Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Cirugía Oral y Maxilofacial
versión On-line ISSN 2173-9161versión impresa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.42 no.3 Madrid jul./sep. 2020 Epub 13-Oct-2020
https://dx.doi.org/10.20986/recom.2020.1140/2020
ORIGINALS
Planning, results and anatomy of the upper airway in obstructive sleep apnea/hypopnea syndrome after bimaxillary advancement: 20 cases
1Maxillofacial Surgery Department, Hospital Universitario Cruces, Barakaldo. Maxillofacial Surgery Group, Biocruces Bizkaia Health Research Institute, Barakaldo. Estomatología I Department, Medicine and Dentistry School, University of the Basque Country, Leioa, Spain.
2Cirugía y Especialidades Médico Quirúrgicas Department, University of Oviedo, Oviedo, Spain.
3Pneumology Department, Hospital Universitario Cruces, Barakaldo, Spain.
4Radiology Department, Hospital Universitario Cruces, Barakaldo, Spain
Objectives:
To present the working protocol, clinical outcomes and upper airway changes of a 20-patient cohort with moderate-severe obstructive sleep apnea/hypopnea syndrome undergoing maxillo-mandibular advancement with counterclockwise rotation.
Material and methods:
A multidisciplinary committee determines the surgical indication, which patients consent. Computed tomographies and polysomnographies are performed before and after surgery, as the usual clinical practice protocol. The clinical investigation ethics institutional review board approved the study. Lengths, volumes, minimum area, antero-posterior dimension, transverse dimension and other measurements are determined in the upper airway. Statistical analysis is descriptive and comparative by pairs with p < 0.05.
Results:
Planned movements are 10.40 mm of advance and 2.11 mm of anterior impaction. Apnea/hypopnea index reduces by 30.50 points and minimum peripheral capillary oxygen saturation increases by 5.00 points. Clinically and statistical significant findings are: 10.98 mm of shortening and 6.26 mm3 of volume enlargement, especially in the retro-palatal compartment; 91.45 mm2, 3.68 mm and 8.00 mm of area, antero-posterior dimension and transverse dimension widening respectively; hyoid bone advances 1.92 mm.
Conclusions:
Maxillo-mandibular advancement with counterclockwise rotation in moderate-severe obstructive sleep apnea/hypopnea syndrome achieves in short-term follow-up apnea/hypopnea index < 15 in 80 % and minimum peripheral capillary oxygen saturation > 85 in 75 % of our series. Main upper airway changes are: shortening, volume and area increase, elliptical shape, and antero-superior hyoid bone movement.
Keywords: Sleep disolver; OSAHS; orthognatic surgery; maxillo-mandibular advancement; counter clockwise rotation
INTRODUCTION
Symptoms and consequences of obstructive sleep apnea/hypopnea syndrome (OSAHS) are the result of repetitive upper airway (UA) collapse. Before starting any conservative or invasive treatment, diagnosis must be confirmed and severity characterized by a nocturnal polysomnography (PSG) performed in a specialized laboratory. Continuous positive airway pressure (CPAP) is the gold standard treatment for moderate-severe cases. In the last decades, mandibular advancement devices (MAD) have also been globally introduced. Before considering any surgical procedure, it is advisable to reevaluate anatomy, comorbidities and patient's desire. In addition, the indication should be discussed in a multidisciplinary committee1,2). Maxillo-mandibular advancement (MMA) especially if associated with counterclockwise rotation (CCW) widens the overall UA and stretches surrounding soft tissues. Although it is an invasive treatment, it has been reported reduction of the apnea/hipopnea index (AHI) to normal values in 75-100% of cases in short-term and medium-term follow-up1,3,4,5. Our working protocol, evaluation of clinical outcomes and a pilot retrospective observational study of UA morphological changes are presented. It is intended to corroborate that our findings, based in a 20-patient cohort with moderate-severe OSAHS undergoing MMA with CCW, are consistent with the current literature.
MATERIAL AND METHODS
Inclusion criteria are: ≥ 18 y/o, moderate-severe OSAHS in non-specific or supine position, indication determined by a sleep pathology committee (pneumology, otorynolaryngology, maxillofacial, dentistry, radiology, and neurophysiology), and written informed consent for surgery. Exclusion criteria are: pregnant woman, predominant apneas of central origin, major craniofacial deformities (such as cleft palate, severe asymmetric malocclusion, trauma or head & neck oncologic surgery), and different surgery than MMA. The study protocol was reviewed and approved by the institutional review board of clinical research ethics "OSI Ezkerraldea-Enkarterri-Cruces", code CEIC E19/39, and it is in compliance with the Helsinki Declaration. Patients signed a specific consent form conveniently informed for the study. Clinical outcomes and UA morphology are analyzed, based on PSG and head & neck computed tomography (CT) as complementary examinations of the usual clinical practice. They were performed a maximum of 3 months before the MMA and postoperatively between the third month and the first year. Diagnosis, treatment and complementary examinations took place between 2012 and 2017 in a single third-level health center.
