Introduction
The psychological impact of infertility has been described based on both clinical observation and empirical research. Infertility can lead individuals and couples to have very high levels of multifaceted stress (Boivin et al., 2011; Cousineau & Domar, 2007; Donarelli et al., 2016) and depression (Verhaak et al., 2007). A systematic review (Conversano et al., 2010) including 23 studies concluded that protective factors for psychological adjustment during in vitro treatments included trait optimism, problem-focused coping, positive family/marital function, social support, situation appraisal involving acceptance of the situation, and secure attachment style.
Originally proposed by Carver and Scheier (2014), dispositional optimism can be defined as the global expectation that things will turn out well in the future and bad things will be scarce. This is particularly relevant to clinical psychology due to its protective role to reduce the risk of developing a psychopathology (Kleiman et al., 2017). Similarly, it seems to confer high resilience during stressful life events, and this resilience is negatively associated with both the onset and the recurrence of psychological distress (Cousins et al., 2014; Kleiman et al., 2017). Resilience, conceptualized as the capacity and dynamic process of adaptively overcoming uncertainty, conflict, and adversity while maintaining normal psychological and physical functioning, is a necessary factor during stressful situations related to maternity (Garcia-Leon et al., 2019).
More precisely, it can be defined as the belief that a person can control the way one copes with adversity. It is one of the strongest buffers against mental health problems (Mancini & Bonanno, 2009). Resilience may be critical in determining how individuals cope with and adapt to stress (Chrzan-Detkos et al., 2022; Johnson et al., 2017).
Psychological stress arises from connections between individuals and their environment that are felt that exceed their adaptive capacities and threaten their wellbeing (Caparros-Gonzalez et al., 2022; Cohen et al., 2007). In the context of infertility, women can experience high levels of stress (Rooney & Domar, 2018). Unsuccessful attempts during assisted reproductive technology (ART) can be associated with infertility-specific stress, which refers to a type of psychological stress related to the sense of loss, failure, and shame in women diagnosed with infertility (Patel et al., 2016). Infertility-specific stress can progress to depression and anxiety (Rockliff et al., 2014). Infertility-specific stress comprises different dimensions, namely, concerns related to the need of parenthood, concerns associated with rejections of a childless future (Bielawska-Batorowicz, 2022), perceived social concerns, and concerns regarding the impact of infertility on the couple relationship (Zurlo et al., 2020). All these dimensions fostered the development of further research aiming at identifying protective factors potentially reducing perceived distress among infertile couples (Donkor & Sandall, 2007). A previous study informed that resilience was a potential protective factor for a couple's quality of life and that could reduce infertility-specific stress among women undergoing ART (Herrmann et al., 2011).
As the prevalence of women undergoing infertility continues to increase worldwide, given the scientific plausibility that psychological stress can affect the success of fertility treatments and current recommendations regarding maternal mental health (Chrzan-Dtko et al., 2022), there is a need to update and re-examine available research (Caparros-Gonzalez et al., 2019). In this context, it is necessary to explore the potential role of mediators that could buffer the consequences of high levels of stress and anxiety during ART procedures (Romano et al., 2012).
The aim of this study was to examine the mediating role of resilience and optimism on stress and anxiety in women undergoing assisted reproductive technologies (ART) in a private fertility clinic.
Method
Participants Using Assisted Reproductive Technology
The study was conducted in a sample of 229 women presenting an infertility diagnosis who were following medical treatment for infertility. Participants were recruited from the city of Madrid (Spain).
Eligibility criteria included: 1) women over 18 years old, 2) first visit to the fertility clinic, 3) currently trying to get pregnant with a male partner, and 4) proficiency in Spanish language. Women with a history of mental health disorder (psychopathological disorders such as depression and/or anxiety before diagnose) were excluded.
Aiming to obtain satisfactory results, a priori sample size requirements according to G*Power Statistical software was established at a minimum sample size of 178 to acquire an adequate power of .80 and using an α = .05. G*Power statistical software is a powerful tool to calculate statistical power analyses, effect size, and sample size requirements for a variety of tests (Faul et al., 2009). A sample size requirement of n = 175 was calculated to achieve a large effect size in the a-path and a medium effect in the b-path (Fritz & Mackinnon, 2007).
A total of 300 potential participants aimed to collaborate in this study. After excluding patients whose ART treatment was not completed (n = 23), those having a spontaneous pregnancy before starting the treatment (n = 4), and women reporting lack of time (n = 44), the total sample size encompassed 229 women undergoing an ART treatment.
Procedure to Study Infertility-Specific Stress
The Ethics Research Committee of the Institution (IVI-RMA) approved this study. This study followed the principles of the Declaration of Helsinki (AMM, 2008) and the Good Clinical Practice Directive (Directive 2005/28/EC) provided by the European Union. Participants were invited to participate prior their initial appointment with a reproductive endocrinologist at a university affiliated private infertility clinic between January and December 2018.
