My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Neurocirugía
Print version ISSN 1130-1473
Neurocirugía vol.16 n.1 Feb. 2005
Hemangioblastoma of the lateral ventricle: case report and review of the literature
R. Prieto and J.M. Roda
Unit of Neurosurgery. Clínica Moncloa. Madrid.
Summary
We report a unique case of hemangioblastoma of the lateral ventricle in a 73 year-old man with cognitive deficits and fluent dysphasia. He harboured an intraventricular tumor, placed at the trigone of the left lateral ventricle. The tumor was successfully excised, by means of a temporal craniotomy. The patient became mute in the immediate postoperative with restoration of speech within a few days. The literature has been reviewed and only three other similar cases have been reported. Discovery of lesions in such unusual location should raise a high degree of suspicion for von Hippel- Lindau disease.
KEY WORDS: Hemangioblastoma. Lateral ventricle. Von Hippel-Lindau disease. Mutism.
Hemangioblastoma del ventrículo lateral: caso clínico y revisión de la literatura
Resumen
En este trabajo describimos el caso de un paciente de 73 años con déficits cognitivos y disfasia sensitiva y que fue diagnosticado mediante tomografía computarizada y resonancia magnética cerebral de una lesión tumoral situada en la encrucijada ventricular izquierda. La lesión se abordó quirúrgicamente a través de una craneotomía temporal, realizándose una extirpación total. El estudio anatomopatológico confirmó el diagnóstico de un hemangioblastoma. Durante la evolución postquirúrgica el paciente presentó un cuadro de mutismo transitorio. Una revisión exhaustiva de la literatura ha evidenciado la existencia de tan sólo tres casos similares descritos previamente. El diagnóstico de este tipo de lesiones en una localización tan infrecuente debería hacernos sospechar la enfermedad de von Hippel-Lindau.
PALABRAS CLAVE: Hemangioblastoma. Ventrículo lateral. Enfermedad de von Hippel-Lindau. Mutismo.
Recibido: 20-02-04 Aceptado: 28-02-04
Abreviaturas. VHL: Hippel-Lindau disease.
Introduction
Hemangioblastomas of the central nervous system (CNS) are the most frequent vascular tumors19,22. They are histologically benign tumors representing 1-2% of all intracranial neoplasms5,14,24 but when posterior fossa tumors are considered alone, the percentage rises to 7.315. Although they are usually isolated tumors, sometimes they can be associated with von Hippel-Lindau (VHL) disease in 3 to 38% as a major manifestation3,14. This inherited phakomatosis is clinically characterized by the formation of vascular tumors, including retinal and CNS hemangioblastomas. Other features include cyst of the kidneys, liver and pancreas, clear renal cell carcinomas, pheocromocytomas and endolymphatic sac tumors. It is thought to be a dysembryogenic defect of the mesenchyme occurring in about the third month of fetal life and affecting various developing organs in the body simultaneously. In 1993, the VHL gene was localized on the shorter arm of chromosome 3 (3p25- 26)10.
Although hemangiobastomas are predominantly found in the cerebellum, spinal cord and brainstem3,24, some unusual locations have been reported16,18. Supratentorial location account for 4% to 13%3. However, hemangioblastomas of the lateral ventricle are very rare indeed. The first described case was an incidental finding during a postmorten examination21. Afterwards only three symptomatic cases have been published6,9,12.
Case Report
This 73 year-old-man presented with a few days history of cognitive deficits and confusion without any other complain. Neurological examination disclosed a Glasgow Coma Scale of 14 (E, 4; V, 4 and M, 6) and fluent dysphasia. He had a history of a previous surgical procedure for the removal of a renal cell carcinoma ten years ago. Laboratory investigations revealed a hemoglobin of 15.5 g/dL and a hematocrit of 46.2%. None of his relatives had had any relevant illness or any lesion of the VHL disease.