Surgical planning
Once the surgery indication is established, a cephalometric analysis is performed: facial and intraoral photographs, lateral teleradiograph of the cranium (LTC), orthopantomography and plaster dental models6. When we consider the patient is prepared from an oral health point of view and occlusally, a CT is performed. From the axial series and current dental models, a digital dental-cranium-facial mesh is segmented and oriented according to the natural plane of the head and clinical exploratory data. Lefort I maxillary osteotomy, Obwegeser-Dal Pont mandibular split, and movements pivoted on the upper central incisor (UCI) are planned in three-dimension (3D), fitting the most stable occlusion, which will be the same as the initial one if pre-operative orthodontics has not been implemented. Repositioning surgical devices, either standard occlusal splints or customized cutting-perforating guides and preformed plates, are designed and manufactured by computer-assisted technology. Other simultaneous skeletal procedures could also be digitally plotted and measured. Genioplasties are considered for achieving the best patient's profile and correct frontal asymmetries; while genioglossus advancements are proposed when there is a huge retro-glossal (RG) collapse and the dental-osseous mandibular anatomy is favorable7,8,9. The first author is the main surgeon regarding planning and techniques' execution.
Examinations standardization
PSG is performed according to the national pneumology society recommendations10. CT (Philips Brilliance CT®, 16 detectors) are: non-contrast, helical, 1 mm axial slices, patient awake, supine position, still, no swallowing, apnea at the end of exhalation, relaxed lips, lingual tip in contact with UCI, mandible centric relation, and complete inclusion of the hyoid bone and cranium.
General data and clinical outcomes
There are collected epidemiological data (sex, ethnicity and age at the time of MMA), exploration data [body mass index (BMI), Mallampati scale and Angle class], previous surgeries and orthodontics, simultaneous MMA procedures UA related, and repositioning system of the osteotomized maxillary segments. The advancement is recorded at the UCI and at the Pogonion (Pog), the anterior vertical movement (AVM) at the UCI, and the posterior vertical movement at the first upper right and left molars. It is registered from PSG the apnea/hipopnea index (AHI) in non-specific, supine and non-supine position; and the basal and minimum peripheral capillary oxygen saturation (SPO2) parameters. Mild OSAHS is considered with 5-15 AHI and daytime sleepiness symptoms, moderate one with 16-30, and severe >301,2.
UA variables: (NemoTec FAB® software, 2.7.0 version)
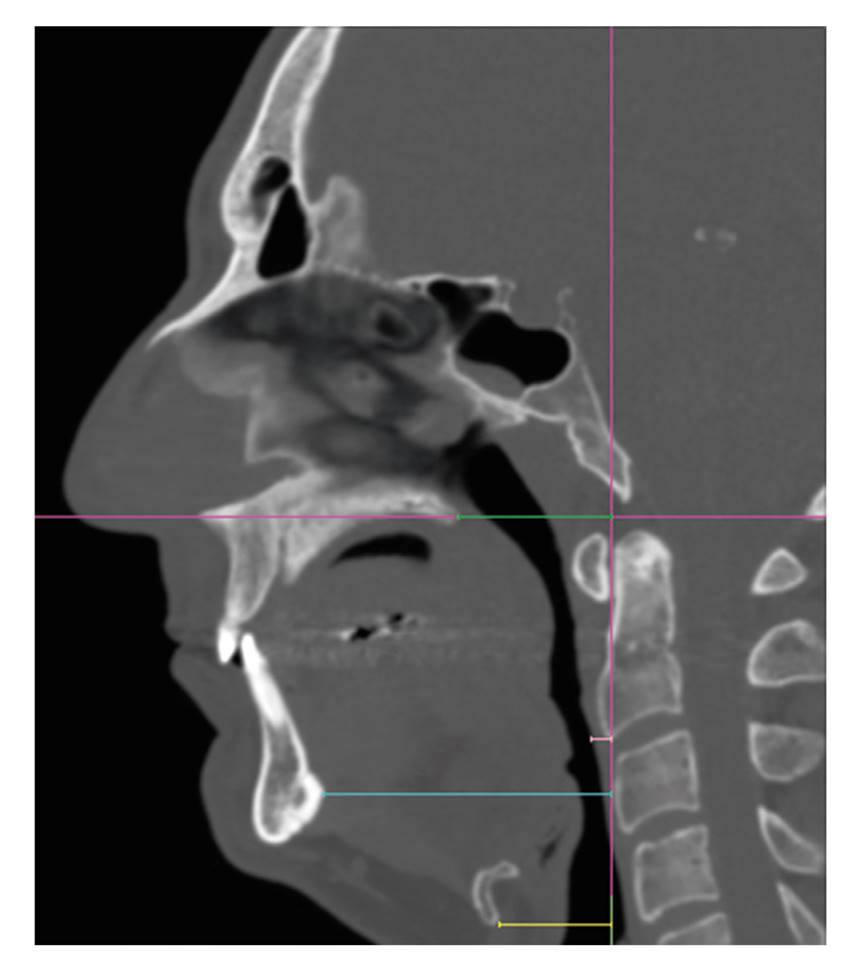
The cranium-facial mesh of each patient is oriented in the axial plane by aligning the nasopalatine duct with the odontoid process, which is aligned at the same time with the base of the crista galli in the coronal plane. In the mid-sagittal one, the horizontal main reference is the hard palate (HP) plane, while the vertical main reference is the perpendicular plane that crosses through the most antero-inferior point of the second cervical vertebra (AIC2) (Figure 1). Parallel planes to the HP one