Participants were informed about the study aims. Participation was voluntary and anonymous. Those women willing to participate read and signed an informed consent form. Afterwards, participants were asked to fill up the psychological measures before their initial appointment with a reproductive endocrinologist at a university affiliated private infertility. Sociodemographic and medical data (including obstetrical variables) was also obtained (age, educational level, treatment, ART treatment, diagnosis of infertility, and number of previous children). Medical data were obtained from a participant's medical records.
The STROBE Statement for reporting cross-sectional studies was followed in the present study (Elm et al., 2007).
Psychological Assessment of Perinatal Stress
The psychological self-report measures used in this study were applied to assess optimism, pessimism, resilience, perceived stress, state anxiety, and trait anxiety. In order to obtain this information, the following psychological self-report measures were applied:
Resilience Scale (RS; Wagnild & Young, 1993; Spanish version by Rodríguez et al., 2009)
This scale was used to assess the capacity to withstand life stressors, and to thrive and make meaning from challenges. This scale comprises a 17-items subscale named Personal Competence and a 8-items subscale named Acceptance of Self and Life. Resilience as described by Wagnild include 5 essential characteristics related with a meaningful life: purpose, perseverance, self-reliance, equanimity, and existential aloneness (i.e. coming home by yourself). Cronbach's alpha reliability coefficient of the Spanish version is α = .79. Cronbach's alpha reliability coefficient of the current sample was α = .81. According to the original version of this measure, a higher score suggests high levels of resilience (Wagnild & Young, 1993).
Life Orientation Test Revised (LOT-R; Scheier et al., 1994)
Dimensions of optimism and pessimism were evaluated using the 10-item Spanish version (Ferrando et al., 2002) This is a self-report questionnaire to assess an individual tendency to expect positive compared to negative outcomes. Items are scored on a 5-point Likert scale and summed to produce a total score. The measure also offers information on optimism and pessimism with two subscale scores. The LOT total score consists of 8 items and reflects a single bipolar dimension in which higher scores indicate greater optimism or less pessimism. Cronbach's alpha reliability coefficient of the Spanish version is α = .72. Cronbach's alpha reliability coefficient of the current sample was α = .73.
STAI (Spielberger, 1983; Spanish version by Buela-Casal & Guillén-Riquelme, 2017)
This inventory was used to measure state and trait anxiety. The STAI consists of two subscales with 20 items each. The State Anxiety Scale (STAI-S) was used to assess the current state of anxiety and offers information on how respondents feel in that moment. Items reflect feelings of tension, worry, apprehension, nervousness, and activation/arousal of the autonomic nervous system. The Trait Anxiety Scale (STAI-T) was used to measure relatively steady aspects of anxiety proneness, including general states of calmness, confidence and security. All items were rated on a 4-point Likert scale (0 = almost never to 3 = almost always). Higher scores indicate greater anxiety. Cronbach's alpha reliability coefficient of the Spanish version is α = .93. Cronbach's alpha reliability coefficient of the current sample was α = .84 for STAI-S and .82 for STAI-T.
Perceived Stress Scale (PSS)
This is a 14-item self-report questionnaire. This measure was used to assess the perception of general stress during the last month. The items are scored on a 5-point Likert scale (0 = never to 4 = very often). An overall score of 20 is considered moderately high. In this study we used the Spanish version (Cohen, 1983; Remor, 2006), which has a Cronbach's alpha reliability coefficient of α = .82. Cronbach's alpha reliability coefficient of the current sample was α = .75.
Statistical Analysis
Statistical analysis was conducted using Social Package for Social Sciences SPSS Statistics Software (v.22; IBM SPSS Statistics). There were no missing data. Pearson's correlation coefficients were used to study potential associations between study variables and age. Two mediation analyses were performed. The first tested whether the relationship between stress and symptoms of anxiety was mediated by resilience.
Structural equation modelling (SEM modelling) was used to test whether the relationship between stress and symptoms of anxiety was mediated by optimism. The mediating effect of resilience in the relationship between stress and symptoms of anxiety and stress while controlling for age was tested. SEM was used to fit a single model for each of the two relationships to estimate the indirect, direct, and total effects. A significant mediating effect was established when the 95% bias-corrected bootstrap confidence interval based on 1,000 bootstrap samples did not contain zero (McKinnon et al., 2004; Sobel, 1986).
In moderation analyses two series of nested models in multiple linear regression analyses were conducted in four steps. In step 1, age was entered. In step 2, three separate analyses were conducted in which stress and resilience were entered separately to ascertain their individual explained variance, and then altogether to test the compensatory model while the interaction (stress by resilience) term was entered in step 3 to test the protective model. Symptoms of anxiety was the outcome variable. Both stress and resilience variables (all continuous) were centered (Frazier et al., 2004) before they were entered in the analyses to test the interactional effect.
