Introduction
Anxiety and depression symptoms and disorders are among the leading causes of associated disability and burden of disease worldwide among young people (Whiteford et al., 2013; World Health Organization [WHO, 2021]). The worldwide prevalence of mental disorders in children and adolescents has been reported at 13.4%, anxiety disorder at 6.5%, and depressive disorder at 2.6% (Polanczyk et al., 2015). In Spanish adolescents, the estimated prevalence for all anxiety disorders is 11.8% (Canals et al., 2019), while for all depressive disorders it is 3.4% (rate of depressive symptoms 11.6%) (Canals-Sans et al., 2018). Anxiety and depression are comorbid conditions both at a clinical and subclinical level. Adolescents who report anxiety problems also have a higher risk of presenting mood problems and vice versa (Balázs et al., 2013; Canals et al., 2019). In addition, the first mental disorder occurs before the age of 14 in a third of cases and before the age of 18 in almost half (48.4%) (Solmi et al., 2021). The peak/median age of onset across all mental disorders is 14.5 years old (Solmi et al., 2022). Moreover, experiencing mental health problems before 14 years of age has been associated with an elevated risk for adult mental disorders (Mulraney et al., 2021).
The consequences of poor psychological adjustment have repercussions in other spheres of young people's lives (i.e., personal, family, school, social, economic, health care) in the short, medium, and long term (Erskine et al., 2015; Marrero et al., 2020). In education, good health is linked to reduced drop-out rates and better educational attainment and performance (WHO, 2021). Economically, the annual human capital loss from mental health conditions in children aged 0-19 is $387.2 billion, of which $340.2 billion are related to anxiety and depressive disorders (UNICEF, 2021). For instance, a recent meta-analysis showed that depression was associated with higher direct costs in adolescents (König et al., 2020). In addition, global prevalence and the burden of depressive and anxiety disorders increased in 2020 due to the COVID-19 pandemic (Amorós-Reche et al., 2022; Santomauro et al., 2021). Given all of that, and the sustainable development goals (SDGs) for mental health (Patel et al., 2018), this emerging social challenge needs to be addressed through prevention strategies in significant developmental stages, such as adolescence.
Schools are at the forefront of promoting mental health, as well as prevention and early interventions during childhood and adolescence. They are the “natural” place for actions to promote mental well-being and, specifically, to prevent mental health problems. Most adolescents spend long periods of time in classrooms, with schools being one of the main agents involved in socialization, as well as in training and promoting optimal development. In this regard, the WHO Guidelines on School Health Services (WHO, 2021) highlight that schools are essential environments for acquisition of socio-emotional skills (e.g., self-regulation and resilience). In the last decade, a range of psychological interventions have been tested for promoting mental health and preventing mental health problems in schools with varying degrees of success (Feiss et al., 2019; González-Roz et al., 2023; Werner-Seidler et al., 2017). Previous research suggests that universal prevention programs for depression had smaller effect sizes post-test than targeted programs, but effect sizes for anxiety were similar for universal and targeted programs (Werner-Seidler et al., 2017). Overall, school-based mental health services demonstrated a small-to-medium effect (Hedges g = 0.39) in reducing mental health problems, with the largest effects found for targeted intervention (Hedges g = 0.76), followed by selective prevention (Hedges g = 0.67), compared with universal prevention (Hedges g = 0.29) (Sánchez et al., 2018). However, there is still a need for a stronger, broader evidence base in the field of mental health promotion and prevention in school settings (O'Connor et al., 2018; O'Reilly et al., 2018).