that pass through the uvula's tip (UT), epiglottis' tip (ET) and the antero-inferior point of the hyoid bone (AIHB) divide the UA into 3 compartments: retro-palatal (RP), RG and hypopharynx (HPh). Parallel to the vertical reference, lengths (L) are measured by compartments, the sum and the total independently. An air mesh is segmented wich limits are: superior HP plane, inferior AIHB plane, anterior soft tissues excluding the oral cavity air, posterior pre-vertebral musculature, and lateral para-pharyngeal musculature. Volumes (V) are calculated as a result of an air density point approximately -1000 HU and a range of +/-500 HU, also by compartments, the sum and the total independently (Figure 2). In axial slices parallel to the HP, we record the minimum area (AR), its location, and dimensions (D), understood as maximum antero-posterior (AP) and transverse (TV) straight distance of air density (Figure 3). In addition, horizontal distances parallel to the HP plane from the AIC2 one are quantified: posterior nasal spine (PNS), mental spine (MS), AIHB and pre-vertebral soft tissues (PST) at the height of the AIC2 (Figure 4). All measurements are carried out by the second author.

Figure 1. Case 11 pre-operative. Sequential orientation method in axial (A), coronal (B, C) and mid-sagittal (D) planes. Mid-sagittal plane in white and reference planes in magenta.

Figure 2. Case 15 pre-operative (A-D) and post-operative (E-H). Mid-sagittal slices. Determination of vertical lengths and volumes. Reference planes in magenta. Reference point and total length in yellow. Retro-palatal length in light turquoise, retro-glossal length in grayish blue, and hypopharynx in lavender. Limits of the drawing for the volume estimation in blue (total and by compartments), delimitation of the airway mesh in light pink. Location of the minimum area in green.

Figure 3. Case 16 pre-operative (A) and post-operative (B). Axial slice at the level of the minimum area, drew in light pink. Antero-posterior dimension in dark pink and transverse dimension in yellow.
Statistic analysis: (SPSS® software, 23.0.0 version)
Descriptive statistics of frequencies are calculated. Furthermore, a comparative by pairs' analysis of the dependent (pre- and post-operative) continuous variables is carried out. The normality of the variables is verified with the Kolmogorov-Smirnov test, so the parametric (dependent-samples Student's t) or non-parametric test (Wilcoxon signed rank) is applied, with p < 0.05.
RESULTS
Male/Female ratio is 19/1.100 % are white-Caucasian with a mean age of 41 (32-52) y/o. 45 % have BMI >25, 85 % Mallampati's III-IV and 45 % no maloclussion. 60 % had not undergone surgeries UA related prior to MMA and 85 % neither did pre-operative orthodontics. Five patients undergo genioplasty and one genioglossal advancement simultaneously to the MMA. All surgeries proceed without intra-operative incidents. Maxillary repositioning is with occlusal splints in 20 % of the cases, while in the rest is performed with customized systems of guides and plates. The mean planned advancement at the UCI is 10.40 mm (9.70-11.00), with 2.11 mm (7.00-1.00) of AVM and posterior leveling, thus carrying out the CCW so the Pog is 14.60 mm (11.30-22.30) pushed forward (Table 1).