Results
Sample Characteristics
Women in this sample had an age ranging from 18 to 45 years (M = 36.83 years, SD = 0.26), with a history of infertility ranging from 6 to 60 months (M = 19.82, SD = 0.89). Participants in this sample had a range of diagnosis associated with infertility. In this respect, an amount of 65 women (28.38%) was diagnosed of advanced maternal age (> 40 years old), n = 45 women (19.21%) had a low ovarian reserve, n = 26 (11.79%) endometriosis, n = 15 (6.99%) suffered from an immunological disease (Hashimoto's disease, rheumatoid arthritis, antiphospholipid syndrome), n = 19 (8.30%) had recurrent miscarriages, n = 36 (15.72%) had a male factor, and n = 23 (9.61%) were diagnosed from idiopathic infertility. Participants' clinical characteristics are presented in Table 1, including levels of resilience and optimism depending on the level of education.
Table 1. Sociodemographic Data, Obstetric History, and Psychological Measures (N = 229).

Note.IVF/ICSI = in vitro fertilization with intracytoplasmic injection; IVF/PGD = in vitro fertilization with preimplantation genetic diagnosis; OD = oocyte donation; IUI = intra uterine insemination; AMA = advanced maternal age; LOR = low ovarian reserve
Test of the Mediation Model
Correlation analysis between the psychological measures showed that state and trait anxiety were significantly associated with optimism (r = .037, p = .05, and r = .031, p = .05, respectively). Our results indicated a significant negative correlation between perceived stress and resilience (r = -.320, p = .001). Perceived stress was significantly associated with state and trait anxiety (r = .560, p = .001 and r = .220, p = .001). Resilience was significantly and negatively correlated with state anxiety (r = -.210, p = .001) and moderately (positive or negative) associated with trait anxiety (r = .160, p = .05). Table 2 presents mean values, standard deviations and Pearson's correlations between age and the psychological measures (LOT-R, RS, STAI-S, STAI-T, PSS).
Table 2. Mean Values, Standard Deviations, and Pearson's Correlations between Age and Psychological Measures.
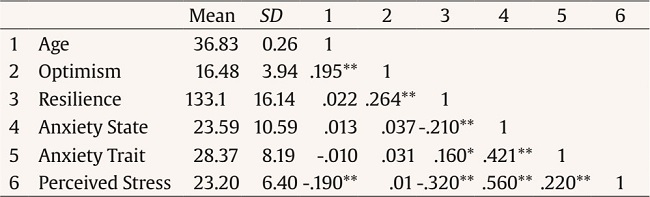
*p < .05,
**p < .001.
Two mediation analysis were performed using SEM modelling. Firstly, it was tested whether the relationship between stress and symptoms of anxiety was mediated by resilience. Secondly, it was tested whether the relationship between stress and symptoms of anxiety was mediated by optimism. The estimated of 95% bias-corrected bootstrap CI and results summary for the relationship between stress and symptoms of anxiety mediated by resilience are presented on Table 3 and Figure 1.
Table 3. The Mediating Effects of Resilience in the Relationship between Stress and Symptoms of Anxiety (N = 229).
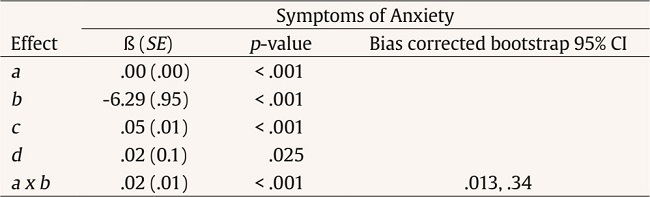
Note.B = Unstandardized path coefficient; SE = standard error; CI = confidence interval; a = effects of stress on resilience; b = effects of resilience on symptoms of anxiety after adjusting for stress; c = total effects of stress on symptoms of anxiety; d = direct effects of stress on symptoms of anxiety; a x b = mediating effects of resilience in the relationship between stress and symptoms of anxiety (i.e., the indirect effects of stress through resilience).

Figure 1. Mediating effects of resilience in the relationship between stress and symptoms of anxiety (N = 229).
There was a significant indirect effect of stress on symptoms of anxiety through resilience (β = -6.29, p < .001, 95% CI [.16, .10]). Resilience partially mediated the relationship between stress and anxiety symptoms (β = .02, p < .001, 95% CI [.34, .13]) as: (i) the direct effect was smaller than the total effect of stress on symptoms of anxiety and (ii) there was no zero in the 95% bias-corrected bootstrap confidence interval for the indirect effect.
No significant association was found between optimism and stress or anxiety.
Discussion
The aim of this study was to examine the mediating role of resilience and optimism on stress and anxiety in women undergoing assisted reproductive technologies (ART).