In recent decades, increasing efforts have been made to prevent mental health problems in adolescent populations, with the development of a plethora of interventions (Fonseca-Pedrero et al., 2021; Weisz & Kazdin, 2017). Research in the field has recently shown interest in understanding it from a transdiagnostic perspective, exploring variables that can account for the onset, progression, and maintenance of different emotional disorders and other co-occurring conditions. Various transdiagnostic psychological interventions have been designed and tested for treatment and prevention, and there have been encouraging findings regarding efficacy, efficiency, and effectiveness (Dalgleish et al., 2020; Fusar-Poli et al., 2019). Within this transdiagnostic approach, Barlow and colleagues developed the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP) for adults (Barlow et al., 2011; Barlow et al., 2017), adolescents (UP-A), and children (UP-C) (Ehrenreich-May et al., 2018). The UP was designed to be a flexible, evidence-based intervention that could treat a wide range of emotional disorders and other mental health conditions with strong emotional components. Previous systematic reviews also indicate that these adaptations usually achieved their intended outcomes; however, further research is needed (Cassiello-Robbins et al., 2020).
The UP-A is an emotion-focused, transdiagnostic cognitive behavioral therapy (CBT) for adolescents (aged 12-17) with a principal diagnosis of any anxiety disorder, any depressive disorder, or any combination of the two (Ehrenreich-May et al., 2018). The UP-A is a downward extension of the UP for adults. It is divided into five main treatment modules (Emotion education, Emotional awareness; Generalized emotion exposures, Nonjudgmental awareness; Cognitive reappraisal, Problem solving; Interoceptive and in vivo exposures, Behavioral activation; Skill consolidation and Relapse prevention) and three optional modules. It is designed to be delivered within 8-21 weekly sessions. Recent studies have shown it to be effective for reducing symptoms of anxiety and depression and functional impairment in adolescents with emotional disorders (Ehrenreich-May et al., 2017). In addition, a significant treatment effect in favor of UP-A was observed for all outcome measures at posttreatment (Bilek & Ehrenreich-May, 2012; Ehrenreich-May et al., 2017; Grossman & Ehrenreich-May, 2019; Kennedy et al., 2019; Weintraub et al., 2020). The UP-A has been adapted to Spanish as a School-Based Anxiety and Depression Prevention Program delivered in a school setting (García-Escalera et al., 2017; García-Escalera et al., 2020). Preliminary results showed that overall differences between conditions did not reach statistical significance. However, subgroup analyses showed a greater decrease of symptoms in the UP-A. Along these lines, and according to García-Escalera et al. (2019), the UP-A is an interesting protocol for application in prevention, since it has a manual, it can be flexibly administered, and it is relatively easy to apply. It also addresses the main risk and maintenance factors of emotional problems. The UP-A shows promise adapted to other formats (e.g., online) and goals (e.g., indicated prevention).
Studies have provided preliminary evidence of the effectiveness of the UP-A in the treatment of anxiety and depression symptoms in adolescents. However, to date there have been few randomized controlled trials (RCT). In addition, the UP-A has not yet been applied in Spain to a large sample of adolescents with emotional problems (indicated prevention) in school settings, nor have medium- or long-term follow-ups (e.g., 12 and 18 months) been carried out to verify the efficacy of the UP-A. In this context, the main goal of the present study is to evaluate the effectiveness of the UP-A in adolescents with moderate emotional symptoms in educational settings. The main goals of the PSICE project are: a) to reduce symptoms of anxiety and depression, b) to prevent clinically elevated levels of anxiety and depression, and c) to improve adolescents' socioemotional adjustment, learning processes, and academic achievement.
Method
The study has been approved by the CEImLAR (Clinical Research Ethics Committee of La Rioja, number PI 552). Following gold standards in research on intervention effectiveness (CONSORT), the study design including the proximal and distal outcomes has been preregistered in ClinicalTrials.gov (ref: NCT05322642).