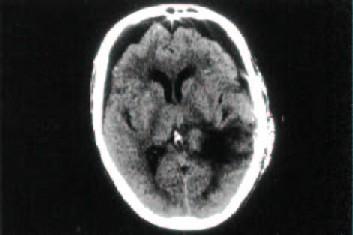
Computed Tomographic (CT) scan showed an intraventricular tumor placed at the trigone of the left lateral ventricle with dilatation of the ipsilateral trigone and temporal horn. It enhanced markedly with contrast medium (Fig. l). The posterior fossa was normal.
 | 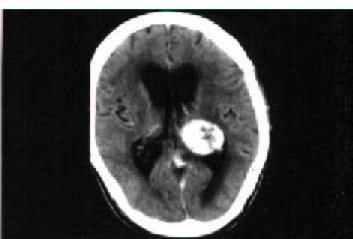 |
Fig. 1. Preoperative computed tomography scan. Left: Plain scan showing and intraventricular tumor situated at the trigone of the left
lateral ventricle with dilatation of the ipsilateral trigone and temporal horn; Right: Enhanced sean showing a homogeneous contrast
enhancement.
On Magnetic Resonance Imaging (MRI) the tumor had a heterogeneous signal. lt was hypo-isointense on T1-weighted images compared with the normal white matter and hypo-isointense on T2 weighted images with central hypointense areas. Long Repetition Time (TR) sequences showed periventricular edema. Gadolinium-enhanced T1-weighted MRI demonstrated a solitary, solid, rounded intraventricular tumor, 3 cm in diameter, placed at the trigone of the left lateral ventricle (Fig. 2). The approximated volume of the lesion was 13.5 cm3 which was calculated by a modified ellipsoid formula (length x width x height x 0.5).
 |  |
Fig. 2. Preoperative magnetic resonance imaging. Left: T1-weighted sagittal section after gadolinium-DTPA infusion showing a
solitary, solid, rounded and well-enhanced intraventricular mass 3 cm in diameter. Right: T2-weighted showing a hypo-isointense
mass compared with the normal white matter with central hypointense areas.
Magnetic resonance angiography demonstrated a large vascular tumor fed by branches of the P2 segment of the posterior cerebral artery (Fig.3).
Fig. 3. Magnetic resonance angiography demonstrating a vascular
tumor fed by branches of P2 segment (posterolateral choroidal arteries).
On June 2003, the patient underwent a left temporal craniotomy. Intraoperative ultrasonography was performed to confirm the precise location of the tumor. A 3 cm horizontal corticotomy was made over the middle temporal gyrus. This gave direct access to the left temporal horn. The choroids plexus was covering a reddish vascular tumor. The lesion was foamy and had an important vascularity. With careful dissection under the microscope, blood supply coming from the posterior choroidal vessels and the ependyma was interrupted. A large vein draining to the deep venous system was coagulated. It was relatively well demarcated except the anterior area, where the limits were somewhat imprecise. The whole tumor was then removed.
The patient became mute in the immediate postoperative period and control CT showed a large frontal pneumo-encephalus and the complete removal of the tumor (Fig.4). Twelve days after the operation, the speech returned but a mixed dysphasia was present. He improved in terms of cognitive disturbances but presented gait ataxia. Serial CTs demonstrated progressive disappearance of pneumoencephalus.
Fig.4. Early postoperative computed tomography scan, demonstrating
complete tumor removal and large pneumoencephalus.
Histopathological examination showed a tissue composed of a fine network of blood spaces separated by numerous polygonal stromal cells, with lighty stained cytoplasm. Immunohistochemical staining showed a strong immunopositivity in several stromal cells for vimentin and EMA (Epithelial Membrane Antigen). The intercapillary component was immunopositive for endothelial cell markers CD31 and CD34. In addition, immunohistochemical expresion of a cell cycle related antigen (MIB-1) showed a low proliferative kinetic. It was typical of a bening hemangioblastoma.
Following the protocol of the National Institutes of Health Screening we performed an additional evaluation. It included ophthalmologic examination, CT scanning of the abdomen and 24-hour urinary analysis for vanillymandelic acid, metanephrines, and total catecholamines. The result of the entire screening workup was negative.