Among different personal characteristics, resilience, defined as a measure of stress coping ability, could be a key factor handling adversity. In this context, exploring the constructs of resilience and optimism in women dealing with the multifaceted infertility-stress was considered the core aim of the current study.
Our findings showed that resilience partially mediated the relationship between stress and anxiety symptoms. Regarding the relationship between anxiety symptoms and stress the results supported a compensatory model of resilience. These findings indicate differences in the stability of resilience across stress and anxiety symptoms. Resilience has also been found to partially mediate stressful events and affective symptoms in previous studies (Charney, 2004; Hjemdal et al., 2006; Masten & Wright, 2009). High resilience levels among involuntary childless women suggests a high level of psychological stability. These results go in line with previous studies (Greil et al., 2010; Herrmann et al. 2011). In this respect, a recent review found that both optimism and resilience were negatively associated with stress and anxiety during ART procedures (Santa-Cruz et al., 2019). Findings from the present study suggest a tendency of women with infertility to adjust and to adapt in face of adversities (Coughlan et al., 2014). As expected, perceived stress was positively associated with symptoms of anxiety. This is consistent with previous studies of anxiety (Donarelli et al., 2016).
When resilience was considered as a mediator it was found that higher levels of perceived stress were associated with lower levels of resilience, which in turn was positively associated with anxiety symptoms. We can argue that infertility patients with higher levels of anxiety symptoms may at least have low access to navigate through and negotiate stress, to overcome adverse outcomes. This may suggest that increased resilience among infertile women could decrease the effect from stress, thereby reducing the impact on anxiety symptoms. A previous study reported additional reduction of maternal stress through support from health care providers (Kovacheva et al., 2022). Resilience accounted for more than double of the variance in anxiety symptoms compared to optimism which shows that resilience seems to be more important in explaining anxiety symptoms than optimism. It is important to acknowledge that resilience is a relatively general measure which is built from composite factors such as tenacity (persistence in maintaining value), strength (being strong with setback), and optimism (positive thinking) (Johnson et al., 2017). These factors may contribute differently in emotion regulation in infertility. Considering the three composite factors, we hypothesize that resilience regulates negative emotions and anxiety through optimism, which may explain why resilience appeared as a mediator of distress but no optimism. Previous studies have showed correlations between optimism and reduced anxiety levels (Bleil et al., 2012; Brissette et al., 2002; Lancastle & Boivin, 2005).
In the present study anxiety was found to be associated with stress. More precisely, it was found that perceived stress has a positive and moderate association with state anxiety, while the association between perceived stress and trait anxiety was also positive but weak. Our study disagrees with a previous study reporting a strong association between stress and anxiety among infertile women (Foti et al., 2023). Nevertheless, none of these studies used infertile-specific stress measures.
This study presents some limitations. Thus, this is a cross sectional study using psychological measures. Participants were recruited from a private fertility clinic by convenience sampling, which may limit the representation. Participants had a variety of diagnosis and medical treatments related to fertility. Additional longitudinal and experimental research is required to determine whether optimism and resilience can contribute to healthier behaviors and whether optimism and resilience could be an effective target to foster in order to reduce distress and maladaptive dysfunction during ART. The use of infertility-specific stress measures could offer alternative findings (Patel et al., 2016). Regarding the mediating effect of resilience, the change was small. However, data gave us the right to apply for partial mediation. More studies would be necessary to support (or not) these findings.
To our knowledge, this is the first study to analyze potential interactions between perceived stress, anxiety, and resilience among women using ART. This cross-sectional study has showed evidence for both direct effects and interactional effects to support both the compensatory and protective models of resilience respectively. Future studies are required, especially in similar samples, with research designs and statistical models that will account for the shared aspects of symptoms of anxiety, and also include depressive symptoms.
Conclusions
This study contributed to a better understanding of the process linking resilience, optimism, anxiety, and psychological stress among women undergoing ART. High levels of resilience were found to be a potential protective factor for stress during ART processes. Resilience may be regarded as a latent and non-specific resource. Psychologists have a key role on promoting perinatal mental health among women (Caparros-Gonzalez et al., 2021). Women undergoing ART are exposed to high levels of stress and anxiety (Bailey et al., 2017). Reasons for these high levels of stress are associated with the high number of medical procedures (i.e. ultrasound, gynecological check-ups, hormonal treatments), and sometimes the lack of success and continual disappointments (Toftager et al., 2018).
Clinical implications of this study include the positive potential role of resilience as a buffer of stress and anxiety among women undergoing ART. This study highlights the protective role of resilience when women and confronted by the adverse effects of stress and anxiety during ART procedures. Psychological interventions to improve resilience and optimism should be addressed on women who are about to go through ART. Therefore, the potential utility of resilience to enhance the psychological health of women should be maximized.