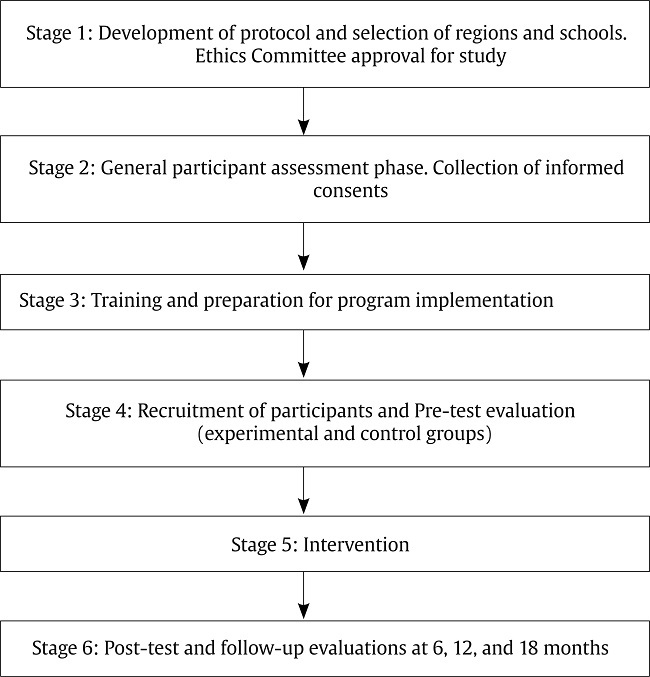
Study Design
This research uses an RCT design, with an experimental group (UP-A) and an active control group (progressive relaxation training). Participants within schools are randomly assigned to one of two study conditions. Each participant is randomly allocated 1:1 to the preventive intervention or control condition. A balanced design is used. Cluster randomization is undertaken for the ecological validity of providing the intervention at the school level. The study includes pre-test and post-test with follow-ups at 6, 12, and 18 months.
Experimental group: The UP-A is an emotion-focused, transdiagnostic CBT for adolescents. It is divided into five main treatment modules and three optional modules. The UP-A seeks to positively affect how adolescents with anxiety and/or depression experience, think about, and respond to a broad range of negative and positive emotions, rather than disorder-specific emotions (e.g., fear, sadness). A 10-session, youth-focused program has been designed to adapt the core modules of the UP-A for both indicated prevention and school settings.
Control group: The active control condition is based on the 10-session Progressive Relaxation Training Program (Bernstein & Borkovec, 1973). It follows a similar structure to the UP-A. Relaxation training is often used in behavior therapy to reduce anxiety, tension, and stress. The main goal is to release tension from the muscles, while helping recognize what that tension feels like. A group format is used.
Participants
In the initial screening phase, adolescents from schools in different autonomous communities (regions) in Spain will be selected. Initially, they will be selected based on a screening of the general school population, although they may come from the school's guidance services or teams. It is estimated that each region will collect a total of approximately 1,600 participants—200 students from 8 different schools. The schools must be heterogeneous in terms of geographical area (rural/urban) and type (public/subsidized).
The sample size in the treatment phase was estimated using the G*Power program. The necessary sample size considering an alpha = .05, a Cohen's d = .8 (large magnitude for the effect size), and power = .95, is 42 participants in each condition, that is, a total of 84 participants. Assuming a loss of 20%, n(1/1–R), the estimated final sample is made up of 105 participants, approximately 53 participants in each condition.
The inclusion criteria are a) being between 12 and 18 years old, b) providing signed informed consent (from the adolescent and their legal guardian), c) being able to understand and read Spanish, and d) showing moderate levels of depressive and anxiety symptoms according to the screening tools (Patient Health Questionnaire - PHQ-9 and the General Anxiety Disorder-7 - GAD-7).
The exclusion criteria are a) having been diagnosed with a mental disorder or alcohol and/or substance dependence disorder, b) the presence of high suicidal risk, c) having a medical disease or condition that prevents the participant from participating in the psychological treatment, d) receiving another psychological treatment while the study is ongoing, e) increases and/or changes in participants' medication if they are receiving pharmacological treatment during the study, and f) not completing or improperly completing (e.g., acquiescence, random response) baseline or post assessments.
