The Prevalent Tendencies for Mental Disorders in Pakistan
Mental health problems are globally recognized as a major social issue which needs to be addressed aggressively. Although 30% to 50% of the world population is expected to be suffering from some form of mental illness (Mackenzie, Gekoski, & Knox, 2006), studies have reported different figures for the prevalence of mental disorders in different countries, e.g., 10.1% in Canada, 18.5% in the United States, and 38.2% in Europe (Lesage et al., 2006; Pearson, Janz, & Ali, 2013; Wang et al., 2007; Wittchen et al., 2011). The prevalence of mental disorders has also been significantly found in Muslim countries. One fifth of primary-care attendees in Saudi Arabia (Al-Khathami & Ogbeide, 2002; Almutairi, 2015), more than half of the general patients in the United Arab Emirates (Abou-Saleh, Ghubash, & Dardkeh, 2001; Dardkeh, Eapen, & Ghubash, 2005; El-Rufaie & Absood, 1993), and 17% general population in Egypt (Ghanem, Gadallah, Meky, Mourad, & El-Kholy, 2009) were found to have some sort of mental disorders. Studies related to India (Khandelwal, Jhingan, Ramesh, Gupta, & Srivastava, 2004; Math, Chandrashekar, & Bhugra, 2007; Weiss, Isaac, Parkar, Chowdhury, & Raguram, 2001) revealed that at least 10 million Indians suffer from severe mental illness. Mirza and Jenkins (2004) referred to 20 studies conducted in Pakistan and stated that the prevalence of depression in Pakistan was 33%, with women having a higher prevalence than men. Other academic studies conducted in the country have also been focusing on a few typical mental disorders, e.g., depression and anxiety, and were mostly not focused on the general population. The researcher did not find any earlier study which would have focused on the prevalence of a variety of mental disorders in the general population. It was, therefore, considered the need of the time to explore it to analyze the latest situation of the prevailing mental disorders in the country. Although the current study did not intend to label the respondents as mentally ill as it would have required deeper clinical investigation, findings would help understand the tendencies of Pakistanis towards different mental disorders.
Method
Participants
The study involved 3,500 conveniently selected Pakistanis from different major cities, such as Islamabad, Rawalpindi, Peshawar, Abbottabad, and Lahore. They included both males (n = 1,621) and females (n = 1,879). Excluding minors, participants of the study belonged to all age groups, i.e., adolescents aged 13 to 19 years (n = 266), young adults aged 20 to 29 years (n = 1,446), adults aged 30 to 59 years (n = 1,702), and elderly aged 60 years and above (n = 86). They included both single (n = 1,696) and married (n = 1,804) people. Their educational qualifications varied as Primary (n = 19), Middle (n = 55), Secondary (n = 184), High School (n = 479), Graduation (n = 1,318), Masters (n = 916), MPhil (n = 397), and PhD (n = 109). The study also included illiterate participants (n = 23). The participants belonged to different professions, i.e., teachers (n = 578), housewives (n = 481), businessmen (n = 262), students (n = 1,128), engineers (n = 118), soldiers (n = 65), lawyers (n = 27), medical doctors (n = 141), bankers (n = 10), laborers (n = 59), managers (n = 180), government servants (n = 206), nurses (n = 6), journalists (n = 1,879), policemen (n = 14), and psychological counselors (n = 5). The study also included jobless participants (n = 40). Based on their economic status, participants were divided into four categories, i.e., poor, whose monthly income was lower than Rs. 30,000 per month (n = 815), lower-middle class, whose monthly income was between Rs. 31,000 and Rs. 60,000 per month (n = 1,121), upper-middle class, whose monthly income was between Rs. 61,000 and Rs. 90,000 per month (n = 607), and well-off, whose monthly income was above Rs. 91,000 per month (n = 957).
Instrument
A detailed research questionnaire in the Urdu language was developed to gather the required data. The first part of the questionnaire consisted of the demographic information of the respondent, i.e., gender, age, profession, marital status, educational qualification, and approximate monthly income. The second part of the questionnaire consisted of a checklist to measure the tendencies for different mental disorders. This checklist was based on the symptoms of the understudied disorders in accordance with the Diagnostic and Statistical Manual of Mental Disorders IV-TR (American Psychiatric Association, 2000). The disorders measured were labeled as Depression, Anxiety, Stress, Adjustment-related problems, Sleep-related problems, Eating-related problems, Memory-related problems, Paranoid Personality Disorder, Schizoid Personality Disorder, Antisocial Personality Disorder, Borderline Personality Disorder, Histrionic Personality Disorder, Narcissistic Personality Disorder, Avoidant Personality Disorder, and Dependent Personality Disorder. It was intended not to label the respondents with certain mental disorders based on this checklist; hence the checklist was assumed to provide the possible tendencies for the understudied disorders. The entire questionnaire could take 20 to 25 minutes to be completed. Twenty-three research participants were illiterate. The same questionnaire was used as an interview schedule to obtain data from them while conducting individual interviews.