Table I. General data and planning movements

1.6: first upper right molar. 2.6: first upper left molar. Adv: advancement. AVM: anterior vertical movement. BMI: body mass index. Cau: Caucasian. CCW: counterclockwise rotation. ESS: endoscopic sinus surgery. F: female. M: male. mm: millimeters. MMA: maxillo-mandibular advancement. Ortho: orthodontics. Pog: Pogonion. PVM: posterior vertical movement. UCI: upper central incisor. SARPE: surgical assisted rapid palate expansion. Sx: surgery. y/o: years-old.
The overall AHI is significantly reduced by 30.50 points of median after surgery while in supine position by 51.00 points. This supposes AHI < 15 in 80 % and < 5 in 50 % postoperatively. There are some absent data in supine and non-supine position if the patient maintained the same position during PSG. Although the basal SPO2 does not change, the minimum one improves 5.00 points of median, that is to say SPO2 > 85% in 75 % of the cases (Table 2).
Table II. Polysomnographies

AHI: apnea/hypopnea index. BAS: basal. K-S: Kolmogorov-Smirnov test. MIN: minimum. NSUP: Non-supine position. p: significance. POST: post-operatory. PRE: pre-operatory. sd: standard deviation. SPO2: peripheral capillary oxygen saturation. SUP: supine position. t: dependent-samples Student`s t test. W: Wilcoxon signed rank test.
The clinically and statistically significant changes in the UA include 10.98 mm of total L reduction of mean, especially in the RP location although it decreases in all compartments. Total V enlarges 6.26 mm3 of mean, doubling in RP location and without statistical significance in HPh. The error range between the difference of the total and the sum of compartments is < 1 mm for L and < 1 mm3 for V. Minimum AR, RP located in 85 % of pre-operative CTs and in 55 % of post-operative ones, increases 49.72 mm2 of mean, almost tripling. D-TV widens more than D-AP, suggesting an elliptical-shaped expansion, with differences of 8.67 mm and 3.62 mm of mean respectively. There is a significant increase in horizontal Ls, to highlight L-AIHB, which implies a more anterior position of the hyoid bone. It also ascends, due to the overall UA vertical shortening. Although the L-PST reduction is statically significant, it is not clinically because the difference is < 1mm of mean and median (Table 3).
Table III. Vertical lengths (in mm), volumes (in mm3), areas (in mm2), dimensions (in mm) and horizontal lengths (in mm)

AIHB: antero-inferior hyoid bone. AR: area. D-AP: antero-posterior dimension. D-TV: transversal dimension. HPh: hypopharynx. K-S: Kolmogorov-Smirnov test. L: length. p: significance. MIN: minimum. MS: mental spine. PNS: posterior nasal spine. POST: post-operatory. PRE: pre-operatory. PST: pre-vertebral soft tissue. RG: retro-glossal. RP: retro-palatal. sd: standard deviation. t: dependent-samples Student`s t test. TOT: total. W: Wilcoxon signed rank test.
DISCUSSION
According to Standford's stepwise-surgery protocol for OSAHS, MMA was initially part of a phase II of management11,12. It was considered whether other surgical procedures had failed, mainly focused on soft tissue of UA specific locations. Nowadays, it is considered as primary treatment, as a single surgery approach with an overall impact in UA, in patients with dental-facial deformities predisposing to collapse such as retrognathia, maxillary hypoplasia or overjet. It will be a secondary treatment in the presence of CPAP or MAD intolerance4,5. MMA intends to widen RP and RG regions by antero-superior traction of the PNS and MS, insertions of the velo-pharyngeal and suprahyoid musculature. In addition, it also stretches the para-pharyngeal musculature13. In refractory cases, there is already a Standford's phase III that includes hypoglossal neurostimulation14. Although it has been demonstrated AHI clearly improves in OSAHS after MMA, most of the studies reported have heterogeneous presentation of planning, technique details, clinical outcomes and UA morphological evaluation15.