Instruments
An overview of the assessment measures is provided in Table 1. In order to analyze the socioemotional adjustment, a wide range of tools are included to assess sociodemographic, family, cognitive, emotional and behavioral, and contextual variables. Most of the assessment measures have been validated in Spanish-speaking adolescent samples. The design of this study leads to three assessment phases: a) screening of adolescents considered at-risk for emotional difficulties, b) pretest assessment, and c) post-test follow-up.
Table 1. Overview of the Assessment Measures at Pre, Post and Follow-ups.
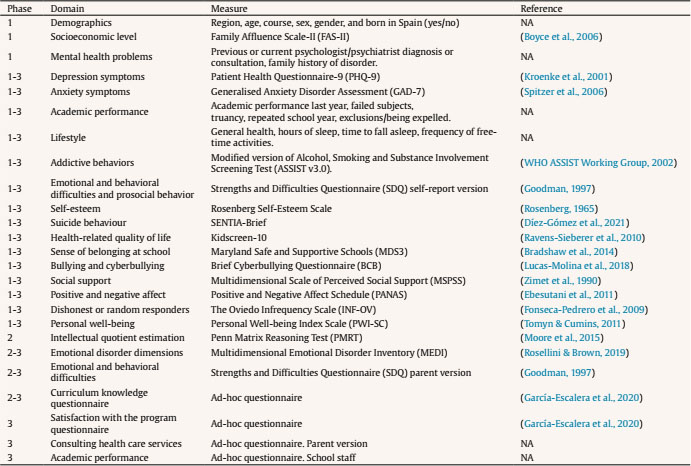
Note.NA = not applicable; Phases: 1 = screening, 2 = pre-test assessment, 3 = post-test assessment.
Screening phase. The instruments are administered collectively via personal computers in classrooms for between 10 and 30 students during a standard one-hour session in specially prepared rooms. Participants are selected using widely known instruments to screen subthreshold emotional symptomatology in adolescent samples. The administration of the different tests is adjusted to 50 min. (1 school hour).
Pre-test assessment. Adolescents at risk of emotional disorders with a moderate score in both the PHQ-9 and GAD-7 are selected (between 10 and 15 points). In this phase, a test for intelligence (IQ) and the Multidimensional Emotional Disorder Inventory are administered. In addition, the Strengths and Difficulties Questionnaire (SDQ) parent version is used for the families.
Post-test and follow-up. Various post-test assessments at 6, 12, and 18 months are performed. The screening phase and pre-test phase tools are used. In addition, this phase includes an assessment of knowledge test, a satisfaction test, and a parent test.
Intervention
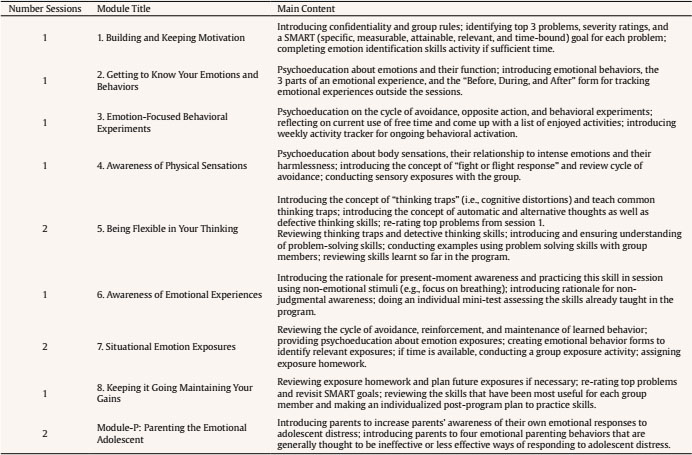
Intervention Program for the Experimental Group
The treatment will be applied to the group randomly selected as the experimental group. Groups of approximately 8-12 participants will be created. The intervention will take place in the school. All participants will be given a copy of the Spanish UP-A Manual for patients (Ehrenreich-May et al., 2018; Ehrenreich-May et al., 2020). An adaptation of the UP-A will be made to ensure its administration in educational contexts, and for adolescents with emotional symptoms rather than with emotional disorders in clinical settings. This adapted version of the UP-A will be delivered in 10 sessions (see Table 2). The sessions are structured as follows: a) review of challenges for homework 10 min.; b) module contents 35 min; and c) explanation of challenges for homework 5 min. The Parenting the Emotional Adolescent module will be implemented in this preventive adaptation of the UP-A. Being given the specific instructions for the family in the UP-A manual, families will be provided with summaries of each module, as well as a activities calendar that their children will be doing, so that they are aware of them.