Discussion
Hemangioblastomas of the CNS are infrequent and they account for approximately 2% of primary CNS tumors14,19,24. The most frequently affected site is the posterior fossa with the cerebellar hemispheres as the most common location (83%), followed by the spinal cord and brainstem14. Supratentorial hemangioblastomas are rare, they account for 4% in patients with sporadic disease and 13% in VHL disease3.The intraventricular location is very unusual and only three symptomatic lesions6,9,12 and an incidental postmorten finding21 have been described to date (Table l).
According to Melmon and Rosen's criterial1, the patient's case can be classified as VHL disease, because he was previously operated of a renal cell carcinoma. lnterestingly, all lateral ventricle hemangioblastomas have been seen in patients with VHL. So a high degree of suspicion for VHL disease should be raised in patients with hemangioblastomas in that location. In addition spinal hemangioblastomas, multiple lesions3 and leptomeningeal hemangioblastomatosis16 are diagnostic of this condition. Within these non-invasive tumors, symptom production depends on lesion size and location. It has been reported that at the time of surgery cerebellar hemangioblastomas (mean tumor volume 3.4+6.8 cm3) were much larger than those lesions in the brainstem (0.7±0.5 cm3) or spinal cord (0.8+1.8 c m3)23. All the lesions reported to be lying in the lateral ventricle had a greater volume, between 13.5 and 62.5 cm3. lt is likely that lesions in the lateral ventricle need major volume to produce symptoms, because there is much space available to accommodate a mass effect in this anatomical compartment. Cysts have been frequently associated with tumor size either in cerebellum, brainstem or spinal cord, but it is noteworthy that the lateral ventricle lesions were solid, in spite of their large volume.
Mutism, developed by our patient in the postoperative period, is a state in which the subject is conscious but unable to speak4. Postoperative mutism is an infrequent and usually transient complication of surgery. It is most commonly seen following extensive callosotomy, ventrolateral thalamotomy (especially when performed bilaterally) and resection of supplementary motor area or posterior fossa lesion4,7,17. These areas are connected via dentatothalamocortical pathways and it appears that bilateral disruption of the elements of this pathway may be responsible for this phenomenon4. lt is also in relation to damage to the limbic system, caused by lesions in the septum pellucidum or both fornices1,13. Single photon emission tomography studies reported that patients with postoperative cerebellar mutism disclosed a marked reduction of cerebral perfusion in the fronto-parietal region8,20. We reviewed the literature looking for reports on patients with temporal transcortical surgery for tumors at the trigone of the lateral ventricle and postoperative mutism and did not find any report to elucidate our disappointing fact. The closeness between the tumor and the posterolateral region of the thalamus and the crura of fornix and/or the edema or ischemia in the fronto-temporoparietal region, caused by surgical manoeuvres, could have been the main causes triggering this speech disturbance.
Conclusion
Hemangioblastomas of the lateral ventricle are exceptional tumors and their discovery should raise a high degree of suspicion for VHL disease.
References
1. Asgan, S., Engenhorn, T., Brondics, A., Sandalcioglu, I.B., Stolke, D.: Transcortical or transcallosal approach to ventricle- associated lesions: a clinical study on the prognostic role of surgical approach. Neurosurg Rev, 2003; 26:192-197. [ Links ]
2. Choyke, P., Glenn, G., Walther, M., et al.: Von Hippel- Lindau disease: Genetic, clinical, and imaging features. Radiology 1995; 194: 629-642. [ Links ]