Regarding planning, just like other surgical cases of dental-facial deformities without OSAHS, three basic pillars should be balanced: occlusion, aesthetics and UA. Current usual clinical practice is working with digitized 3D radiology, which provides more information and allows greater control and accuracy than 2D, especially in frontal planes6,9The tomography par excellence to assess cranium-facial bones is the cone-bean one (CBCT). However, we believe it is still more reliable a helical medical CT in OSAHS patients, gaining more soft tissue resolution and possibly more precision in UA segmentation too, at the cost of more radiation exposure. These surgeries have great impact on health and psychosocial aspects because of implicit aesthetics, so CBCT/CT is sometimes considered not only for planning, but also for the initial cephalometric analysis and post-operative control, achieving an entirely 3D evaluation16. We perform the first control with CT in OSAHS patients, but not the initial study or successive reviews.
We should take into account differences in OSAHS population compared to general one who goes through orthognathic surgery. OSAHS patients are usually middle-aged adults in the fourth-fifth decade, with body positional compensations to facilitate air flow such as hyperextension and anterior cervical translational movement, more anesthetic risk, more cardiovascular risk factors and more cardiac, respiratory and neurological comorbidities2. There is a tendency for maxillary bi-retrusion and bone atrophy with aging due to loss of the trabecular layer, making osteotomies more complex. Facial profiles tend to be convex with more soft tissue laxity, tolerating traction relatively well, but less predictable in regard to cosmetic changes with the standard cephalometric and morphing estimations, which are focused on young adult population17. With regard to dental-oral health, many OSAHS patients are mouth breathing and there is a greater teeth attrition, more crown reconstructions, more dental implants, more edentulous sectors, more large dental compensations, worse periodontal status with greater risk of gingival retractions and dental vitality losses. As for orthodontic appliances, OSAHS patients may sometimes not need nor wish to carry out dental movements, so no changes will happen in pre-operative and post-operative occlusion. However, there will be situations where for guaranteeing a stable occlusion it is essential a minimum decompensation, arch coordination and tooth carvings. Rigid arches with strong anchor pins are placed before surgical procedure in all cases, to hold the inter-maxillary fixations during the osteotomized segments positioning with conventional splint systems and to carry out post-operative orthodontic adjustments, which is necessary nearly always18.
MMA movement should be the maximum that allows occlusal stability, enough bone contact between osteotomized segments to achieve consolidation, reliable vascularization thought soft tissues after their detachment and traction, and reasonable cephalometric measurement. A common reported complication is protrusive profiles, although they are usually favorably accepted due to its rejuvenating connotation17.
As technique particularities, sometimes the upper-maxilla needs to be segmented into several fragments in the face of transverse hypoplasias. We perform H-shape segmentation. If transversal discrepancy is greater than 5-8mm, we would prefer surgically-assisted palatal expansion technique, delaying MMA to a second procedure (case 5). In pre-operative small noses, we consider sub-spinal Lefort I osteotomies, which try to preserve the perinasal musculature and modify lesser the base and nasal tip. Mandibular osteotomies at buccal bone level should not be too posterior, at least between the second and first molar, to assure enough bone contact during osteosynthesis. When the osteotomized segments are anteriorly pulled, bone interferences and soft tissue attachments should be removed, carefully not to compromise vascularization. It stands out the complete release, but not ligation, of the greater palatine pedicles in the upper-maxilla, while in the mandible it is to highlight the detachment of the basilar cortical periosteum and the pterygoid-masseteric sling preserving only its posterior attachment.
CCW enhances the MMA, widening the RP region further and also the RG because of the more antero-superior mandibular repositioning with the maximum facial bony impact at the Pog, compensating situations in which we do not reach the recommended 10-12mm of advancement at the UCI19. Caution should be taken with posterior gaps in the upper-maxilla, requiring sometimes bone grafts or additional osteosynthesis in the zigomatico-maxillary buttress. Palpable defects could happen in the mandibular basilar edge. There is also a risk, especially if there was not pre-operative orthodontics, of reduced incisor exposure and posterior gummy smile20.
Traditional method of osteotomized maxilla segments repositioning is by means of occusal spints. Navigator systems and custom-made guides and plates have been developed in the last decade. Their utilization could reduce surgical times and provide better control of the vertical dimension and condyle position. Absolute certainty is required that the pre-operative mandibular centric relation records are all right for the design and manufacture of these custom-made devices. A disadvantage is the greater economic expense they entail. These could be justified in OSAHS patients, due to the large movements required, leading to more complex segments stabilization than conventional orthognathic surgery cases. We perform the maxilla-first osteotomies with these systems, while we prefer mandible-first procedures with occlusal splints, so that the intermediate splint would not be too thick because of the open bite generated with the CCW7,8.
