INTRODUCTION
Langerhans cell histiocytosis (LCH) is a rare idiopathic disease with an incidence in the general population ranging from 1 to 4 cases per million annually1. Its presentation is more common in the pediatric population under 15 years of age, but it can occur at any age and without gender predilection2. In children, the most commonly affected bones are the skull and femur, while in adults it mainly affects the ribs, vertebrae and jaw. In the latter, it displays an incidence of 10-20 % of all cases1, highest in the mandibular body, reaching 40 % in the pediatric population3. Localization to the mandibular condyle is infrequent; only 16 cases have been reported so far in the English literature, 5 of them in children4.
We present a clinical case of mandibular histiocytosis in a 6-year-old female patient, with a rare location in the mandibular ramus and condyle. We used a novel treatment strategy, as the biopsy was performed by endoscopic access, and the treatment protocol was based on indomethacin without chemotherapy, reducing the morbidity of the latter approach.
CLINICAL CASE
A six-year-old female patient, with no history of morbidity was brought in for consultation by her mother after noticing a small increase in volume in the right preauricular area and a deviation of the mandibular midline. Physical examination revealed a painful increase in volume in the preauricular area, associated with a painless limitation of mouth opening, with ipsilateral mandibular deviation. No important pathological alterations were observed on the intraoral clinical examination.
Panoramic X-ray showed an extensive osteolytic lesion involving the head and neck of the condyle extending towards the mandibular ramus (Figure 1 A). Axial computed tomography showed signs of bone destruction in the area described above and MRI evidenced the presence of intraosseous soft tissue with diffuse limits (Figure 1 B, Figure 1 C and Figure 1 D).
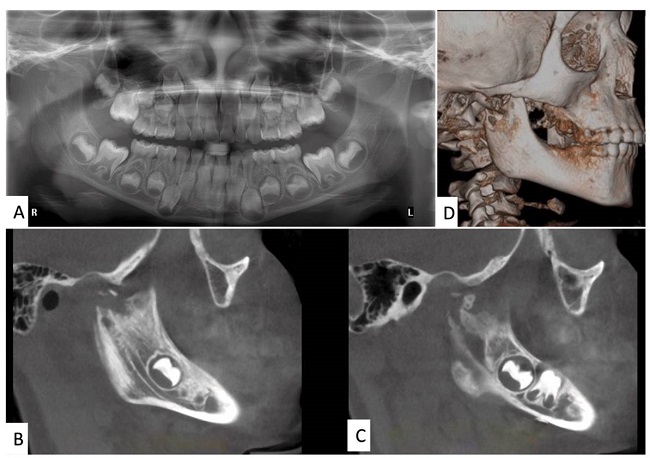
Figure 1. A: panoramic X-ray showing osteolytic process involving the neck and ramus of the right condyle. B, C: computed tomography scan: sagittal sections of the right mandibular ramus and condyle show large osteolytic process. D: three-dimensional reconstruction showing the extent of the lesion.
An incisional biopsy was indicated for the differential diagnosis between a possible mandibular osteomyelitis and a mandibular tumor. The surgical intervention included an arthrocentesis of the right TMJ, using the Nitzan technique for the cytological study and culture of the synovial fluid as part of the study for osteomyelitis and probable septic arthritis. Since the anatomical location was difficult to access, an intraoral endoscopic technique was chosen for the biopsy of the mandibular lesion, avoiding skin scars in the preauricular and retromandibular regions, and thus reducing surgical morbidity. With the patient under general anesthesia, local anesthesia was infiltrated into the retromolar trigone and the vestibular fundus of the right hemimandible, and a linear incision was made in the retromolar area, extending towards the anterior rim of the mandibular ramus, detaching its external and internal sides. An endoscope was installed on the internal side to access and visualize the surgical area, where a porous and thickened bone tissue was observed in the lower part of the lesion, with pathological appearance, and a biopsy was taken and classified as sample 1 (Figure 2).
Atypical soft tissue was observed towards the neck and condyle and an incisional biopsy was taken and classified as sample 2. For the arthrocentesis, performed under local right preauricular and right truncal auriculotemporal nerve subcutaneous anesthesia, a sample of synovial fluid was obtained and sent out for culture to rule out infectious osteomyelitis. The histopathological result of the mandibular lesion (sample 1) revealed signs of moderate to marked chronic osteomyelitis, showing lamellar and cancellous bone tissue with signs of marked remodelling, osteoid deposit and osteoblastic rim, associated with bone marrow, with an inflammatory lymphoplasmacytic component and associated fibrosis (Figure 3 A). Sample 2 from the articular and periarticular soft tissue regions exhibited bone reactive to Langerhans cells with round to ovoid morphology, nucleus with central cleft and eosinophilic cytoplasm, and multinucleated and inflammatory lymphocytic cells (Figure 3 B).