3. Conway, J., Chou, D., Clatterbuck, R., Brem, H., Long, D.M., Rigamonti, D.: Hemangioblastomas of the Central Nervous System in von Hippel-Linday Syndrome and Sporadic Disease. Neurosurgery 2001; 48: 55-63. [ Links ]
4. Crutchfield, J., Sawaya, R., Meyers, C., Moore, B.D. 3rd: Postoperative mutism in neurosurgery. J Neurosurg 1994; 81: 115-121. [ Links ]
5. Cushing, H., Bayley, B.: Tumours arising from the blood vessels of the brain. Angiomatous malformations and hemangioblastomas, ed Springfield IL: Charles C: Thomas. 1928. [ Links ]
6. Diehl, P., Symon, L.: Supratentorial Intraventricular Hemangioblastoma: Case Report and Review of Literature. Surg Neurol 1981; 15: 435-443. [ Links ]
7. Gelabert-Gonzalez, M., Fernander-Villa, J.: Mutism after posterior fossa surgery. Review of the literature. Clin Neurol Neurosurg 2001; 103: 111-114. [ Links ]
8. Germano, A., Baldari, S., Caruso, G., et al.: Reversible cerebral perfusion alterations in children with transient mutism after posterior fossa surgery. Neuropediatrics 1998; 23: 144-146. [ Links ]
9. Ho, Y-S., Plets, C., Goffin, J., Dom, R.: Hemangio-blastoma of the Lateral Ventricle. Surg Neurol 1990; 33: 407-412. [ Links ]
10. Latif F, Tory K, Gnarra J, et al: ldentification of the von Hippel-Lindau disease tumor suppressor gene. Science 1993; 260: 1317-1320. [ Links ]
11. Melmon K, Rosen S: Lindau"s disease. Review of the literature and study of a large kindred. Am J Med 1964; 36: 595-617. [ Links ]
12. Murakami H, Toya S, Otani M, Sato S, Ohiera T, Takenaka N: A case of concomitant posterior fossa and supratentorial hemangioblastomas. No Shinkei Geka 1985 (abstract); 13: 175-179. [ Links ]
13. Nakasu Y, Isozumi T, Nioka H, Handa J: Mechanism of mutism following the transcallosal approach to the ventricles. Acta Neurochir (Wien) 1991; 110: 146-153. [ Links ]
14. Neumann H, Eggert H, Weigel K, Friedburg H, Wiestler OD, Schollmeyer P: Hemangioblastomas of the central neorvous system. J Neurosurg 1989; 70: 24-30. [ Links ]
15. Olivecrona H: Cerebellar angioreticulomas. J Neurosurg 1952; 9: 317. [ Links ]
16. Reyns N, Assaker R, Louis E, Lejeune JP: Leptomeningeal Hemangioblastomatosis in a Case of von Hippel- Lindau Disease: Case Report. Neurosurgery 2003; 52: 1216. [ Links ]
17. Sagiuchi T, Ishii K, Aoki Y, et al: Bilateral crossed cerebellocerebral diaschisis and mutism after surgery for cerebellar medulloblastoma. Ann Nucl Med 2001; 15: 157-160. [ Links ]
18. Sajadi A, Tribolet N: Unusual locations of hemangioblastomas. J Neurosurg 2002; 97: 727. [ Links ]
19. Strugar J, Criscuolo G: Primary intracranial vascular tumors, in Vecht C (ed): Handbook of Clinical Neurology. Neuro-Oncology, 1997; Part II, pp 69-286. [ Links ]
20. Van Mourik M, Catsman-Berrevoets C, Van Dongen H, Neville BGR: Complex orofacial movements and the disappearance of cerebellar mutism: report of five cases. Dev Med Child Neurol 1997; 39: 686-690. [ Links ]
21. Vecchi B, Patrassi G: Angioretriculoma del plessi corioidei, con "aree di Gamna". Schweiz Med Wochenschr 1935; 65: 242-246. [ Links ]
22. Vega-Basulto S, Silva-Adán S, Peñones-Montero R, Mosqueda-Betancourt G: Hemangioblastomas of the Central Nervous System in Camagüey (Cuba). Rev Neurol 2002; 35: 512-516. [ Links ]
23. Wanebo JE, Lonser RR, Glens GM, Oldfield EH: The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg 2003; 98: 82-94. [ Links ]
24. Weil R, Vortmeyer A, Zhuang Z, et al: Clinical and molecular analysis of disseminated hemangioblastomatosis of the central nervous system in patients without von Hippel- Lindau disease. J Neurosurg 2002; 96: 775-787. [ Links ]
Prieto, R.; Roda, J.M.: Hemangioblastoma of the lateral ventricle: case report and review of the literature. Neurocirugía 2005; 16: 58-62.
Corresponding author: Ruth Prieto. Hospital Universitario La Paz. Castellana, 261, 28046 Madrid.