Other complementary procedures with implications in UA could be performed using the same intraoral approach of MMA. Septoplasties and turbinectomies aim to improve the air flow though the nasal cavity. Bone remodeling and widening of the pyriform aperture could be carried out before completing the maxillary osteosynthesis, carefully so it is not compromised the nasal-maxillary buttress and pre-maxilla bone where the plates and screws will be placed. Genioglossal advancements and elevated sliding genioplasties (Figure 5), in addition to improving facial cosmetics, project MS even more by pulling antero-superiorly the genioglossal and geniohyoid musculature. These two techniques should always be done after the MMA is completed. Uvulopalatopharyngoplasties associated with MMS have velopalatine incompetence risk13. Therefore, excisions should be very conservative, only in patients clearly with soft tissue excess, always before MMA, and limited advancement by convex protrusive profiles which are more frequent in asian or black ethnicities than white-Caucasians20.

Figure 5. Cases 17 (A-D) and 20 (E-H). Cranium-facial meshes and detail pictures in mid-sagittal slice. Pre-operative and post-operative, maxillo-mandibular advancement with counterclockwise rotation, associated to genioplasty and genioglossal advancement.
In regard to UA morphology after MMA, several studies have reported quantitatively changes in nasal cavity (NC), nasopharynx (NPh), RP, RG and HPh. Most promising findings are located in RP and RG and in relation to the hyoid bone position19,21. NC, oral cavity and NPh are left out of account in our analysis, due to the tremendous anatomical variability and complex margin delimitation of these locations. The main issues are the examinations' standardization [LTC, CBCT, CT or magnetic resonance imaging (MRI)], the 3D segmentation method and the measurements' acquisition, often poorly specified and hardly reproducible22. In general, the same references are taken for cephalometric diagnosis, movements' planning and UA measurements: Frankfurt plane, natural head positioning and true gravitational vertical plane23,24,25.. Nevertheless, posterior soft tissues contain the UA that could modify its morphology because of the following cervical spine movements: flexo-extension, translation, rotation and transverse bending. It is a critical limitation, since although radiological examinations might be well-standardized, cervical positioning is not assured. A cranium-facial-cervical positioning mask is a possible solution, but we have not found any study that works with it. Other option is to use a 3D landmark (both hard and soft tissue structures) localization methodology which provides reliable segmentation and accurate measure of volumes, cross-sectional areas and linear distances. Previous reports such as this study use this kind of method, but it is to be mentioned ours is with medical CT in supine position while the others are with CBCT and the patients usually sitting22,23,24,25.
It stands out the following comparative pre-post-operative studies in OSAHS patients, with methodologies similar to ours and consistent with our results too. Faria et al. 23 report by MRI a V increase of 26.72 % in RP and 27.20 % in RG. The same group by LTC concludes that each mm of advancement implies a RP gain of 0.76 mm and a RG one of 1.20 mm; and also reports a more superior hyoid bone position. Zinser et al.24 using CTs present significant results of: UA shortening, V increase, more elliptical shape and more antero-superior hyoid bone position. The greater impact is in RP, RG and minimum AR location. Schendel et al.25 report significant data of V increases of x2.5 overall, x3.5 in RP and x1.5 in RG; and more elliptical architecture. UA shortening and hyoid bone elevation are not significant.
Some authors do an attempt to correlate and quantify the amount of planned advancement in direct relation with the L, V, AR and D changes19,21,23. Although it could be of great interest, it was not considered in our series. Many individual anatomical particularities are involved and each patient's planning is unique. Furthermore, the real bone movements rarely are exactly the planned ones, even with customized systems and especially in the mandible. We think a greater number of patients should be recruited to perform that kind of analysis and extra caution should be taken in its interpretation inasmuch as the morphing estimation of soft tissues in the face and UA with dental-osseous repositioning is not clearly established7,8).
Other structures rather than UA could be 3D segmented, studied and compared in OSAHS patients, such as the upper-maxilla, mandible, even soft tissues (tongue, soft palate or PST) knowing their meshes are less accurate than air or bone ones. Dynamic imaging, differentiating supine versus non-supine positioning and even wakefulness versus induced-asleep status, could provide more valuable information regarding the collapsibility. Due to the huge amount of CBCTs are performed nowadays to carry out dental and maxillofacial clinical evaluations, a specific 3D radiological measurement package beside physical examinations (BMI specially), could suggest high OSAHS risk before symptoms appear, as a complementary tool to sleepiness questionnaires17,19,22.