Table 2. Overview of the UP-A adapted for Preventive Intervention on PSICE Project (adapted and modified from Ehrenreich-May et al., 2018; García-Escalera et al., 2017).
Intervention Program for the Active Control Group
The randomly selected control group will complete a Jacobson Progressive Relaxation Training Program (see the method section for justification) according to the procedure by Bernstein and Borkovec (1973). Progressive relaxation is a well-known procedure consisting of a deep muscle relaxation based on the principle that the muscle tension is the body's psychological response to anxiety-provoking thoughts. There will be 10 sessions, each lasting approximately 50 minutes. A manual developed specifically for the PSICE project will be used (Fonseca-Pedrero, 2022).
Unified Protocol for Transdiagnostic Treatment for Adolescents with Emotional Symptoms Implementation
First, the psychologist who will implement the UP-A will receive training using the Spanish UP-A Manual Therapist Guide (Ehrenreich-May et al., 2022). Training will also be delivered to the professionals who will apply progressive relaxation techniques to the active control group. To determine the feasibility of training in the UP-A, 10-20 school psychologists with more than 2 years of professional experience will be trained. The authors of the Spanish UP-A will teach a course consisting of ten-hour sessions. The first session will present the characteristics of the UP-A and the objectives, content, and techniques of each intervention module. The remaining two sessions will provide training in different therapeutic skills that facilitate change through role-playing, following the foundations of evidence-based psychology and deliberate practice. The level of learning achieved in the UP-A will be assessed through performance in the role-plays. School psychologists will conduct the intervention sessions under the supervision of an expert psychologist who will coordinate the psychologists' team throughout the study and across schools. Psychologists' fidelity and adherence to the treatment protocol will be regularly evaluated by means of an ad hoc questionnaire developed by the authors of the Spanish adaptation of the program.
Design of the Evaluation
To evaluate the results of the effectiveness of the UP-A intervention, multi-informant measures (self-report and hetero-report) will be taken. The outcomes will be evaluated by measures of anxiety and depression symptomatology, functionality, and transdiagnostic variables. Other outcomes will also be examined by measures of emotional, cognitive, social, family, and academic adjustment. Main outcome measures are:
Change in the Patient Health Questionnaire-9 (PHQ-9) scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in the Generalized Anxiety Disorder Assessment (GAD-7) scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in the Strengths and Difficulties Questionnaire (SDQ) scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in the Kidscreeen-10 scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in the Positive and Negative Affect Schedule-Brief child (PANAS) scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in Multidimensional Emotional Disorders Inventory (MEDI) scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in SENTIA-brief scores between pre- and post-intervention and at 6-, 12-, and 18-month follow-ups.
Change in school achievement scores and related indicators between pre- and post-intervention and at 6-, 12-, and 18-months follow-ups.
Data Analysis
Data will be analyzed using the linear mixed-models (LMMs; MIXED) procedure with full-information maximum likelihood estimation. To estimate the effect between all the model variables taken together, Wilks lambda will be used. The partial eta squared statistic (ηp2) will be used to calculate effect size and to determine the practical significance of the results. In cases considered appropriate, gender, age, socioeconomic level, and estimated IQ will be considered as covariates. To analyze the differential effect of possible predictors of treatment success, a logistic regression analysis will be performed. Analysis of the outcome evaluation (effectiveness assessments) will be conducted using an intention-to-treat approach, meaning all participants successfully completing the baseline and receiving the first intervention session will be included in subsequent analyses (Figure 1).