Procedure
The researcher paid frequent visits to the aforesaid cities and approached the conveniently selected participants in different educational institutions, governmental and non-governmental offices, private companies, etc. The respondents were briefly informed about the objective of the study and their consent was obtained. The data gathered was analyzed with the Statistical Package for Social Sciences.
Results
The current study has tried to assess tendencies for different mental disorders. Based on these findings, we cannot label the respondents with certain mental disorders; however, we can assume the possibilities of those disorders among them. According to the findings in this regard (Table 1), 38% of the respondents possessed tendencies for depression, 31% for anxiety, 32% for stress, 33% for adjustment-related disorders, 38% for sleep-related problems, 30% for eating-related problems, 36% for memory-related problems, 26% for paranoid personality disorder, 23% for schizoid personality disorder, 11% for anti-social personality disorder, 18% for borderline personality disorder, 24% for histrionic personality disorder, 17% for narcissistic personality disorder, 25% for avoidant personality disorder, and 29% for dependent personality disorder. The findings, if seen from an overall perspective on mental health, reveal that 27% of the respondents did possess tendencies for mental disorders. Depression and sleep-related problems were found to be on the top.
Gender
The analysis based on gender revealed highly significant differences between males and females in having tendencies towards mental disorders (Table 2). Females had significantly higher tendencies towards mental disorders as compared with males (M = 29% vs. 26%, p = .000). Probing further, females were found to have significantly higher tendencies for depression (M = 43% vs. 31%, p = .000), anxiety (M = 33% vs. 29%, p = .003), eating-related problems (M = 32% vs. 28%, p = .014), paranoid personality disorder (M = 29% vs. 23%, p = .000), avoidant personality disorder (M = 28% vs. 23%, p = .001), and dependent personality disorder (M = 33% vs. 25%, p = .000). Males, on the other hand, had significantly higher tendencies of borderline personality disorder (M = 22% vs. 17%, p = .013) and narcissistic personality disorder (M = 19% vs. 16%, p = .016) as compared to females.
Table 2 The Prevalent Tendencies for Different Mental Disorders: A Categorical View by Percentages
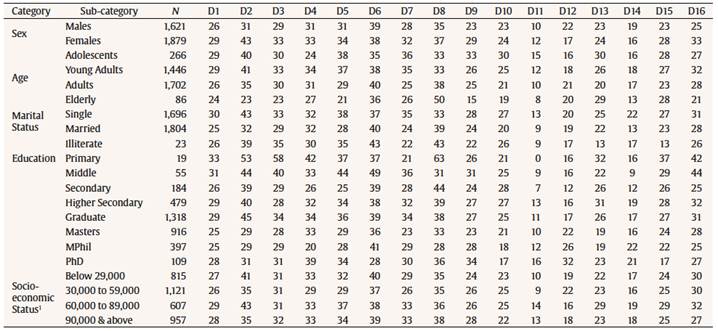
Note. N = total respondents; D1 = Overall Tendencies; D2 = Depression; D3 = Anxiety; D4 = Stress; D5 = Adjustment; D6 = Sleep; D7 = Eating; D8 = Memory; D9 = Paranoid
Personality Disorder; D10 = Schizoid Personality Disorder; D11 = Antisocial Personality Disorder; D12 = Borderline Personality Disorder; D13 = Histrionic Personality Disorder;
D14 = Narcissistic Personality Disorder; D15 = Avoidant Personality Disorder; D16 = Dependent Personality Disorder.
1Monthly income in Pakistani Rupees.
Marital Status
Unmarried participants were found to have significantly higher tendencies towards mental disorders (Table 2) as compared to married (M = 30% vs. 25%, p = .000). Unmarried had significantly higher tendencies for depression (M = 43% vs. 32%, p = .000), anxiety (M = 33% vs. 29%, p = .008), adjusted-related problems (M = 38% vs. 28%, p = .000), eating-related problems (M = 35% vs. 24%, p = .000), paranoid personality disorder (M = 28% vs. 24%, p = .004), schizoid personality disorder (M = 27% vs. 20%, p = .000), antisocial personality disorder (M = 13% vs. 9%, p = .000), histrionic personality disorder (M = 25% vs. 22%, p = .020), narcissistic personality disorder (M = 22% vs. 13%, p = .000) and avoidant personality disorder (M = 27% vs. 23%, p = .007). Married participants, on the other hand, had significantly higher tendencies towards memory-related problems (M = 39% vs. 33%, p = .000).
