biopsy through general anesthesia. In the surgical act, the bleeding control was properly carried out, so this led the surgeon to perform the removal of the lesion in a single surgical time3,6.
Some of the aspects of the PGCG lesion described in this case report such as: age, gender, color and other visible features are very similar to the typical clinical and histological characteristics described elsewhere. However, there are several bone lesions associated with the presence of multinucleated giant osteoclast-like cells, such as central giant cell granuloma, brown tumor of hyperparathyroidism, anuerismatic bone cyst, among others. The main characteristic of these lesions is their intraosseous involvement. The present case showed no bone alteration and with this finding, as well as laboratory studies related to bone metabolism, intra-bone lesions could be ruled out. The GPCG may have bone resorption, but this is commonly limited to the periphery of the alveolar ridge5,7.
There have only been a few reports of PGCG cases which have dimensions greater than 5 cm3,6. For instance, Mannem and Chava described a very similar case in 2012, a 65-year-old patient with a swollen purple lesion located on the left side of the jaw. The reported dimensions were 6 x 5 x 5 cm. The chosen treatment was excisional biopsy during which an unexpected hemorrhage occurred at the time of extirpation but was easily controlled with cauterization procedures to achieve hemostasis3.
On the other hand, in 2011, Khatry et al. reported a case of PGCG in a 30-year-old male patient, the dimensions of the lesion were 5 x 4.5 cm, in which no complications were encountered during surgical excision8.
The etiology of PGCG is still uncertain, however, there have been some factors outlined that are highly associated with its development and growth. In this specific case report, it is presumed that poor oral hygiene, hyposalivation, (which is believed to increase the growth and fast evolution of this lesion) added to various antipsychotic medications (which are known to reduce salivary flow) and the constant irritation of the mucosa caused by smoking, are crucial factors that might have boosted the development and fast growth of the lesion1,4,5,9.
The first-choice treatment is surgical excision with curettage on the base of the lesion and elimination of local factors of irritation, as well as, an important improvement of oral hygiene. The reported recurrence varies from 12% to 16%, which suggests that curettage or conservative peripheral osteotomy should be performed in most of the cases to avoid recurrence of the lesion 4,10,11.
The peripheral granuloma of giant cells is a reactive lesion of rapid growth and ulcerated surface, these characteristics can be similar to neoplasic lesions, so the timely and early diagnosis of this type of lesions will allow an appropriate and less invasive management of adjacent tissues10.