Figure 3. A: sections showing trabecular bone with reactive changes and increased cellularity in the marrow cavity (Hematoxylin and Eosin - 200x). B: diffuse proliferation of neoplastic Langerhans cells with irregular nuclei and eosinophilic cytoplasm, mixed with scattered eosinophils (Hematoxylin and Eosin - 400x). C: immunohistochemical stain for CD1a showing that the mononuclear cells in Langerhans cell histiocytosis exhibit diffuse strong staining for this antibody (400x). D: strong labelling of CD 207 (Langerin) antibody of neoplastic cells. Langerin is a very specific and sensitive marker for Langerhans cell histiocytosis (400x).
The final diagnosis was Langerhans cell histiocytosis, in accordance with immunohistochemical studies; lesion strongly positive for S100 protein, CD1a and CD207 (Langerin) (Figure 3 C, Figure 3 D). The mycobacterial molecular PCR test was negative, while cultures were positive for S. viridans and S. veillonella.
The diagnosis determined by oncological evaluation was unifocal Langerhans cell histiocytosis with special site involvement, located in the mandibular ramus and right condyle, exhibiting reactive bone with signs of microfracture and moderate to marked chronic osteomyelitis. Systemic involvement and/or presence of other foci was ruled out through body resonance imaging. The extent of the lesion, the age of the patient and the affected site were considered when deciding on the treatment. According to the clinical guidelines of the International Histiocyte Society, the first-line treatment in pediatric patients is chemotherapy. However, in order to minimize adverse effects, we decided to use the proven alternative of 5 mg/ml oral indomethacin for 24 months, at a dose of 4.5 ml every 12 hours. In addition, amoxicillin was indicated due to positive cultures. At the two-week control, the patient evolved without mouth-opening pain, with a slight deviation of the chin to the right and without volume increase in the area. Monthly controls were performed with orthopantomography and after 2 months of pharmacological treatment, radiographic signs of reossification of the right mandibular condyle and neck were observed (Figure 4 A). After 8 months, complete reossification of the area was observed and without deviation of the chin during mouth opening. The patient completed the treatment during the agreed time and is currently maintained under periodic controls, without observed recurrence (Figure 4 B and Figure 4 C).
DISCUSSION
Histiocytosis is a neoplastic and locally-aggressive disease. Bone lesions in the jaws affect the mandibular body3. Treatment depends on the type and extent of the disease, and includes clinical and radiographic observation, resection, intralesional corticosteroid injections, chemotherapy and radiotherapy, with the latter being indicated in persistent lesions5. On the other hand, spontaneous remission of less extensive lesions has been observed after biopsy or curettage. Chemotherapy can help in multisystemic manifestations with special site involvement or in reducing recurrences6. In addition, there is one reported case with special site involvement that used a combination of these therapies with good results7.
The present case presents the novel treatment of LCH in an uncommon location, in the mandibular ramus and condyle. In addition, the lesion presented an osteolytic radiological pattern with poorly-defined borders and cortical loss of the lesion, added to an increase in volume of the affected area, making it necessary to perform a differential diagnosis with entities such as osteomyelitis, lymphoma, Ewing's sarcoma and malignant metastases from a distant organs4. For the diagnosis, considering the age of the patient, the choice of the oral endoscopic approach for biopsy collection considerably reduced the morbidity compared to an extraoral approach, such as transient or permanent facial nerve damage, salivary fistula, in addition to the advantage of not leaving visible scars and promoting faster functional recovery. Moreover, the endoscope provided a superior visualization of the area, allowing for the collection of an optimal and more representative sample8. Treatment of this case with curettage and intralesional injections was ruled out because of the location and extent of the lesion9. The protocol suggested by the International Histiocytosis Society for this type of LCH is chemotherapy, recommending prednisone and vinblastine9. However, recurrence has been described in a significant percentage and is associated with adverse effects, including neutropenia, autonomic neuropathy, hypoacusis and glaucoma, in addition to the emotional burden associated with this type of treatment10. We decided to use indomethacin, a non-steroidal anti-inflammatory drug, which was administered systemically for 24 months based on its proven effectiveness in children, both in the initial treatment and in the reactivations of unisystemic LCH11. It has been shown that Langerhans cells purified from LCH bone lesions produce interleukin 1 (IL-1), thromboxane and prostaglandins 2 (PGE 2) and D2; therefore, the use of indomethacin is supported by the inhibition of the production of prostaglandins, which plays an important role in the development of LCH12. In view of the above, indomethacin was preferred due to the age of the patient, pharmacological safety, the extent and the location of the lesion, and special site involvement. This protocol proved to be successful in the present case, since we observed a recovery 2 months after starting treatment and a relapse-free evolution at the end of the pharmacological protocol.
CONCLUSION
LCH is a disease that can appear with bone lesions in different areas of the jaw, especially in the mandibular body. This article highlights the use of an intraoral endoscopic technique that allowed good access to difficult sites and reduced morbidity. In addition, the study presents a novel systemic therapy with indomethacin, which reduces toxic effects. In this case, a good result was achieved, and a remission and reossification of the compromised area were observed, with no current recurrences.
