Discussion
Emotional symptoms and disorders in young people stand out as an educational and public health problem because of both their prevalence and associated co-morbidity, as well as the risk of personal, family, social, and health consequences extending into adulthood. More specifically, these problems can have a negative effect on academic performance and learning processes in the short, medium, and long term. Mental health is an integral component of health and well-being and influences academic, social, and economic outcomes across the lifespan. Adolescence is an essential stage of human development during which the roots of later adulthood are put down. Young people hold the key to creating a better future. Ignoring this issue could be considered almost unconstitutional, as it affects the basic human rights and quality of life of a significant section of the country's population. In addition, schools are one of the best settings for promoting and protecting mental health and psychosocial well-being during adolescence. This emerging educational, health, and social challenge needs to be addressed through evidence-based research and informed decisions.
In order to respond to these issues, we believe that using the UP-A, which has a treatment manual and is widely applicable to emotional disorders in adolescents, and assessing its effectiveness, will contribute to the evaluation and dissemination of school-based psychological interventions in Spain. The PSICE project aims to provide initial support for the effectiveness of manual-guided, transdiagnostic CBT preventive interventions for anxiety and depression in adolescents in regular school settings delivered by school psychologists. The central purpose is to reduce symptoms of anxiety and depression in adolescents as an indicated prevention, and at the same time, to improve adolescents' social-emotional adjustment, learning processes, and school achievement.
Emotional disorders and symptoms can be prevented with timely, evidence-based, and often low-cost interventions. For instance, two transdiagnostic CBT protocols have been developed and evaluated for young children: a) EMOTION: “Coping Kids” Managing Anxiety and Depression (Kendall et al., 2013) and b) Super Skills for Life (Essau & Ollendick, 2013). The efficacy of these transdiagnostic programs has been demonstrated at international (Essau et al., 2019; Loevaas et al., 2020) and at national levels (de la Torre-Luque et al., 2020; Fernández-Martínez et al., 2019, 2020). The UP-A is an emotion-focused, standardized, transdiagnostic CBT for adolescents (ages 12-17) with anxiety or depressive disorders (Ehrenreich-May et al., 2018). However, new studies are required in order to extend the evidence. For instance, in Spain the UP-A has not yet been applied as an indicated prevention program, with an active control group, medium-term follow-up testing, incorporating the module for families, or using large and representative samples of the population.
This evaluation design is subject to at least two limitations. First, given that the measures are self-reported, some potential bias in substance use estimations is expected. Nonetheless, self-reporting is deemed suitable and has been used in previous evaluations of prevention programs in schools. Second, the participating schools will not be randomized; instead, they will be selected from those currently delivering the intervention, limiting the generalizability of the results, but ensuring ecological validity.
The implementation of preventive, standardized, empirically supported psychological interventions such as the UP-A will allow proper management of school, social, economic and/or care resources and make them accessible to a large proportion of the population. In addition, the PSICE project will, among other things, help us to: a) better understand the etiological mechanisms and target modifiable vulnerability factors—from a dimensional, transdiagnostic, dynamic perspective—that underlye emotional problems during adolescence; b) demonstrate that prevention strategies are effective in a real-world school setting, at low cost in the educational context, with benefits on personal, family, school, social, and health levels; c) determine the importance and relevance of psychologists in schools; d) ensure that empirically supported psychological interventions, carried out by school psychologists, are accessible to the whole population; and e) provide a novel line of action within the framework of promoting emotional well-being and prevention of child and adolescent mental health problems to improve, optimize or enhance, mental health policies and learning processes in educational contexts.
To conclude, it should be noted that it is a constitutional duty to promote, protect, and look after the entire population's mental health, particularly, in children and adolescents. People deserve high-quality, accessible, inclusive, public psychological care that improves the quality of life for present and future generations. We all share responsibility and can play an important role in listening to and supporting our children and adolescents, helping them to build a good sense of belonging and a life worth living. It is time to act, generating hope through action.