Although AHIs are not in normal range, all patients in our series describe in the clinical interview decreased snoring, improvement of daytime sleepiness and well-functionality at working time. Our study only compares PSG and CT in the short-term post-operative timing as a limitation. However, OSAHS is a chronic disorder and requires personalized multidisciplinary management with long-term follow-up. MMA provides quality of life with clinical features' improvement and morbidity reduction, but does not cure the syndrome. After MMA there seems to be skeletal stability over time, but it is not well established in terms of soft tissues and clinical symptoms, which tend to recur, inherent to aging1,2,19.
CONCLUSIONS
The MMA with CCW technique for the treatment of moderate-severe OSAHS patients, due to the anterior maxilla repositioning and the antero-superior mandibular projection, has a high success rate in short-term follow-up. It achieves overall AHI < 15 in 80 % and minimum SPO2 > 85 in 75 % of our series. The largest possible advancement and rotation are planned, taking into account occlusal, bone, soft tissue and cosmetic limitations. UA anatomical changes after MMA statistically significant and clinically relevant are shortening and total V increase, mainly due to the RP compartment, which is the most collapsible location. Minimum AR triples, UA shape is more elliptical and the hyoid bone moves to a more antero-superior position. The stability of these morphological and clinical changes in the long-term follow-up is yet to be determined. More patients will continue to be recruited for this study.
REFERENCES
1. Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil SP, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med. 2009;5(3):263-76. [ Links ]
2. Lloberes P, Durán-Cantolla J, Martínez-García MÁ, Marín JM, Ferrer A, Corral J, et al. Diagnosis and treatment of sleep apnea-hypopnea syndrome. Archivos de Bronconeumología (English Edition). 2011;47(3):143-56. DOI: 10.1016/S1579-2129(11)70034-9. [ Links ]
3. Ronchi P, Novelli G, Colombo L, Valsecchi S, Oldani A, Zucconi M, et al. Effectiveness of maxillo-mandibular advancement in obstructive sleep apnea patients with and without skeletal anomalies. Int J Oral Maxillofac Surg. 2010;39(6):541-7. DOI: 10.1016/j.ijom.2010.03.006. [ Links ]
4. Zaghi S, Holty JE, Certal V, Abdullatif J, Guilleminault C, Powell NB, et al. Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea: A Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142(1):58-66. DOI: 10.1001/jamaoto.2015.2678. [ Links ]
5. Holty JE, Guilleminault C. Maxillomandibular advancement for the treatment of obstructive sleep apnea: a systematic review and meta-analysis. Sleep Med Rev. 2010;14(5):287-97. DOI: 10.1016/j.smrv.2009.11.003. [ Links ]
6. Birbe J. Planificación clásica en cirugía ortognática. Rev Esp Cir Oral Maxilofac. 2014;36:99-107. DOI: 10.1016/j.maxilo.2012.04.007. [ Links ]
7. Brunso J, Franco M, Constantinescu T, Barbier L, Santamaría JA, Alvarez J. Custom-Machined Miniplates and Bone-Supported Guides for Orthognathic Surgery: A New Surgical Procedure. J Oral Maxillofac Surg. 2016;74(5):1061.e1-.e12. DOI: 10.1016/j.joms.2016.01.016. [ Links ]
8. Brunso J, Prol C, Franco M, Carlos FD, Martin JC, Santamaria JA. Guías y miniplacas personalizadas: un protocolo guiado para cirugía ortognática. Rev Esp Cir Oral Maxilofac. 2017;39(1):7-14. DOI: 10.1016/j.maxilo.2016.05.001. [ Links ]
9. Aboul-Hosn Centenero S. Planificación tridimensional y utilización de férulas Computer Aided Design/Computed Aided Manufacturing en cirugía ortognática. Rev Esp Cir Oral Maxilofac. 2014;36(3):108-12. 10.1016/j.maxilo.2013.02.003 [ Links ]
10. Martín Viñé L, Manchado García N, Pamiés Solé M, Bello Sebastián J, Ordax Carvajo E. Polisomnografía: procedimientos. In: Morante Vélez F, Ordax Carbajo E, editors. Manual Separ de Procedimientos 20 Manual de Procedimientos en trastornos respiratorios del sueño: Novartis Farmacéutica SA; 2010. p. 21-32. [ Links ]