Age
Adolescents (13 to 19 years of age) and young adults (20 to 29 years of age) had significantly higher tendencies towards mental disorders (M = 29%, p = .001) (Table 2) as compared with adults (30 to 59 years of age) and elderly (60 years of age or above). Further analyses of variance revealed that adolescents had significantly higher tendencies towards adjustment-related problems (M = 38%, p = .000), eating-related problems (M = 36%, p = .000), paranoid personality disorder (M = 33%, p = .004), schizoid personality disorder (M = 30%, p = .004), antisocial personality disorder (M = 15%, p = .007), histrionic personality disorder (M = 30%, p = .000) and avoidant personality disorder (M = 28%, p = .059). Young adults had significantly higher tendencies towards depression (M = 41%, p = .000), stress (M = 34%, p = .016) and dependent personality disorder (M = 32%, p = .010). Adults had not projected any significantly higher variance towards any of the understudied mental disorders. Elderly had significantly higher tendencies towards memory-related problems (M = 50%, p = .001).
Education
People having primary level education had significantly higher tendencies towards mental disorders (Table 2) as compared with their counterparts (M = 33%, p = .000). Further analyses of variance revealed that people with primary levels of education (till grade 5) had significantly higher tendencies towards depression (M = 53%, p = .000), anxiety (M = 58%, p = .009), stress (M = 42%, p = .000), memory-related problems (M = 63%, p = .000) and histrionic personality disorder (M = 32%, p = .000). People with middle levels of education (till grade 8) had significantly higher tendencies towards adjustment-related problems (M = 44%, p = .001), eating-related problems (M = 36%, p = .000) and dependent personality disorder (M = 44%, p = .031). People with secondary level of education (till grade 10) had significantly higher tendencies towards schizoid personality disorder (M = 28%, p = .012). People with MPhil had significantly higher tendencies towards narcissistic personality disorder (M = 22%, p = .039). People with PhD had significantly higher tendencies towards borderline personality disorder (M = 32%, p = .001). Illiterates, people with higher secondary education (grades 11 & 12), people with graduation and people with master level qualification did not showed any significantly higher variance towards any of the understudied mental disorders.
Income
The upper-middle class had significantly higher tendencies towards mental disorders (M = 29%, p = .054) compared to the poor, lower-middle or well-off class (Table 2). This class specifically had significantly higher tendencies towards depression (M = 43%, p = .000), adjusted-related problems (M = 37%, p = .009), eating-related problems (M = 33%, p = .002), anti-social personality disorder (M = 14%, p = .001) and histrionic personality disorder (M = 19%, p = .016) as compared with its counterparts. The poor class, at one instance only, showed significantly higher tendencies towards borderline personality disorder (M = 19%, p = .054) compared with rest of the classes.
Discussion
Earlier studies in different parts of the world have also found women having more mental disorders than men (e.g., Kessler, McGonagle, Swartz, Blazer, & Nelson, 1993; Seedat et al., 2009). Certain studies also attempted to distinguish this difference for specific mental disorders separately and found that women were twice more likely to have anxiety and mood-related disorders as compared to men (e.g., Angst et al., 2002; de Graaf, ten Have, van Gool, & van Dorsselaer, 2012; Kessler et al., 1994); men were four times more likely to develop substance abuse and impulsive disorders as compared to women (e.g., Offord et al.,1996; Seedat et al., 2009); and women had higher levels of borderline personality disorder as compared to men (American Psychiatric Association, 2000).
The impact of marital life on mental health has been studied widely. The emotional security and social stability associated with marital life helps improve one’s mental health. Consequently, widows, separated, and divorced showed higher rates of mental disorders as compared to the married (e.g., Gove, 1972; Gove & Tudor, 1973; Kiecolt-Glaser & Newton, 2001; Wu & DeMaris, 1996).
Studies in the lifespan psychopathology have also suggested that the prevalence of mental disorders is more common in young adults as compared with the elderly (Donnellan & Lucas, 2008; Gum, King-Kallimanis, & Kohn, 2009; Hasin, Goodwin, Stinson, & Grant, 2005; Hoertel et al., 2013; Jorm, 2000; Kessler et al., 2005; Manetti et al., 2014; Schuster, Hoertel, Le Strat, Manetti, & Limosin, 2013; Seitz, Purandare, & Conn, 2010; Sunderland, Anderson, Sachdev, Titov, & Andrews, 2015; Weissman et al., 1985).
Higher educational qualifications have always been positively associated with enhanced mental health. Lower-educated people generally report more tendencies towards mental disorders (Dohrenwend & Schwartz, 1995; Mirowsky & Rose, 1998, 2003, 2005).
Earlier studies have suggested that mental disorders are more associated with the ones who belong to lower economic status and poverty has also been positively associated with poor mental health (e.g., Adler, Epel, Castellazzo, & Ickovics, 2000; Collins & Goldman, 2008; McLeod & Shanahan, 1993; Rutter, 2003; Singh-Manoux, Adler, & Marmot, 2003; Singh-Manoux, Marmot, & Adler, 2005). The findings of the current study did not support the association of poverty and poor mental health, but the people belonging to the upper-middle range by their income were found more inclined towards mental disorders. The role of religiosity could have been one of the mediating factors here and could be further studied in future.