11. Riley RW, Powell NB, Guilleminault C. Obstructive sleep apnea syndrome: a review of 306 consecutively treated surgical patients. Otolaryngol Head Neck Surg. 1993;108(2):117-25. DOI: 10.1177/019459989310800203. [ Links ]
12. Riley RW, Powell NB, Guilleminault C. Obstructive sleep apnea syndrome: a surgical protocol for dynamic upper airway reconstruction. J Oral Maxillofac Surg. 1993;51(7):742-7. DOI: 10.1016/s0278-2391(10)80412-4. [ Links ]
13. Aurora RN, Casey KR, Kristo D, Auerbach S, Bista SR, Chowdhuri S, et al. Practice parameters for the surgical modifications of the upper airway for obstructive sleep apnea in adults. Sleep. 2010;33(10):1408-13. DOI: 10.1093/sleep/33.10.1408. [ Links ]
14. Liu SY, Riley RW. Continuing the Original Stanford Sleep Surgery Protocol From Upper Airway Reconstruction to Upper Airway Stimulation: Our First Successful Case. J Oral Maxillofac Surg. 2017;75(7):1514-8. DOI: 10.1016/j.joms.2017.02.008. [ Links ]
15. Caples SM, Rowley JA, Prinsell JR, Pallanch JF, Elamin MB, Katz SG, et al. Surgical modifications of the upper airway for obstructive sleep apnea in adults: a systematic review and meta-analysis. Sleep. 2010;33(10):1396-407. DOI: 10.1093/sleep/33.10.1396. [ Links ]
16. Shaheen E, Shujaat S, Saeed T, Jacobs R, Politis C. Three-dimensional planning accuracy and follow-up protocol in orthognathic surgery: a validation study. Int J Oral Maxillofac Surg. 2019;48(1):71-6. DOI: 10.1016/j.ijom.2018.07.011. [ Links ]
17. Neelapu BC, Kharbanda OP, Sardana HK, Balachandran R, Sardana V, Kapoor P, et al. Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: A systematic review and meta-analysis of cephalometric studies. Sleep Med Rev. 2017;31:79-90. DOI: 10.1016/j.smrv.2016.01.007. [ Links ]
18. Larson BE. Orthodontic preparation for orthognathic surgery. Oral Maxillofac Surg Clin North Am. 2014;26(4):441-58. DOI: 10.1016/j.coms.2014.08.002. [ Links ]
19. Louro RS, Calasans-Maia JA, Mattos CT, Masterson D, Calasans-Maia MD, Maia LC. Three-dimensional changes to the upper airway after maxillomandibular advancement with counterclockwise rotation: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2018;47(5):622-9. DOI: 10.1016/j.ijom.2017.11.003. [ Links ]
20. Wei S, Zhang Y, Guo X, Yu W, Wang M, Yao K, et al. Counterclockwise maxillomandibular advancement: a choice for Chinese patients with severe obstructive sleep apnea. Sleep Breath. 2017;21(4):853-60. DOI: 10.1007/s11325-017-1484-7. [ Links ]
21. Tan SK, Leung WK, Tang ATH, Zwahlen RA. How does mandibular advancement with or without maxillary procedures affect pharyngeal airways? An overview of systematic reviews. PLoS One. 2017;12(7):e0181146. DOI: 10.1371/journal.pone.0181146. [ Links ]
22. Neelapu BC, Kharbanda OP, Sardana HK, Gupta A, Vasamsetti S, Balachandran R, et al. The reliability of different methods of manual volumetric segmentation of pharyngeal and sinonasal subregions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124(6):577-87. DOI: 10.1016/j.oooo.2017.08.020. [ Links ]
23. Faria AC, da Silva-Junior SN, Garcia LV, dos Santos AC, Fernandes MR, de Mello-Filho FV. Volumetric analysis of the pharynx in patients with obstructive sleep apnea (OSA) treated with maxillomandibular advancement (MMA). Sleep Breath. 2013;17(1):395-401. DOI: 10.1007/s11325-012-0707-1. [ Links ]
24. Zinser MJ, Zachow S, Sailer HF. Bimaxillary 'rotation advancement' procedures in patients with obstructive sleep apnea: a 3-dimensional airway analysis of morphological changes. Int J Oral Maxillofac Surg. 2013;42(5):569-78. DOI: 10.1016/j.ijom.2012.08.002. [ Links ]
25. Schendel SA, Broujerdi JA, Jacobson RL. Three-dimensional upper-airway changes with maxillomandibular advancement for obstructive sleep apnea treatment. Am J Orthod Dentofacial Orthop. 2014;146(3):385-93. DOI: 10.1016/j.ajodo.2014.01.026. [ Links ]
Received: April 11, 2020; Accepted: June 15, 2020











 texto en
texto en